Minimally Invasive Posterior Cervical Laminoforaminotomy
Laura A. Snyder
Richard G. Fessler
DEFINITION
Cervical radiculopathy is a neurologic condition characterized by dysfunction of a cervical spinal nerve, the roots of the nerve, or both.
It usually presents with unilateral pain that radiates from the neck to the arm and/or the hand.
There can be a combination of sensory loss, loss of motor function, and reflex changes in the affected nerve root distribution.
This chapter focuses on minimally invasive posterior cervical laminoforaminotomy as a surgical treatment option for patients with cervical radiculopathy.
ANATOMY
The external occipital protuberance (EOP) can be palpated in the midline of the skull. The superior nuchal line is the thickened ridge that extends laterally from the EOP (FIG 1A).
Beneath the skin and subcutaneous fat of the posterior cervical spine is located the superficial fascia (FIG 1B).
Deep to the superficial fascia, structures are anatomically compartmentalized by an organized deep fascia and several interfascial planes (FIG 2).
There are three principal deep fascial layers: a superficial, middle, and deep layer.
One layer is attached to the EOP, the superior nuchal line, the ligamentum nuchae, and the spinous processes of the cervical vertebrae.
It divides to surround the trapezius.
The deep layer of the deep cervical fascia is attached to the ligamentum nuchae in the midline.
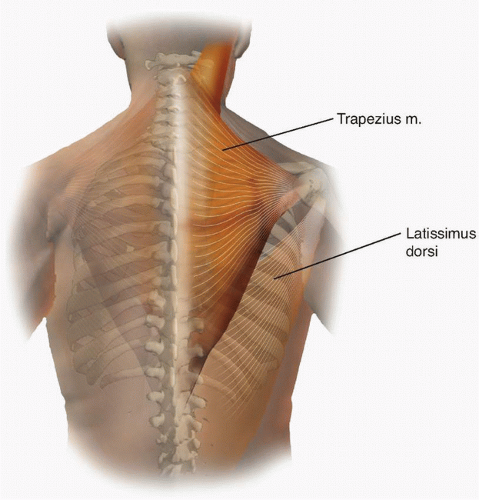
The most superficial muscle on the posterior aspect of the neck is the trapezius, which arises from the EOP and the medial part of the superior nuchal line of the occipital bone, the spinous processes of C7-T1 through T12, the supraspinal ligament, and the ligamentum nuchae (FIG 3).
The next muscle is the splenius capitis and arises from the ligamentum nuchae and spinous processes of C7 through T3 and inserts on the lateral portion of the superior nuchal line (see FIG 1B).
The erector spinae lie deep in the cervical region and include the iliocostalis cervicis, longissimus cervicis, the splenius cervicis, and the splenius capitis.
The deep layer of the deep cervical musculature includes the semispinalis cervicis and the semispinalis capitis (see FIG 1B).
The spinous process projects posteriorly from the junction of the laminae.
The lateral mass forms at the junction of the lamina and pedicle and gives rise to the superior and inferior articular processes or facets (FIG 4).
The superior facet at each level faces upward and posteriorly; the inferior facet faces downward and anteriorly.
A superior facet articulates with the corresponding inferior facet of the vertebral body cephalad to form the osseous elements of the zygapophyseal joints.
A vertebral notch is located on the superior and inferior aspect of each pedicle, such that adjacent notches contribute to the intervertebral foramen, through which the spinal nerve exits the spinal canal.
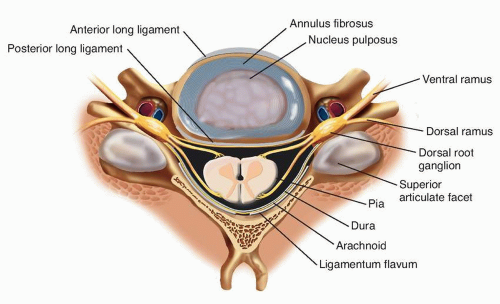
The foramen is bound superiorly and inferiorly by the pedicle; posteriorly by the facets; and anteriorly by the intervertebral discs, uncovertebral joints, and vertebral bodies (FIG 5).
The vertical diameter of the foramen is approximately 9 mm, the horizontal diameter is 4 mm, and the length ranges from 4 to 6 mm.
Foramina exit at an angle of 45 degrees from the midsagittal plane.
The spinal cord is cylindrical and slightly flattened in the anteroposterior (AP) direction, and thus usually has a larger transverse than AP diameter.
The spinal cord enlarges from C3 to C6 where it usually attains a maximal transverse diameter of 13 to 14 mm (FIG 6).
In the lower cervical spine, the anterior and posterior root entry zones are located approximately one disc level higher than the corresponding intervertebral foramen through which will pass the nerve root formed from its rootlets.
