Meniscectomy
Introduction
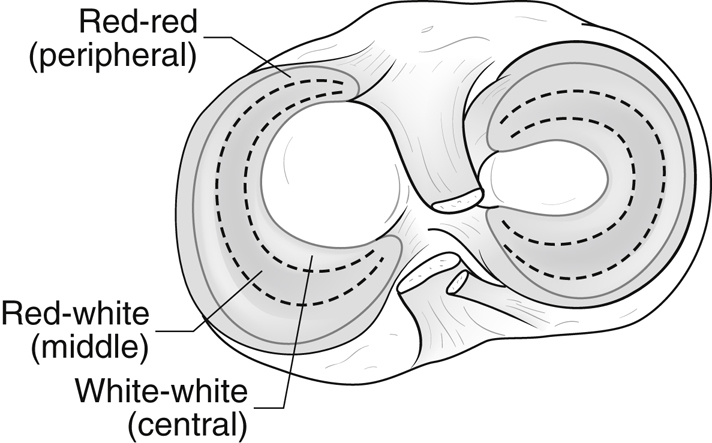
Figure 1Illustration of the vascular zones of the meniscus. The medial meniscus is on the left, and the lateral meniscus is on the right.
Most symptomatic meniscal tears are irreparable
Subtypes of meniscal tears
Simple patterns
Radial
Vertical/longitudinal
Horizontal
Complex patterns
Displaced bucket-handle
Parrot-beak
Multiplanar
Degenerative
Meniscal root tear
Location of tear directly affects the capacity for repair (Figure 1)
Peripheral third of meniscus—Red-red zone
Middle third—Red-white zone
Central third—White-white zone
The menisci occupy 60% of the contact area between the tibia and femur
They transmit 50% of compression forces across the joint
The medial meniscus is a secondary stabilizer against anterior translation in the anterior cruciate ligament–deficient knee
The lateral meniscus plays a much greater role in force transmission than the medial meniscus; the convexity of the lateral plateau leads to point loading after meniscal débridement, increasing peak contact pressures in the lateral compartment (235% to 335% in total meniscectomy)
Relative medial joint congruity buffers the effect of the meniscectomy on peak pressures
Circumferential meniscal collagen fibers distribute hoop stresses; disruption may lead to degeneration
Patient Selection
Indications for Repair
Repair should be attempted for young patient with red-red and red-white zone tears
For radial tears, repair red-red and red-white zones and débride white-white zone
Stable partial-thickness vertical tears less than 10 mm in the red-red zone may be treated with abrasion or trephination or left alone if showing healing
Indications for Meniscectomy
Irreparable tears due to
Degeneration
Fragmentation
Tearing of avascular tissue
Goals of meniscectomy
Resect irreparable and/or unstable meniscal tissue
Leave a contoured and smooth tissue remnant
Preserve over 50% of meniscal rim
Controversial in patients with underlying degenerative arthritis.
FIDELITY study group published in 2017 had 2-year follow-up of arthroscopic partial meniscectomy (APM) versus sham surgery. No statistical difference in outcomes. Multiple recent systematic reviews show that APM has equal or worse outcomes to nonsurgical management
Diagnosis
History—Symptoms include
Knee pain
Mechanical locking
Pain or swelling with activities of daily living, work, or sports
Knee effusion
Physical examination
McMurray test
Apley grind test
Thessaly test has an accuracy greater than 94% in anterior cruciate ligament–intact knees
Discoid meniscal tears
Typically present in a child younger than 10 years
Intermittent painful episodes of dramatic popping or snapping of the knee
Unable to fully extend knee
Clunk is elicited on examination with flexion, extension, and circumduction
Preoperative Imaging
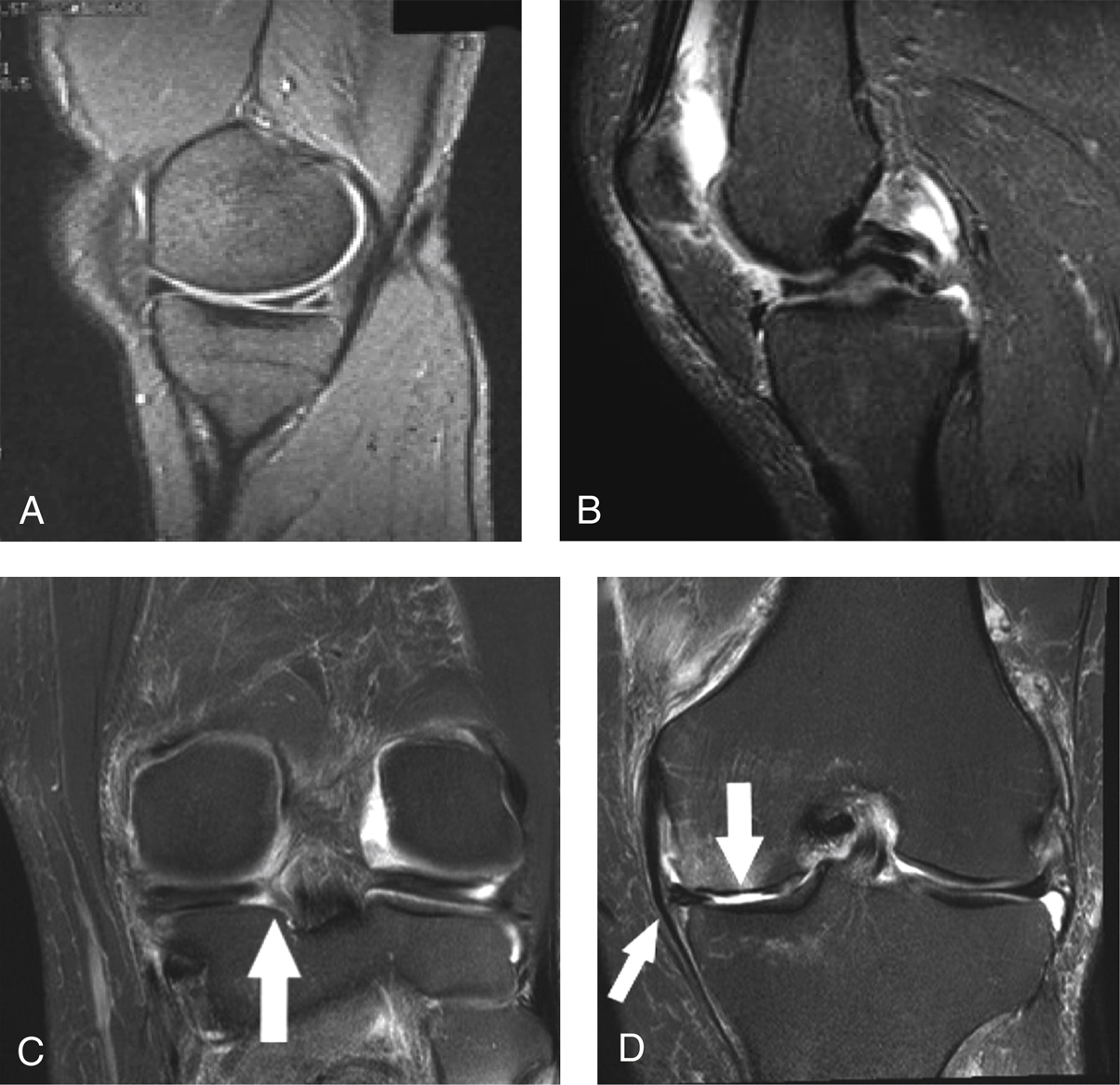
Figure 2Magnetic resonance images (3-T) show meniscal tears. A, Horizontal tear of the posterior horn extending to the inferior surface. B, Double posterior cruciate ligament sign, indicative of a displaced bucket-handle tear. C, Meniscal root tear (arrow) on coronal view. D, A tear at the root (large arrow) and extrusion of the meniscus (small arrow).
Radiographs include 30° flexion lateral, Merchant, AP weight-bearing in extension, and 45° PA flexion weight-bearing views
Best MRI sequences (Figure 2)



