Chapter 12 Meniscal Allograft Transplantation
Introduction
Loss of meniscal tissue drastically alters the biomechanical environment of the knee joint, especially in the lateral compartment, where contact stress can increase by 200% to 300% after total meniscectomy. Compartment overload syndrome can ensue, presenting with weight-bearing pain and recurrent effusions. Secondary osteoarthritis is a predictable endpoint,1,2 which has led to increased awareness among orthopedic surgeons of meniscal transplantation in cases where subtotal or total meniscectomy was unavoidable. In carefully selected patients, meniscal allograft transplantation can provide improved biomechanics and function while providing good pain relief.3–5
This chapter discusses the techniques for open and arthroscopic meniscal allograft transplantation.
Indications
The ideal patient for meniscal allograft transplantation has a history of prior total or subtotal meniscectomy, usually followed by a symptom-free interval of varying duration. This is followed by the onset of weight-bearing pain localized to the involved compartment, frequently with recurrent effusions. The articular surfaces should be without full-thickness chondral defects, ligaments should be stable, and the knee should be normally aligned; otherwise, these comorbidities must be addressed in concurrent or staged fashion. Several reports that investigated the outcomes of concurrent meniscal transplantation and cartilage repair demonstrated results comparable to isolated meniscal transplantation.6,7 Therefore, repairable, focal chondral defects should not be viewed as a contraindication.
Planning
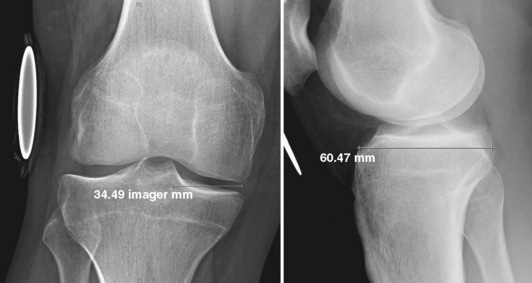
Meniscal allografts are size, side, and compartment specific; therefore, they must be individually measured and ordered for each patient. Preoperative measurements are obtained from AP and lateral radiographs with magnification markers placed on the skin at the level of the joint line. After accounting for radiographic magnification, meniscal width is measured on the AP radiograph from the edge of the ipsilateral tibial spine to the edge of the tibial plateau. Meniscal length is calculated by multiplying the depth of the tibial plateau (as measured on lateral radiographs) by 0.8 for medial and 0.7 for lateral meniscal grafts (Figure 12–1).
Graft preparation
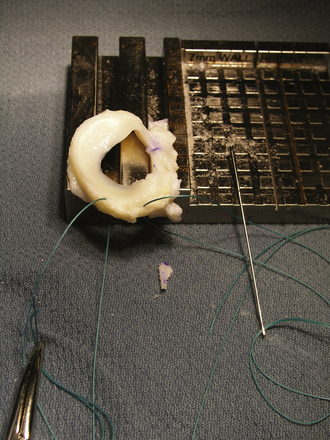
Depending on the specific system used, the bone bridge or plugs are prepared and sutures are placed. For our preferred technique, pull sutures are placed in the posterior horn (Figure 12–2) to assist in reducing the meniscus under the femoral condyle. Additional sutures can be placed through the bone bridge/plugs and around the meniscal roots to assist in graft fixation. After the graft has been prepared, any residual marrow elements should be removed from the bone using pulse lavage.