The rootlets pass obliquely laterally and caudally within the canal, entering the root sleeve where the sensory and motor roots are separated by the interradicular septum, a lateral extension of the dura mater.
Each dorsal root presents an oval enlargement, the spinal ganglion, as it approaches or enters the intervertebral foramen.
Just distal to this ganglion, the dorsal and ventral roots combine to form a spinal nerve.
The cervical nerve root occupies one-third of the foraminal space in a normal spine, usually the inferior aspect, with the superior aspect being filled with fat and associated veins.
The ventral (motor) roots emerge from the dura mater more caudally than the dorsal (sensory) roots, and the ventral roots course along the caudal border of the dorsal roots within the intervertebral foramina.
Thus, compression of the ventral roots, dorsal roots, or both depends on the anatomic structures around the nerve roots, such as a prolapsed disc (ventral root compression) or osteophytes from the facet joint (dorsal root compression).
The most likely site of compression of the radicular nerve is at the entrance zone of the intervertebral foramen because the medial entrance zone of the foramen is smaller in diameter than the lateral exit zone, whereas the nerve roots
are widest at their takeoff from the central thecal sac and become more narrow laterally.
Nerves C2-C7 exit above the correspondingly numbered vertebrae.
The C8 nerve root exits the intervertebral foramen formed between C7 and T1.
The dorsal root ganglion is usually located between the vertebral artery and the superior articular process.
In the sagittal plane, cervical nerve roots C3-C8 in the intervertebral foramina lie midway between the posterior midpoints of the lateral masses situated an average of 5.5 mm above or below each lateral mass point.
Thus, cervical nerve roots enter their intervertebral foramina and leave the spinal canal at the level of the disc and above the pedicle of the same numbered level, except for C8, which exits above the T1 pedicle.
The vertebral artery enters the transverse foramen of C6 and ascends through the transverse foramen to the level of the atlas.
In this region, it lies just in front of (ventral) to the ventral rami of cervical nerves C2-C6 and is surrounded by a venous plexus and sympathetic nerve fibers.
The transverse interforaminal distance and thus the transverse distance between vertebral arteries at the same cervical level increases slightly from C3 to C6.
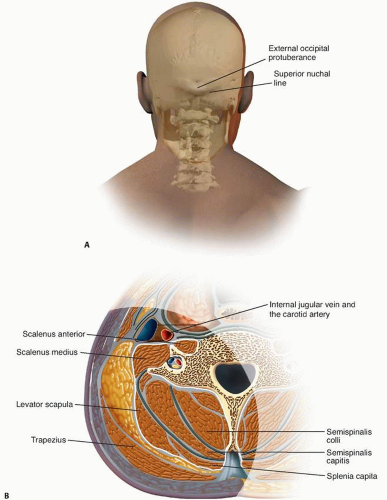 FIG 1 • A. Superficial anatomic landmarks of the posterior cervical spine. B. Cross-sectional anatomy of posterior cervical spine: superficial fascial layer (blue) and the muscles underneath. |
 FIG 2 • Cross-sectional anatomy of posterior cervical spine: deep fascial layer (blue) and the muscles underneath. |
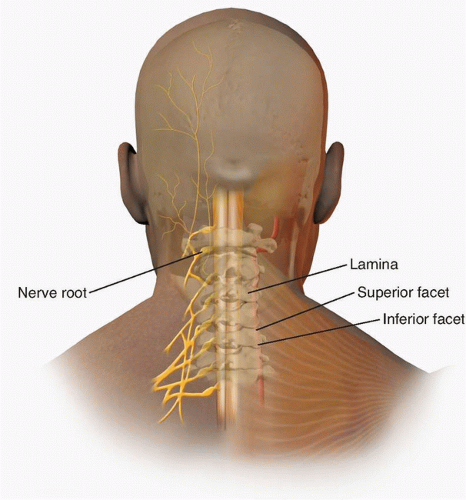 FIG 4 • Bone anatomy of the posterior cervical spine demonstrating the relationships of the superior and inferior facets, the lamina, and the exiting nerve roots. |
 FIG 5 • Lateral view of cervical spine depicting exiting nerve roots and vertebral artery within the region of the neural foramen. |
PATHOGENESIS
The most common cause of cervical radiculopathy is foraminal compression of the spinal nerve.
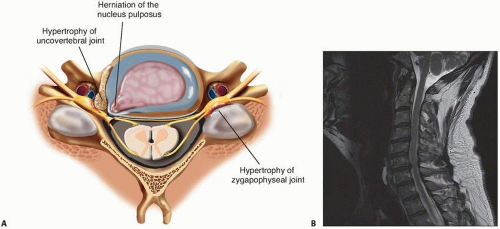
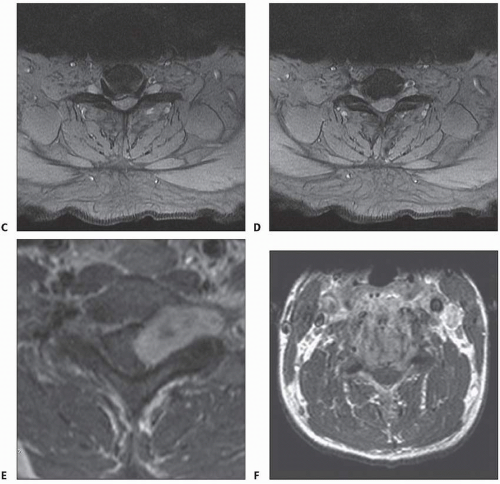
Contributing factors include disc herniations and bulges, decreased disc height, degenerative changes of the uncovertebral joints anteriorly, and the zygapophyseal joints posteriorly (FIG 7A-D).
Other rare causes include tumor and spinal infections (FIG 7E,F).
Normal disc itself does not contain nociceptive nerve fibers and is insensitive to pain.
When the nucleus pulposus ruptures through the annulus fibrosus, there is little or no localized pain until nociceptive fibers of the sinuvertebral nerves in the lateral posterior ligament and the dura of the nerve root sleeves are stimulated.
This stimulation generates localized back and neck pain.
In cases of cervical spondylosis, vertebral bodies subside and lose height, the ligamentum flavum and facet joint capsule tend to fold, which further decreases foraminal dimensions.
Some have postulated that nerve root compression by itself does not always lead to pain and note that the dorsal root ganglion must also be compressed.7
Mechanical distortion of the nerve root leads to a cascade of events in the microenvironment of the nerve.
Hypoxia of the nerve root and dorsal ganglion can aggravate the effect of compression.
Evidence indicates that inflammatory mediators—including matrix metalloproteinases, prostaglandin E, interleukin-6, substance P, and nitric oxide—are released by herniated cervical intervertebral discs.
These observations underlie the reason that anti-inflammatory agents often suffice to treat the radicular pain.
NATURAL HISTORY
Cervical radiculopathy occurs annually in 85 out of 100,000 people.
It is estimated that 75% to 90% of patients with acute cervical radiculopathy due to disc herniation will improve without surgery.
In a 1994 population-based study from Rochester, Minnesota, 26% of patients with cervical radiculopathy underwent surgery within 3 months of the diagnosis (typically for the combination of radicular pain, sensory loss, and muscle weakness), whereas the remainder were treated medically.
Recurrence, defined as the reappearance of symptoms of radiculopathy after a symptom-free interval of at least 6 months, occurred in 32% of patients during a median follow-up of 4.9 years. At the last follow-up, 90% of the nonoperated patients had normal findings or were only mildly incapacitated owing to cervical radiculopathy.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with cervical radiculopathy exhibit the hallmark symptoms of unilateral neck and/or arm pain, sensory disturbances, and possibly motor deficits (Table 1).
Central to the patient’s history are descriptors that include location, onset, duration, severity, associated symptoms, and triggers.
Pain is most prominent in acute cervical radiculopathy and it may be described as sharp, electric, achy, or burning.
It can be located in the neck, shoulder, arm, or chest, depending on the nerve root involved.
Classically, an acute radiculopathy presents with pain radiating in a myotomal distribution.
Sensory symptoms, predominantly paresthesias and numbness, are more common than motor loss and diminished reflexes.
The clinician should keep in mind that the sensory symptoms frequently do not follow classic dermatomal patterns as there is normal anatomic variation from individual to individual (FIG 8).
For patients with acute cervical radiculopathy, arm pain is present in nearly 100%, sensory deficits in 85%, neck pain in 79%, reflex deficits in 71%, motor deficits in 68%, scapular pain in 52%, anterior chest pain in 17%, headaches in 9%, anterior chest and arm pain in 5%, and left-sided chest and arm pain in 1%.
Radicular pain is often accentuated by maneuvers that stretch the involved nerve root, such as coughing, sneezing, Valsalva, and certain cervical movements and positions.
The Spurling test is performed by maximally extending and rotating the neck toward the involved side (FIG 9).
When positive, this test is particularly useful in differentiating cervical radiculopathy from other etiologies of upper extremity pain, such as peripheral nerve entrapment disorders, because the maneuver stresses only the structures within the cervical spine.
It is important to note that the physical examination can be normal.
The presence of “red flags” in the patient’s history (including fever, chills, unexplained weight loss, unremitting night pain, previous cancer, immunosuppression, or intravenous drug use) should alert clinicians to the possibility of more serious disease such as tumor or infection.
Table 1 Distribution of Cervical Disc Herniations and Anatomic Correlates | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain Films
Plain films offer the advantage of showing the spinal column in a weight-bearing state.
Degenerative changes on plain radiographs become more prevalent as individuals age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree