Fig. 15.1
The Advance Medial Pivot (AMP) total knee arthroplasty is shown (Reprinted with permission from Microport)

Fig. 15.2
Satisfactory radiological results of an AMP TKA at 10 years follow up is shown
AMP Design Characteristics and Features
Restoration of Normal Knee Kinematics and Stability
For many decades it has been suggested that knee kinematics are controlled by a four-bar-link mechanism [2–4]. This mechanical link, with the cruciate ligaments acting as an almost rigid tensile element, describes a posterior “rollback” phenomenon demanding certain knee motions (the femur should roll back posteriorly in relation to the tibia). In the 1980s research confirmed that the knee is not controlled by the four-bar link, and does not “rollback”. Rather, the medial side of the knee is more stable (less compliant or more constrained), and the lateral side is more mobile (more compliant and less constrained). Therefore, in the normal human knee, the tibia pivots about the medial femoral articular surface in flexion [5–17]. Thus, the knee is modeled as a shallow ball-in-socket on the medial side and two discs articulating convex to convex on the lateral side. AMP design followed this model and the principle that the kinematics and stability of a total knee prosthesis should be as close as possible to those of a normal knee, so that the arthroplasty would function more like the normal knee. Thus AMP is designed with medial femoro-tibial articulation comprised of a shallow ball-in-socket (creating stability), and the lateral side is an accurate trough (allowing mobility) (Fig. 15.3). This design more effectively recreates the kinematics of a normal knee than other implants. Studies have demonstrated that, after TKA, medial tibia pivoting is replaced by A/P sliding and rotation. This can significantly increase wear and reduce range of motion. The benefits of a ball-in-socket (medial-pivot) design are that it is stable to anterior/posterior loads and highly conforming, creating a large contact area allowing for low contact stress. The rotation allowed by the arcuate lateral side allows rotational freedom and the combined medial and lateral articulations give stability while allowing rotational mobility [20].


Fig. 15.3
The ball in socket medial compartment of the AMP design is shown (Reprinted with permission from Microport)
Both static and dynamic knee joint stabilizers are responsible for knee joint stability (collateral ligaments, posterior capsule, anterior and posterior cruciate ligaments and medial compartment conformity). The stability and kinematics of the normal knee are created by the circular femoral condyles spinning in the cupped tibial surface on the medial side and rolling over the convex tibial surface on the lateral side. During TKA several stabilizing knee structures are sacrificed (e.g. meniscus, anterior cruciate ligament, tibial articular anatomic curvatures etc.). In order to ensure stability, surgeons attempt to equalize both the flexion and extension gaps, to balance the ligaments, and to achieve proper implant alignment and rotation. As a result, a reduction of TKA stability is often found. Conventional TKA designs (although designed to exhibit a posterior roll-back in flexion) often slide anteriorly (paradoxical slide forward) due to loss of stabilizing structures and tibiofemoral congruity. As the knee flexes past 20°, body weight and force vectors slide the femur forward on the tibia (Fig. 15.4). This is termed “paradoxical motion” because normal knees are thought to roll-back as they flex [19, 20]. The raised anterior lip of the AMP polyethylene insert, coupled with the constant radius of the femoral component, resists this paradoxical motion by providing complete medial antero-posterior conformity throughout range of motion (Fig. 15.5) [5, 6, 20, 27].



Fig. 15.4
The anterior roll back of the femoral component (paradoxical motion) is shown

Fig. 15.5
The design feature for anteroposterior stability is shown
Optimization of Range of Motion (ROM)
Clinical studies report that average flexion obtained after AMP TKA is 111°, while other authors report an average ROM from 115.4° to 123° after a primary TKA with the AMP TKA [28–30]. A multicenter study group compared the Range of Motion (ROM) data for the Medial-Pivot Implant with five contemporary knee designs (PROFIX®, LCS®, AXIOM®, NEXGEN® and ADVANTIM®). The data was collected at a 6-month and 1-year time period. Compared to the other five designs, the Medial-Pivot prosthesis delivers an average of 7.6° and 7.2° greater ROM at 6-months and 12-months respectively [31].
Improvement of Clinical Wear Rates
The ability of the AMP TKA to resist polyethylene wear has been verified in clinical studies. The polyethylene components are sterilized with ethylene oxide instead of gamma radiation. Previous studies have shown gamma radiation sterilization increases stiffness and decreases polyethylene toughness [25]. Synovial fluid was obtained 1 year after knee arthroplasty from 17 patients (22 knees). Polyethylene particles were isolated and analyzed from the synovial fluid surrounding two knee designs: a PS and an AMP. The shape, size and number of the particles were compared. Particles were smaller and rounder in the AMP implants as compared to those of PS implants, but the differences in size and shape were not significant. In contrast, the difference in the amount of particles was significant. The Medial-Pivot Knee generated fewer particles than the traditional designs [32]. In an unpublished comparable dimensional study of retrieved AMP liners and intact unused AMP liners, satisfactory wear patterns were found in the mid-term (Fig. 15.6a–c).
Fig. 15.6
Dimensional wear patterns of a AMP polyethylene retrieved insert at 7 years follow up: (a) the different dimensional sections studied, (b) mediolateral frontal sections studied, (c) satisfactory wear pattern of the retrieved insert compared to the intact one
Restoration of Patellofemoral Joint Kinematics
High complication rates (pain, maltracking, subluxation and fractures) from the patellofemoral joint of conventional TKA designs have been reported [33, 34]. It has been shown in recent cadaveric studies that the average anatomic trochlear groove is oriented 3.6° related to the mechanical axis with small individual variations [35]. The AMP Femoral Component trochlear groove is angled 3.6° to minimize strain in the lateral retinacular tissues. The trochlea is also long and deep. The lateral anterior flange rises 3–4 mm above the floor and provides resistance to lateral subluxation 9 (Fig. 15.7a–c).
Fig. 15.7
AMP patellofemoral articulation design features are shown: (a) the orientation of the trochlear groove, (b) the length of the groove, and (c) the rise of the lateral anterior flange are shown, (d) skyline radiograph showing a congruent patellofemoral joint (Reprinted with permission from Microport)
Preservation of Bone Stock for Primary and Revision TKA
AMP femoral bone cutting instrumentation is designed in order to preserve bone. Additionally, the AMP revision system is a bone preserving design because no box cut is needed (60–80 % less bone removal is required [36]. In a study by Glasgow et al. [36], 29 patients who underwent revision TKA were tested for stability, ROM, extensor lag, leg alignment and clinical scores. Results showed that the medial pivot design provides AP stability of a PS insert without a need for extra bone removal [36].
Early Clinical Outcome
In a series of 440 patients who underwent a staged bilateral total knee arthroplasty with 5 different designs, using a different prosthesis on each side, Pritchett investigated patient satisfaction after a 2 year period [37]. The prostheses that were used were AMP, anterior and posterior cruciate retaining, posterior cruciate-retaining, posterior cruciate-substituting and mobile bearing [37]. Patients with bilateral TKA preferred retention of both cruciates with the use of the ACL-PCL retaining prosthesis or substituting with an MP prosthesis. When flexion was assessed in groups of patients with an AMP and a PS TKA no significant differences were found at 12 months follow up [38]. The same study showed that knees with a preoperative flexion up to 90° gained the most after the knee replacement (mean 19.6° for the AMP knee). On the other hand, knees with a preoperative flexion of 125° or greater, lost flexion (average 2.9°). This was attributed to patient factors such as pain, swelling and poor compliance with rehabilitation [38]. The hypothesis that the implication of increased constraint in the medial compartment of the TKA may lead to earlier aseptic loosening was tested by Amin et al. [39]. The authors compared (Freeman-Samuelson 1,000 Medial Pivot – Medial Rotation Knee-MRK and Freeman-Samuelson 1,000 modular TKA’s) standard antero-posterior and lateral radiographs and studied radiolucent lines for component migration and signs of loosening. For a minimum follow-up period of 2 years, no sign of loosening was present in either group. Therefore, this early radiological survey concludes that the increased constraint of the medial pivot design did not result in an increased incidence of radiographic loosening [39].
In a Level I study conducted by Kim et al. [40], including 92 patients who had an AMP TKA implanted in one knee and a PFC Sigma mobile bearing TKA implanted in the other, the authors report that the early outcome of TKA is worse in the knees with the AMP compared to the PDC TKA. Knee scores and range of motion were worse in the AMP TKA, while a high infection rate was reported in the same group of patients [40]. The latter study has raised serious arguments in the literature with two letters to the Editor criticizing its methodology [41, 42].
Mid- and Long-Term Clinical Outcome
Several studies have shown favorable mid-term outcome of the Medial Pivot designs without records of implant related complications. In a multi-center study the clinical outcome of 298 AMP TKAs was reported after a minimum of 5 years follow up [43]. The 5 year survival rate was 97.2 %. Preoperative mean Knee Society Score and flexion were 33 points and 107° respectively, improving to 90 points and 121°. There was no sign of implant failure or migration. When compared to the average 6 year results of fixed INBS II and LCS TKA designs, AMP TKA showed superior flexion [43]. Satisfactory mid-term outcomes were also reported in another study of 55 consecutive patients who underwent 58 primary AMP TKAs [44]. The Knee Society Score improved from 30.5 to 91.1 and the functional score from 36.7 to 82.3. Few complications were found and most of the knees were found to be stable following thorough valgus–varus balancing [44]. Karachalios et al. [45] reports satisfactory outcomes for 284 AMP TKAs after a mean follow up of 7 years. Both objective and subjective clinical rating scales and serial radiographs were evaluated. All patients showed a statistically significant improvement in the Knee Society Score, Oxford knee score, SF-12 and WOMAC questionnaires. Range of motion improved from 101 to 117 on average. The majority of patients (93–95 %) experienced very good to excellent pain relief. This prospective clinical outcome study shows a cumulative success rate of 99.1 % at 5 years and 97.5 % at 9 years [45] (Figs. 15.8 and 15.9). More recently, Chinzei et al. [46] has retrospectively reported on 76 patients (85 knees) with AMP TKAs with a mean age at operation of 70.2 years and a mean follow-up period of 8 years (72–132 months). The survival rate at 8 years was 98.3 %. There was an improvement of knee extension angles (from 106.2 to 110.3°, p > 0.05) and of range of motion (from 94.2 to 110.6°, p < 0.05). All clinical evaluation scores (KSS, KSFS) improved significantly. According to the authors all AMP TKAs achieved excellent clinical and radiographic results without implant related failures at mid-term follow-up. Clinical and radiologic results of 172 AMP TKAs, at a mean follow-up period of 7 years, were presented by Vecchini et al. [47] showing a survival rate of 98.6 %. Satisfactory relief of pain was recorded in 90 % of patients, and 96 % of them were able to return to age-related daily life activities with 85 % of them showing excellent or good functional scores. Range of motion improved from a mean of 97.7° to a mean of 112.5° and Knee Society Score from a mean of 77.6 points to a mean of 152.8 points. Patients also judged stability and comfort during walking as satisfactory. In another study, the outcome of 50 consecutive AMP TKAs was evaluated with pre and postoperative clinical scores (Knee Society score system, Western Ontario and McMaster Universities Arthritis Index Score). Patient satisfaction was also documented and standard radiographs were used in order to record signs of failure. The results were then compared with the results in the Australian Orthopaedic Association National Joint Replacement Registry [48]. It was found that, in the mid-term, the AMP TKA provided pain relief, functional improvement and complication and revision rates similar to reported registry data.

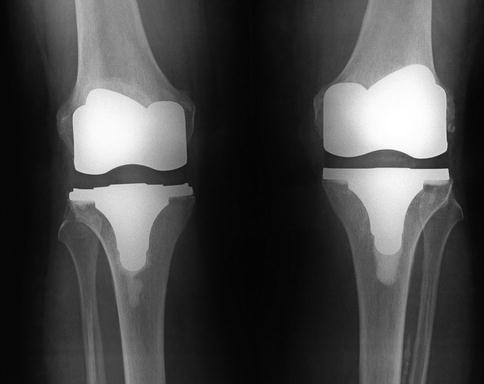

Fig. 15.8
Satisfactory radiological results of an AMP TKA (with the old version of PE insert locking mechanism) at 15 years follow up is shown
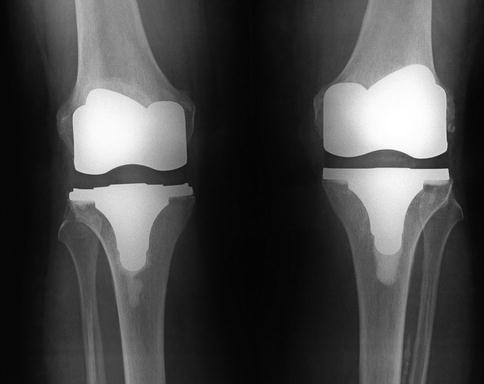
Fig. 15.9
Satisfactory radiological results of bilateral AMP TKA (right knee at 15 years and left knee at 14 years follow up) is shown
The AMP implant provides two different polyethylene liners, the conventional Medial pivot insert and the double high insert. The double-high tibial insert has been developed recently in order to provide high stability and high flexion. It has been designed with a 3 mm lower posterior lip, to allow posterior femoral rollback and get a better flexion angle. A comparison between the mid-term clinical results of the Medial Pivot insert and the double high insert, in combination with the same AMP TKA design, showed equally good results [49]. The authors suggest that improved range of motion cannot be expected from changes in the design of the tibial insert only [49].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







