Meniscal Repair
Nicholas A. Sgaglione
Kevin Myers
Adam Bitterman
DEFINITION
A meniscus tear results in mechanical disruption of the gross structure of the medial or lateral meniscus or both.
The goals of meniscus repair are to preserve and optimize meniscus function and to restore joint biomechanics, ultimately resulting in protection and preservation of the articular cartilage.
ANATOMY
The medial meniscus and the lateral meniscus are crescentshaped and triangular in cross-section.
The medial meniscus is C-shaped. It covers about 64% of the tibial plateau. Its width varies from anterior to posterior, with an average of 10 mm (FIG 1).
The lateral meniscus is more circular. It covers about 84% of the tibial plateau, with an average width of 12 to 13 mm.
The menisci are fibrocartilaginous structures made up of collagen (90% type I and the remainder made up of types II, III, V, and VI), fibrochondrocytes, and water.
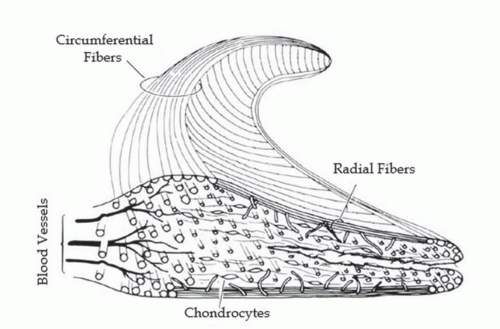
The collagen fibers are arranged in a circumferential pattern in the peripheral third, whereas the inner two-thirds is organized with a combination of radial and circumferential fibers (FIG 2).
The collagen fiber arrangement is integral in transforming axial force into a circumferential force within the meniscus. Three layers within the meniscus each have particular fibril arrangements.
Within the most superficial zone are fibers arranged in a meshlike pattern. The middle zone has fibers in a random array, whereas the deepest layer contains circumferential fibers. These deep zone fibers are cross-linked with radial fibers and function to prevent longitudinal tears (ie, bucket-handle tear). If a tear in the deep layer exists, the distribution of forces is subsequently altered and may lead to meniscal extrusion.14
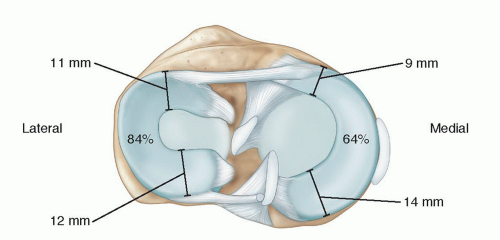
FIG 1 • Anatomy of the meniscus, showing the average sizes of the components of the medial and lateral meniscus with the average amount of tibial plateau coverage.
The menisci function to deepen the articular surface of the tibial plateau, providing shock absorption and compensating for gross incongruity between the articulating surfaces, acting as joint stabilizers. They provide joint lubrication and maintenance of synovial fluid and assist in providing nutrition of articular cartilage.39
The vascular supply comes from the perimeniscal capillary plexus supplied by the medial and lateral inferior and superior geniculate arteries. The plexus penetrates the meniscus peripherally and its abundance decreases as it crosses centrally. This difference in vascularity creates the red-red, redwhite, and white-white zones.5
The meniscus contains free nerve endings and corpuscular mechanoreceptors, providing pain and proprioception in the knee joint.39
PATHOGENESIS
Acute tears typically occur in younger patients from compression and rotational injury of the knee joint as it moves from a flexed to an extended position.
Degenerative tears are typically chronic in nature, are found in older patients, are complex, and are usually irreparable.
Medial meniscus tears most often occur in the stable knee or chronic anterior cruciate ligament (ACL)-deficient knee, whereas lateral tears occur more often in younger patients with acute ACL tears.
Associated injuries are often found. The “terrible triad” consists of tears of the lateral meniscus, ACL, and medial collateral ligament (MCL). It is often sustained from a hyperextension with a valgus stress, such as during a “clipping” injury in football.
Tears may be classified according to anatomic zone (as described by Cooper et al13), vascularity (red-red, red-white, white-white), or by tear pattern.
Tear patterns are described as horizontal, radial, longitudinal, bucket-handle, oblique, or complex.13
NATURAL HISTORY
Walker and Erkman49 in 1975 found that with loads up to 150 kg, the lateral meniscus bore most of the weight bearing in that compartment, whereas the medial meniscus shared about 50% of the load with the articulating surfaces of the tibiofemoral joint.
Partial and total meniscectomy has been shown to increase the contact stresses exerted on the articular cartilage, resulting in its degeneration and ultimately osteoarthritis.
After partial meniscectomy, femoral-tibial contact areas decrease by about 10%, with peak local contract stresses (PLCS) increasing by about 65%. After total meniscectomy, contact areas decrease about 75% and PLCS increases about 235%.7
Lee et al24 demonstrated significantly decreased contact areas and increased mean and peak contact stresses compared to the intact meniscus for tears involving 50% radial width, 75% radial width, segmental, and total meniscectomy.
Vertical tears of the meniscus were found to have contact areas and pressures similar to total meniscectomy, with repair yielding values near to the normal meniscus.31
The menisci also contribute to joint stability, especially in the anteroposterior (AP) plane. In a cadaver study, a longitudinal tear of the posterior horn of the medial meniscus in the ACL-deficient knee was found to result in a significant decrease in AP joint stability compared to the ACL-deficient knee with intact meniscus.2 Repair of the meniscus restored kinematics to the ACL-deficient, intact meniscus level.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history should include location of pain (joint line tenderness), recent traumas, prior injuries and surgery, as well as evidence of effusions, locking, catching, or instability (which may indicate associated ligamentous pathology).
In addition, questions should be asked about the patient’s age, function, activity level, occupation, goals, expectations, and other pertinent medical problems. These will help the surgeon decide on nonsurgical versus surgical treatment and resection versus repair.
A complete examination of the knee should be performed, including evaluation for the following:
Anterior and posterior ligament injury: Lachman, anterior and posterior drawer, pivot shift, along with a history of hearing a “pop” with injury and acute swelling
Posterolateral corner injury: injury of the popliteus tendon, iliotibial band, popliteofibular ligament, biceps, and posterior capsule. Asymmetry on the dial (external rotation) test is the most sensitive examination.
Collateral ligament injury: Medial and lateral collateral ligament injuries may be assessed by palpation and widening with varus-valgus stresses at 30 degrees and at full extension.
The examiner should also
Inspect for effusion. The presence of diffuse joint effusion is not specific enough. A localized swelling at the joint line may indicate a parameniscal cyst.
Palpate all ligament and tendon insertions as well as the patellofemoral joint; this may indicate associated pathology.
Evaluate range of motion. Loss of extension or locking may relate to a displaced or bucket-handle tear. Pain with squatting may indicate a posterior horn tear.
Perform the McMurray test—flex the knee, bring knee into extension with external rotation and valgus while palpating the medial joint line, or bring the knee into extension with internal rotation and varus while palpating the lateral joint line. Pain or popping/clicking is indicative of a meniscal tear.
Perform the Apley test to look for a meniscus tear—place patient prone, flex knee to 90 degrees, apply an axial load while internally and externally rotating the knee. Relief on distraction is found if a meniscus tear is the only pathology, but no relief will be found if a concomitant collateral ligament injury is present.
Perform the Childress test—have the patient assume a squatting position and either repeatedly squat or walk while squatting. The test is positive if the patient has pain or mechanical blocking; this may indicate a meniscus tear.
While assessing for the Merkel sign, pain with internal rotation of tibia is consistent with a medial meniscus tear; pain with external rotation is consistent with a lateral meniscus tear.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs should be taken to evaluate for bony pathology, extremity alignment, arthritis, chondrocalcinosis, or findings consistent with associated injuries such as a Segond sign (ACL injury), osteochondritis dissecans lesion, or osteochondral fracture.
Typically, four views are obtained: a 30- or 45-degree posteroanterior flexion weight-bearing view, a true lateral view, a notch view, and a patella skyline view.
Magnetic resonance imaging (MRI) is not always indicated to evaluate for meniscal pathology, but it is typically used and helpful in evaluation of associated injuries when a meniscus tear is suspected. The sensitivity of MRI for meniscus tears is reported as high as 96%, with a specificity of 97%.26
MRI classification is as follows:
Grade 1: small focal area of increased signal, not extending to the joint surface
Grade 2: linear area of increased signal, not extending to the joint surface
Grade 3: linear area of increased signal extending to the joint surface
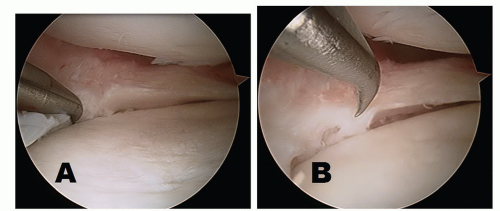
A linear abnormality is identified as extension to the articular surface on two consecutive images and is considered to have a high likelihood of being a true tear (FIG 3A).
A bucket-handle tear may be identified by the “double PCL” (posterior cruciate ligament) sign (FIG 3B,C).
Evaluation of the meniscus postoperatively presents a challenge because the repair site becomes filled with fibrous scar and may continue to produce abnormal magnetic resonance signal on postoperative imaging. Currently, the best method of evaluation is with a gadolinium-enhanced MRI.
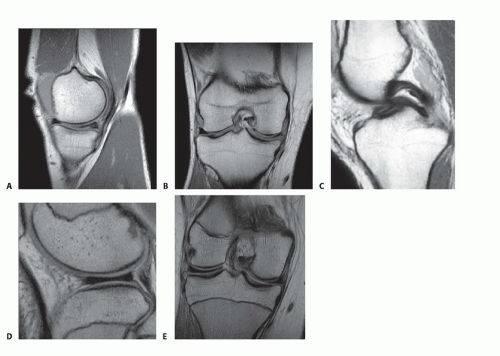
FIG 3 • A,B. Lateral and posteroanterior MRIs of meniscus tears. C. MRI of medial bucket-handle meniscus tear and double PCL sign. D,E. Sagittal and coronal MRIs of discoid lateral meniscus tears.
A discoid meniscus may be evident on MRI as a rectangular meniscus on all slices as opposed to the wedge shape typically seen. It is more commonly found in the lateral meniscus (FIG 3D,E).
DIFFERENTIAL DIAGNOSIS
ACL or PCL tear
Medial or lateral collateral ligament tear
Osteochondritis dissecans lesion
Patellofemoral syndrome
Osteoarthritis
Chondrocalcinosis
NONOPERATIVE MANAGEMENT
Conservative treatment options include physical therapy, nonsteroidal anti-inflammatory medications, steroid injections, and activity modification.
Typically, a stable longitudinal tear in the periphery less than 10 mm is likely to heal on its own.
Bracing usually is not indicated in the treatment of meniscus tears.
The expected result of nonoperative treatment is improved symptoms in 6 weeks, with return to full activities by 3 months.
SURGICAL MANAGEMENT
Intervention may proceed after failure of conservative treatment or more urgently if the patient shows mechanical symptoms such as locking or catching. These may represent loose bodies or an unstable torn meniscus (ie, bucket-handle tear), which can cause significant articular damage if left untreated.
With all meniscus pathology, the goal is to preserve as much meniscus as possible.
Repair versus resection
The potential long-term benefit of repairing the meniscus is chondroprotection.
The surgeon should consider tear location, pattern, vascularity, tissue viability and ability to hold repair sutures, and associated pathology when determining whether to repair or resect the meniscus.
The surgeon should consider the patient’s age, activity level, overall health, and compliance with a limited postoperative activity regimen.
When resection is performed, all efforts should be made to preserve as much viable meniscus as possible.
Mobile, unstable meniscus fragments should be resected, leaving a smooth contour.
The peripheral rim of meniscal tissue should be carefully assessed and measured to determine the “rim width.” This is the area where the circumferential collagen fibers are located and function to provide the ultrastructural integrity to resist joint compressive hoop stresses and should be preserved.
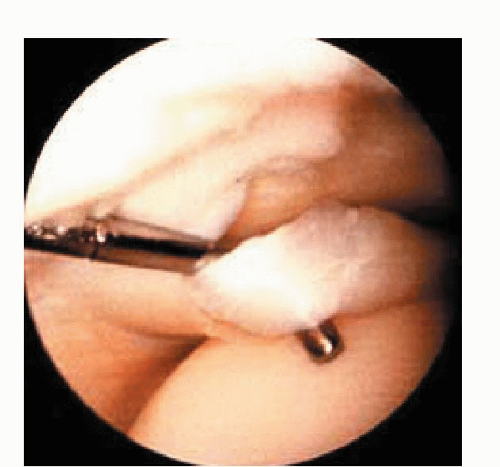
The surgeon should consider leaving a stable tear alone. An unstable tear will be easily mobilized, displaced at least 7 mm, and/or will have the ability to “roll” (FIG 4).
Preoperative Planning
Before surgery, all radiologic studies should be reviewed and clinical correlation must be confirmed. Comprehensive patient counseling should also be performed.
The knee should be examined under anesthesia before beginning the surgery in an attempt to detect associated pathology.
The healing potential for a meniscus repair in conjunction with an ACL reconstruction is far superior to that of a repair alone.
The surgeon should discuss with the patient the risks and benefits of the surgery as well as the principle of informed consent.
