Modular Tapered Titanium Stems for Femoral Revision
Jacob T. Munro
Bassam A. Masri
Donald S. Garbuz
Clive P. Duncan
Case Example
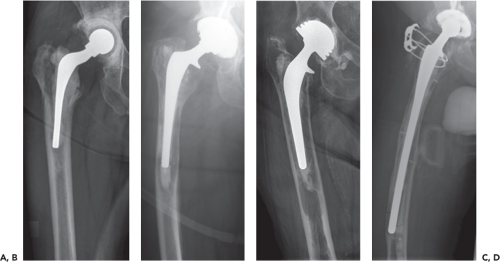
A 91-year-old woman presents to the emergency room with pain in the left thigh following a fall after tripping on loose carpet. She is unable to weight bear on the affected side and she had a cemented hip replacement performed 10 years ago. She has a history of hypertension controlled on medication and is an independent community ambulator, living in her own home and still driving. On physical examination she has pain with any attempt at motion of the left leg and there is neither shortening nor rotational deformity of the leg. AP and lateral x-rays show a displaced Vancouver type B2 fracture around a cemented stem (Fig. 120.1).
Introduction
Total hip arthroplasty (THA) is one of the most successful procedures in orthopedic surgery. Improvements in primary implants have expanded the indications and with an ageing population we will expect to see more procedures being performed in the coming decades (1,2). Unfortunately, regardless of technical and material improvements, implant failures will still occur. Currently, 50,000 revision THA procedures are performed in the United States annually, half of these involving revision of the femoral component (2,3).
As primary THA has developed so too have revision techniques. Surgeons have several options depending on bone deficiency, the age and comorbidity of the patient, and their own experience (4). Of particular interest are techniques that can be reliably used to manage severe femoral bone loss. Ideally, these should be robust and efficient, allowing restoration of leg length and stability, with long-term fixation and if possible, preservation or restoration of bone stock.
Cementless, cylindrical nonmodular cobalt–chromium stems have demonstrated excellent results in several centers (5,6,7). These rely on reaming the femur to a tube into which a stem of closely matched diameter is impacted. Friction holds the stem stable while bone ongrowth occurs. This approach is less successful when the bone available to contact the stem is insufficient to provide enough friction to prevent stem subsidence (8,9). Weeden and Paprosky showed excellent results using cylindrical stems in mild and moderate bone loss but a failure rate of 21% when used in severe bone loss (6,10).
In 1987, Wagner (11) published results for a tapered, fluted, grit-blasted, titanium stem. The key concept in this approach is to ream the remaining distal femur into a cone into which the tapered stem is wedged. This provides axial stability whereas longitudinal flutes provide rotational stability. These types of stems have increased in popularity as a reliable, reproducible means of managing severe femoral bone deficiency (10,12,13,14,15,16,17,18,19). It is essential to plan the surgery carefully and a number of critical steps must be executed accurately to optimize results.
The concepts pioneered by Wagner have been retained in modern tapered stems, that is, circular cross section, a gradual taper over the distal portion of the stem and longitudinal flutes. Modern systems have been modified to overcome potential drawbacks in the initial design with the addition of increased offset, modular heads and proximal bodies and higher taper angles (Fig. 120.2).
Manufacturing femoral implants using titanium has several advantages. With a lower elastic modulus than chrome-cobalt, stress transfer to bone is closer to physiologic conditions (20). This should reduce rates of thigh pain and stress shielding seen with porous-coated chrome-cobalt stems (6,19). This generally contrasts with reports of proximal bone stock restoration seen with titanium stems (2,3,14,15,21,22,23,24). The grit-blasted titanium surface has an excellent record of reliable ongrowth (4,24,25,26).
The original Wagner stem was nonmodular, with a limited offset, and was prone to subsidence and dislocation (5,6,7,27). This has been explained by a tendency to undersize the stem during the learning curve. Inexperience may lead to seating the implant at a level to correct leg length rather than the point at which axial stability is achieved in the femoral canal (8,9,23,28,29). By modifying the implant to a modular device with separate stem and body components of different lengths, the appropriate stem can be rigidly driven into the femur, before overall construct length and offset are established by selecting the appropriate body. Most modular systems also allow the version to be varied and fine-tuned with rotation of the body prior to engagement and locking.
The stem taper is critical to the success of the implant. With straight cylindrical designs, the stem is supported solely by friction between the implant surface and the bone until ongrowth occurs. A distal taper stem fitted into a conically reamed femur has the advantage of compression as the implant is axially loaded. This demonstrates superior initial
stability with axial load when compared to cylindrical stems (6,30). The original Wagner stem was manufactured with a 2-degree taper. This has been increased in most modern systems to 3 degrees or more to lower the risk of subsidence reported in early series. The degree of taper changes the relationship of stem length to diameter. For example, with a 2-degree taper the diameter of the stem increases by 1 mm for every 57 mm in length. For a 3.5-degree taper a 1-mm increase occurs over 46 mm of stem. Thus if the stem subsides, the larger taper will engage over a shorter distance. The length of the required contact zone has been variably reported. Originally, Wagner proposed that this needed to be at least 7 cm, preferably 10 cm (10,27). Others have used tapered stems in situations where there is less than 4 cm (10,11,19), but in these cases, success is dependent on the quality of bone, as well as the length of contact.
stability with axial load when compared to cylindrical stems (6,30). The original Wagner stem was manufactured with a 2-degree taper. This has been increased in most modern systems to 3 degrees or more to lower the risk of subsidence reported in early series. The degree of taper changes the relationship of stem length to diameter. For example, with a 2-degree taper the diameter of the stem increases by 1 mm for every 57 mm in length. For a 3.5-degree taper a 1-mm increase occurs over 46 mm of stem. Thus if the stem subsides, the larger taper will engage over a shorter distance. The length of the required contact zone has been variably reported. Originally, Wagner proposed that this needed to be at least 7 cm, preferably 10 cm (10,27). Others have used tapered stems in situations where there is less than 4 cm (10,11,19), but in these cases, success is dependent on the quality of bone, as well as the length of contact.
Longitudinal flutes confer considerable rotational stability (10,12,13,14,15,16,17,18,19,30) and increase the friction between the stem and the cortical bone. Different designs may alter the number and distribution of flutes but these are generally triangular with bone penetration ranging from 0.1 to 0.5 mm (Fig. 120.3). The circular cross section is necessary with nonmodular tapered designs so that bone contact in the area of primary fixation remains the same regardless of version of the stem. Modular systems allow alterations in stem geometry as the body component controls version. An anterior bevel (Fig. 120.2) at the distal end of the stem reduces the chance of stem perforation through the anterior cortex of the femur. The circular cross section may be flattened anteriorly and posteriorly (Fig. 120.3) reducing stem contact in the corresponding femoral diaphysis and potentially decreasing rotational stability. Some recently introduced designs have an anterior bow or angle to match the natural sagittal bow of the femur and further reduce the risk of perforation.
Indications and Surgical Considerations
The Paprosky classification (20,31) for femoral bone loss may be used to guide surgical treatment (Fig. 120.4). A femur with type I deficiency has minimal loss of metaphyseal
cancellous bone, often seen with fibrous ingrowth following a cementless primary stem. With type II defects, metaphyseal bone is deficient but the diaphysis is intact. Type III defects are characterized by severe metaphyseal loss with involvement of the diaphysis. These are classified as IIIA where there is greater than 4 cm of intact diaphyseal bone available for distal fixation, and IIIB when there is less than 4 cm. A femur with type IV deficiency has extensive diaphyseal damage with widening of the canal and a nonsupportive isthmus. Similarly, periprosthetic fractures of the femur can be reliably classified according to the Vancouver classification (6,19,32,33). Type B fractures occur about the stem and are subdivided into B1 where the implant is stable, B2 where the implant is loose but bone stock is maintained, and B3 where the implant is unstable but the bone stock is poor.
cancellous bone, often seen with fibrous ingrowth following a cementless primary stem. With type II defects, metaphyseal bone is deficient but the diaphysis is intact. Type III defects are characterized by severe metaphyseal loss with involvement of the diaphysis. These are classified as IIIA where there is greater than 4 cm of intact diaphyseal bone available for distal fixation, and IIIB when there is less than 4 cm. A femur with type IV deficiency has extensive diaphyseal damage with widening of the canal and a nonsupportive isthmus. Similarly, periprosthetic fractures of the femur can be reliably classified according to the Vancouver classification (6,19,32,33). Type B fractures occur about the stem and are subdivided into B1 where the implant is stable, B2 where the implant is loose but bone stock is maintained, and B3 where the implant is unstable but the bone stock is poor.
Tapered stems are indicated for revision of failed cemented and uncemented stems when the proximal metaphyseal bone is deficient. This includes Paprosky types II, IIIA, IIIB, and most type IV femoral deficiencies (10,13,31). They are ideally suited for cases where an extended trochanteric osteotomy (ETO) is utilized and are indicated in the management of Vancouver type B2 and B3 periprosthetic fractures (34




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree