Microfracture for Osteochondral Lesions of the Talus: Perspective 2
Raymond J. Walls
Keir A. Ross
Ethan J. Fraser
John G. Kennedy
DEFINITION
Osteochondral lesions of the talus (OLT) are common conditions that can involve both the cartilage and underlying bone of the talar dome and have the propensity to degrade and lead to osteoarthritis if left untreated.2,10 Cartilage injuries have a poor inherent healing response.
Bone marrow stimulation (BMS), initiating fibrocartilage through microfracture or microdrilling, is a commonly used technique for small, noncystic lesions.
The objective is to create multiple breaches in the subchondral plate to facilitate the flow of marrow with mesenchymal stem cells (MSCs) from the underlying bone.
ANATOMY
The talus articulates with the tibial plafond superiorly as well as the medial and lateral malleoli to form the ankle mortise.
Approximately 60% of talar surface is covered by cartilage.
It has no muscular attachments and thus its blood supply is derived from branches of the posterior tibial artery (artery of the tarsal canal and deltoid branches), the peroneal artery (artery of the tarsal sinus), and the dorsalis pedis.
PATHOGENESIS
The etiology is primarily traumatic with an incidence of between 50% and 70% following ankle sprains and fractures.7,11,13
Repetitive microtrauma leading to OLTs is often associated with ankle instability.11
Impaction, crush, and shearing injuries occur with the location of the OLT dependent on the position of the ankle at time of injury.
NATURAL HISTORY
Smaller lesions can occasionally heal with nonoperative management, although this is more commonly seen in a pediatric population.19
Theoretically, OLTs tend to progress, as highly pressurized fluid invades the subchondral plate through cartilaginous defects and eventually infiltrates subchondral bone.
Spontaneous healing is uncommon and there is a propensity for further degeneration.
Prevention of disease progression is aimed at repair of the subchondral plate and alignment of the joint.
Surgical intervention can be considered as reparative (BMS) or replacement (autologous chondrocyte implantation, autologous osteochondral transplantation, juvenile particulate cartilage).
PATIENT HISTORY AND PHYSICAL FINDINGS
OLTs may be asymptomatic.
Patients often, but not always, will recall an acute injury.
Activity-related deep anterior ankle pain is the typical complaint.
Mechanical symptoms such as clicking or locking of the ankle joint are less common and may indicate a loose fragment.
Clinical examination may reveal swelling and localized tenderness along the joint line.
Chronic cases with associated synovitis and joint effusions can have limited ankle motion.
As many cases occur with concomitant pathology, such as ankle instability, detailed clinical examination of the ankle osseous, ligamentous, and tendinous structures is advocated.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging studies are useful to assess lesion location, size, and depth as well as the presence of subchondral cysts preoperatively. This will determine the most appropriate treatment strategy.
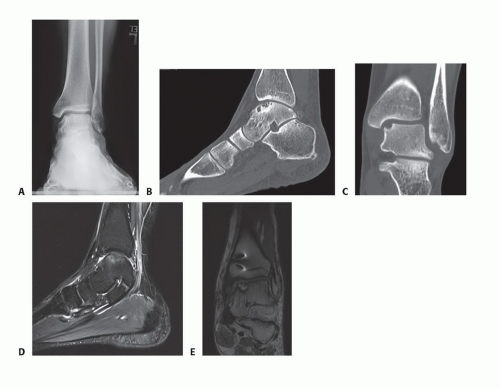
Standard weight-bearing plain radiographs (anteroposterior [AP], lateral, and mortise views) (FIG 1A)
May miss up to 50% of OLTs, especially if very small or isolated cartilage lesions9
Useful to assess lower limb, ankle, and hindfoot alignment
Computed tomography (CT) (FIG 1B,C)
Permits further evaluation of osseous morphology and dimensions, especially depth
Only gives information about the osseous structure; no information regarding overlying chondral loss or damage
Magnetic resonance imaging (MRI) (FIG 1D,E)
Recommended for a definitive diagnosis and evaluation
Evaluation of articular cartilage and the degree of subchondral involvement/bone edema
T2 mapping sequences provide increased sensitivity for cartilage architecture and quality.
Can also assess for concomitant pathology (ligamentous injury, tendinous injury, loose bodies, etc)
DIFFERENTIAL DIAGNOSIS
Anteromedial or anterolateral ankle impingement
Chronic ankle instability
Tendinopathy (peroneals, tibialis posterior, tibialis anterior)
Early posttraumatic osteoarthritis
Inflammatory arthropathy
Stress response or fracture
NONOPERATIVE MANAGEMENT
Indicated for minimally symptomatic, smaller, stable lesions that involve cartilage alone
A period of immobilization and restricted weight bearing followed by progressive weight bearing and physical therapy. Range-of-motion exercises are encouraged to preserve cartilage nutrition.
Pharmacotherapy (oral nonsteroidal anti-inflammatory drugs [NSAIDs] and intra-articular steroid injection)
The role of biologic adjuncts such as platelet-rich plasma (PRP), concentrated bone marrow aspirate (CBMA), and hyaluronic acid (HA) are under investigation.
SURGICAL MANAGEMENT
Microfracture was first described by Steadman et al17 and has gained widespread popularity, as it is marginally technically demanding, minimally invasive with minimal postoperative pain, is low cost, and is associated with low complication rates.
Indications
Failed conservative management
Consider retrograde drilling for subchondral bone lesions where the overlying cartilage is intact.
Absolute contraindications include severe degenerative joint disease and infection. Caution is recommended in the setting of active inflammatory arthropathy, especially if the patient is on long-term oral steroids.
Preoperative Planning
Based on clinical examination and preoperative imaging outlined earlier
The lesion location will determine surgical approach, whereas lesion size determines the technique.
Anterior arthroscopy is used for most lesions through standard anteromedial and anterolateral portals. Accessory posteromedial portals are also employed on occasion.
In our experience, approximately 75% of the ankle joint is accessible with the anterior approach.
Posterior arthroscopy is used for the most posterior of lesions. The original two-portal technique is safe and provides access not only to an OLT but other hindfoot, posterior ankle, subtalar joint, and extra-articular pathologies.16
Retrograde drilling is used for lesions in which the overlying cartilage is preserved and is performed under fluoroscopic navigation.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree