Fig. 4.1
Hamstring muscular complex located in the posterior thigh. Muscles of the complex include: the semimembranosus, semitendinosus, and the biceps femoris
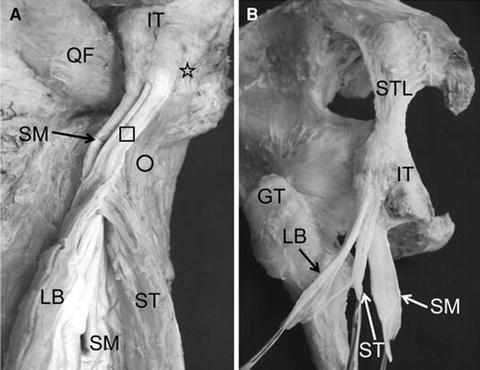
Fig. 4.2
(a) The origin of the long head of the biceps femoris and the semitendinosus (posterior, left-sided view of the left thigh). The long head of the biceps femoris originated from the posteromedial surface of the ischial tuberosity as a thick tendinous part (square), and the semitendinosus tightly adjoined the medial surface of the tendon of the long head of the biceps femoris as a muscular part (circle) and partly originated from the ischial tuberosity as a short and thin tendinous part medial to the tendon of the long head (star). (b) After removal of the muscular parts, the tendons of the hamstring muscles were observed. The semitendinosus muscle had a short and thin tendon which originated directly from the ischial tuberosity. GT greater trochanter, IT ischial tuberosity, LB long head of the biceps femoris, QF quadratus femoris, SM semimembranosus, ST semitendinosus, STL sacrotuberous ligament. With kind permission from Springer Science + Business Media: Journal of Orthopaedic Science, Anatomical study of the proximal origin of hamstring muscles, 17(5), 2012, Kengo Sato
The biceps femoris muscle is comprised of a long head and a short head, which additionally contribute to externally rotate the hip. Despite sharing a common insertion point on the lateral side of the fibular head, the short head differs slightly from the long head and other hamstring muscles in that it originates from the lateral lip of the linea aspera, located on the lateral supracondylar line of the femur [1, 2]. Further, the short head is innervated by the common peroneal division of the sciatic nerve (L5-S2), whereas the long head, semimembranosus and semitendinosus muscles are innervated by the tibial division of the sciatic nerve [1]. The semimembranosus and semitendinosus muscles additionally act to medially rotate the knee. After descending medially along the posterior thigh, the semimembranosus tendon divides into three main divisions: the oblique popliteal expansion, the anterior expansion, and the inferior expansion. Benninger et al. [3] found that the oblique popliteal ligament consists solely of a branch of the semimembranosus tendon and thus should be referred to as a tendon, not a ligament, as is commonly done. This branch spans across the popliteal fossa and inserts into the posterior capsule. The anterior division of the semimembranosus tendon extends its fibers to insert at the medial meniscus and medial collateral ligament [3]. The inferior division inserts at the posterior part of the medial condyle of the tibia [2, 3]. The semitendinosus muscle inserts along the superior part of the medial surface of the tibia, where it joins the tendons of the sartorius and gracilis muscles to form what is collectively called the pes anserinus. All muscles of the hamstring receive their blood supply from the perforating branch of the deep artery of the thigh and the superior muscular branches of the popliteal artery [1].
Hamstring anatomy is of clinical importance in injury assessment. The hamstring muscle complex is primarily used to decelerate while running, walking, or athletic motions such as sharp changes in the direction of motion at high speeds [4]. Through eccentric muscle contraction, these muscles serve to slow the lower limb during forward swing. Since the complex spans two joints, the hip and the knee, injury to any of the hamstring muscles can present with a wide range of symptoms [2].
Demographics and Risk Factors
Although injury to any of the muscles involved in the hamstring muscular complex can result from multiple complex interactions, modifiable and non-modifiable risk factors have been identified. Modifiable risk factors leading to hamstring injury include inadequate warm-up, increasing training volume, muscle fatigue, hamstring inflexibility and weakness, cross-pelvic posture, lumbar-pelvic weakness, and poor biomechanics during movement [5–11]. Risk factors that cannot be modified are seen in athletes of older age, a history of previous lower extremity injury, and may even be more common in African or Aboriginal ethnic backgrounds [8, 11–15].
Although the overall incidence of hamstring injuries in the general population is not known, athletes involved in competitive sports requiring sprinting and jumping are at particular risk. Bennell and Crossley reported a 14 % overall incidence of hamstring strains in track and field athletes [12], while Woods et al. reported that hamstring strains comprised 12 % of the total injuries in English professional soccer players over a two-season period [13]. Of these injuries, 53 % were found to involve the biceps femoris. Additionally, players of black ethnic origin and older age groups (23 or older) were found to have a significantly increased risk for hamstring strains.
Risk factors thought to be associated with hamstring strains include: history of previous hamstring injury, hamstring tightness, muscle fatigue, muscular strength imbalance, and insufficient warm-up. Orchard et al. followed 37 professional Australian rules football players and found a significant association between hamstring injury and both absolute hamstring weakness as well as a low hamstring-to-quadriceps muscle peak ratio [14]. However, the same study did not find a correlation between flexibility (tightness) and risk of injury. Although no data exist regarding the protective role of warm-up programs in relation to hamstring injuries specifically, one biomechanical study found that isometrically preconditioned muscles, similar to muscles subject to a warm-up period in athletes, required significantly more force to fail than non-preconditioned controls [15].
Mechanism of Injury and Grading Scale
In broad terms, the different types of hamstring injuries include: lacerations, contusions, delayed-onset muscle soreness, and strains. Muscle strains are the most common type of hamstring injuries and are the focus of this chapter. Hamstring strains occur most commonly at the musculotendinous junction of the hamstring musculature and are often a result of eccentric contractions [16]. Hip flexion combined with knee extension forces the hamstring musculature into maximum stretch which increases the risk for injury. Most injuries are noncontact and a high percentage occur during running. In their study, Woods et al. reported 91 % of hamstring injuries were noncontact while 57 % of them occurred while running [13].
Grading of hamstring injury has been based on the amount of muscle torn, clinical symptoms, range of motion at the knee, and magnetic resonance imaging (MRI). Zarins and Ciullo [17] described three grades of hamstring tear with grade II or partial tear being the most common (Table 4.1).
Table 4.1
Clinical grades of hamstring strainsa
Grade I | Mild injury with a tear of “a few muscle fibers” from overstretching of muscle |
Grade II | Partial tear of muscle |
Grade III | Complete tear of muscle |
Malliaropoulos et al. [18] described a classification scheme the clinical severity of acute hamstring stains that relates the loss of active range of motion of the knee to the severity of injury (Table 4.2).
Table 4.2
Clinical grades of hamstring strainsa
Grade I | <10° deficit |
Grade II | 10–19° deficit |
Grade III | 20–29° deficit |
Grade IV | ≥30° deficit |
In addition to clinical classifications, radiologic grading schemes for hamstring strains (Table 4.3) have been developed by Shelly et al. [19].
Table 4.3
Radiographic grades of hamstring strainsa
Grade I | T2 hyperintense signal about a tendon or muscle without fiber disruption |
Grade II | T2 hyperintense signal with fiber disruption of less than 50 % the width of the tendon or muscle |
Grade III | Tendon or muscle disruption of greater than 50 % of the width of tendon or muscle |
An MRI study of 516 hamstring injuries in professional European soccer players from 23 teams examined the correlation of severity of hamstring injury grade on MRI to days of play/practice lost [20]. The number of days missed as a result of MRI grades 0, I, II, and III injuries was 8 ± 3, 17 ± 10, 22 ± 11, and 73 ± 60 days, respectively. The biceps femoris was noted to be injured 83 % of the time while the semimembranosus and semitendinosus were injured 11 and 5 % of the time. As expected, the severity of MRI findings correlated with days lost. As the quality of MRI improves, the classification of these injuries is expected to be better understood.
Clinical Presentation and Imaging
In most cases, athletes who suffer acute hamstring strains have a reliable clinical presentation (Fig. 4.3). They will often be seen grabbing their posterior thigh at the time of injury and be unable to continue performing their sport due to pain. They are likely to report pain isolated to the posterior thigh for a midsubstance injury with symptoms traveling more proximally for proximal injuries. Some athletes feel or hear an audible pop at the time of injury. On examination, posterior thigh ecchymosis may develop and weakness with resisted knee flexion may be evident. In some cases, there may be a palpable defect in the mid-thigh hamstring musculature.


Fig. 4.3
Clinical photo representative of a patient with a high-grade hamstring strain demonstrating posterior thigh ecchymosis. When present, the clinician should be suspicious of a high-grade hamstring strain
Often, the diagnosis of a hamstring strain can be made clinically and imaging is unnecessary but it can have some value in diagnosing hamstring injuries. MRI can be useful in cases where the diagnosis is unclear. Ultrasound is another imaging modality that has been used in the diagnosis of hamstring injuries. A recent study by Petersen et al. [21] found no correlation between ultrasound findings and time to return to play in elite soccer players. In addition, of players with a clinical diagnosis of an acute hamstring strain, only 61 % had sonographic findings. The vast majority of hamstring strains can be diagnosed without imaging and are routinely treated without surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