All patients should be apprised of the possibility of meniscus resection versus repair. They should understand the implications of each in terms of short- and long-term consequences, including risks of failure and rigors of postoperative rehabilitation protocols.
The surgeon may discuss the potential for associated pathology and may obtain a better understanding of the patient’s treatment preferences before entering the operating room. This may be a particularly crucial conversation with an elite athlete who would prefer to undergo a resection in an attempt to return to competitive sport faster.
The anesthesia used is typically decided on by the anesthesiologist and orthopedist before entering the operating room. General anesthesia or a laryngeal mask airway (LMA) may be used.
We prefer to have the anesthesiologist provide sedation in conjunction with a local anesthetic administered by the surgeon.
We typically use a mixture of 0.5% Marcaine and 1% lidocaine with epinephrine in equal proportions. About 30 to 40 mL is injected intra-articularly, and about 5 mL is injected into each portal site.
Positioning
Typically, the patient is lying supine.
There are two methods for using an intraoperative leg support device to facilitate coronal plane valgus joint distraction; these include the use of a knee holder or a lateral post.
The knee holder should be placed perpendicular to the position of the femur at a level above the patella and portals that allows for a valgus force on the knee.
The end of the table is dropped down below 90 degrees from horizontal to allow both legs to hang freely from the knees.
The lateral post should be placed above the patella and angled outwardly to allow for a valgus force on the operative knee. This technique is performed without dropping the end of the table.
The surgeon should check that the knee may be taken through a range of motion by abducting the leg against the lateral post with flexion of the knee off the side of the table.
A tourniquet may be placed on the upper thigh if bleeding is suspected, such as in débridement of hypertrophic synovitis or a hypertrophic fat pad.
Padding of the contralateral leg is used to prevent pressurerelated injury to the bony prominences or superficial nerves.
Approach
The typical portal sites are anteromedial and anterolateral (FIG 5).
In addition, a superomedial portal can be made proximal to the superior pole of the patella in line with the medial border of the patella (medial to the quadriceps) and is directed in an oblique manner to the joint.
This portal is typically used for outflow or inflow.
The anterolateral portal is created by making a small (about 6 mm) stab incision 1 cm proximal to the joint line and 1 cm lateral to the patella tendon.
This area can be identified as the “soft spot.” This portal is used for insertion of the arthroscope.
The anteromedial portal is considered the working portal for insertion of instruments. It is typically made under direct visualization by inserting a spinal needle into the medial soft spot 1 cm medial to the patella tendon and 1 cm proximal to the joint line.
Accessory portals are useful depending on tear patterns and repair strategies and may include superolateral, posteromedial, posterolateral, midpatella, central, far medial, or lateral (FIG 5).
Meniscal tears may be stimulated to heal with either rasping or trephination. Rasping may be performed with either an arthroscopic shaver or a meniscal rasp that lightly abrades both the tibial and femoral edges of the tear site, as well as the meniscosynovial junction, to stimulate vascularity.

FIG 5 • Placement of the standard (superolateral, anteromedial, and anterolateral) and accessory arthroscopic portals in the knee.
Trephination is performed by inserting a long 18-gauge needle either percutaneously or through the arthroscopic portals across the meniscus tear to create vascular channels.
The surgeon should avoid perforation of the meniscus surface, causing further injury.
The MCL pie-crusting technique can be performed to avoid articular cartilage damage/scuffing in the tight medial compartment. An 18-gauge needle or arthroscopic awl is used to create multiple punctures in the deep MCL while a valgus force is applied. The punctures should begin posteriorly and advance anteriorly until adequate visualization is obtained6 (FIG 6).
TECHNIQUES
▪ Inside-Out Technique
This technique requires passage of double-loaded 2-0 or 0 nonabsorbable and/or high-strength sutures with long flexible needles passed arthroscopically and directly through low-profile contoured suture cannulas (TECH FIG 1A-E).
It is best used for posterior horn, middle third, peripheral capsule, and bucket-handle tears.
Before passage of the sutures, an incision is made posteromedial or posterolaterally to capture the needles as they exit through the capsule. In this manner, all neurovascular structures are protected.
For passage of a needle through the medial compartment, the knee is placed in 20 to 30 degrees of flexion to avoid tethering the capsule.
A 4- to 6-cm posteromedial incision is made just posterior to the MCL, extending about one-third above and two-thirds below the joint line.
Dissection is continued anterior to the sartorius and semimembranosus musculature, deep to the medial head of the gastrocnemius.
The posterolateral incision is made with the knee in 90 degrees of flexion to allow the peroneal nerve, popliteus, and lateral inferior geniculate artery to fall posteriorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree