, Antonio Cesarani2 and Guido Brugnoni3
(1)
“Don Carlo Gnocchi” Foundation, Milano, Italy
(2)
UOC Audiologia Dip. Scienze Cliniche e Comunità, Università degli Studi di Milano, Milano, Italy
(3)
Istituto Auxologico Italiano, Milano, Italy
Abstract
Ménière’s disease (MD) is a chronic illness of the inner ear that affects a substantial number of patients every year worldwide. Ménière’s disease may be classified according to different levels of certainty. The key lesion is the histopathological alteration of the inner ear called endolymphatic hydrops. In some cases, the aetiology of hydrops may be considered unknown, but in several patients, causal factors may be identified: post-viral infection, metabolic disorders like hyperinsulinemia, vascular disorders, autoimmune and food intolerances like gluten sensitivity. The key disabilities are vertigo or dizziness attacks, intercritical unsteadiness and fear of acute attacks. The main therapy is based on drugs and lifestyle amelioration. Rehabilitation may be addressed to (1) prepare the patient to imbalance provoked by labyrinthectomy, called vestibular prehab, (2) treat the acute vertigo seen after vestibular neurectomy or labyrinthectomy, (3) amelioration of intercritical unsteadiness, (4) manage fear of acute attacks and (5) decrease the frequency of acute attacks.
Ménière’s disease (MD) is a chronic illness of the inner ear that affects a substantial number of patients every year worldwide. The disease is characterized by intermittent episodes of vertigo lasting from minutes to hours, with fluctuating sensorineural hearing loss, tinnitus and aural pressure. Attacks of vertigo may come on suddenly or after a short period of tinnitus or muffled hearing. Some people have single attacks of vertigo or dizziness once in a while. Others may have many attacks close together over several days. Some people with Ménière’s disease may have very severe attacks to lose their balance and fall.
Ménière’s disease may be classified according to different levels of certainty (Table 10.1) [1].
Table 10.1
The American Academy of Otolaryngology—Head and Neck Surgery criteria for diagnosis of Ménière’s disease
The definition of the disease requires the combination of: |
1. Recurrent spontaneous and episodic vertigo. A definitive spell of vertigo lasting at least 20 min, often prostrating, accompanied by disequilibrium that can last several days; usually nausea or vomiting, or both; no loss of consciousness. Horizontal rotatory nystagmus is always present |
2. Hearing loss (not necessarily fluctuating) |
3. Either aural fullness or tinnitus, or both |
The classification of the disease is graded as follows: |
Certain Ménière’s disease |
Definite disease with histopathological confirmation |
Definite Ménière’s disease |
Two or more definitive episodes of vertigo with hearing loss, plus tinnitus, aural fullness, or both |
Probable Ménière’s disease |
Only one definitive episode of vertigo and the other symptoms and signs |
Possible Ménière’s disease |
Definitive vertigo with no associated hearing loss or hearing loss with non-definitive disequilibrium |
The key lesion is the histopathological alteration of the inner ear called endolymphatic hydrops, that is, an excess of fluid in the inner ear. It is thought that endolymphatic fluid bursts from its normal channels in the ear and flows into other areas, causing damage. In some cases the aetiology of hydrops may be considered unknown, but in several patients, causal factors may be identified: post-viral infection [2–5], metabolic disorders like hyperinsulinemia [6–9], vascular disorders [10], autoimmune disorders [11–13] and food intolerances like gluten sensitivity [14, 15].
The key disabilities are vertigo or dizziness attacks, intercritical unsteadiness and fear of acute attacks. The main therapy is based on drugs and lifestyle amelioration [16, 17].
Vestibular neurectomy and chemical [18, 19] or surgical [20] labyrinthectomy are the treatment of choice when conservative therapies are unsuccessful.
Rehabilitation [21] may be addressed to:
1.
Prepare the patient to imbalance provoked by labyrinthectomy by means of a pretreatment plan before planned vestibular lesions, so-called vestibular prehab [22]
2.
Treat the acute vertigo seen after vestibular neurectomy or labyrinthectomy [23], as a post-operative plan
3.
Amelioration of intercritical unsteadiness
4.
Manage fear of acute attacks
5.
Decrease the frequency of acute attacks
10.1 Vestibular Prehab
Prehab has been proposed for subjects undergoing gentamicin treatment, as in chemical labyrinthectomy. Subjects would perform vestibular exercises for 2 weeks before the first gentamicin installation or surgical operation.
Exercises in the gymnasium to be performed with the therapist three times a week
1.
Relaxation exercises such as control of breathing with improving consciousness of abdominal or thoracic breathing. A simple exercise consists in deep inhalation followed, after few seconds, by a forced exhalation pronouncing the word “one”. This exercise is repeated 8–10 times.
2.
3.
In the sitting position, the patient grasps a stick with both hands and takes the stick behind her/his shoulder, positioning the stick at the level of the cervico-dorsal junction. In this position, she/he pushes the stick against her/his back, exhaling and inhaling rhythmically and slowly. She/he then repeats the exercise, moving the stick forward on the sternum at the level of the sterno-clavear joint. The patient grasps the stick with both hands frontally positioned.
4.
Standing on a foam mattress.
(a)
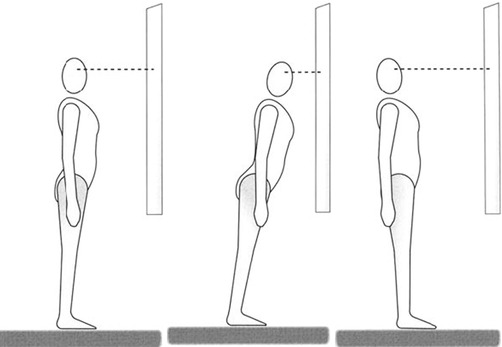
The patient fixates her-/himself in a mirror. The therapist helps her/him to align her/his position correctly. She/he must maintain equilibrium for 1 min with eyes open and then close her/his eyes visualizing her/his correct position while remaining in this position for at least 1 min.
(b)
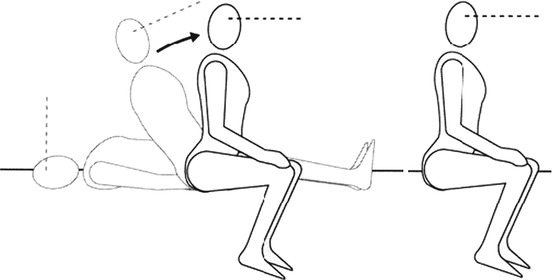
The patient fixates her-/himself in a mirror (Fig. 10.2a). Then she/he oscillates right and left (Fig. 10.2b), around her/his pelvis. She/he then resists the therapist’s attempts at destabilizations (Fig. 10.2c) and maintains equilibrium, crossing the legs (Fig. 10.2d).
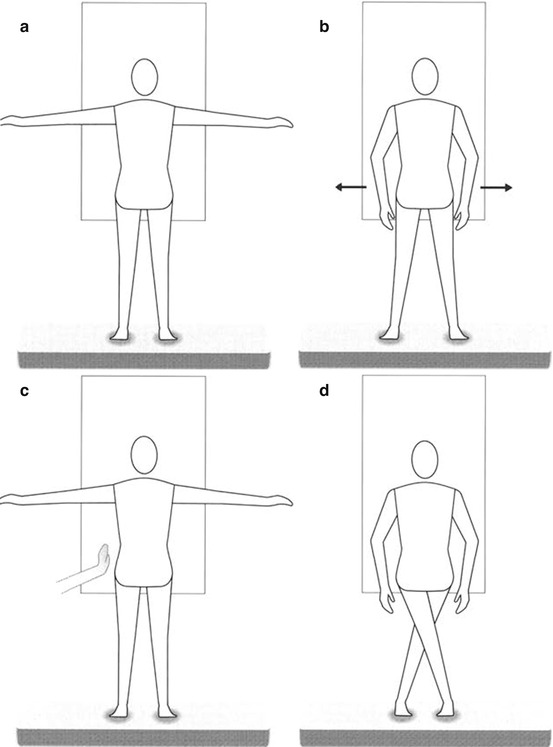
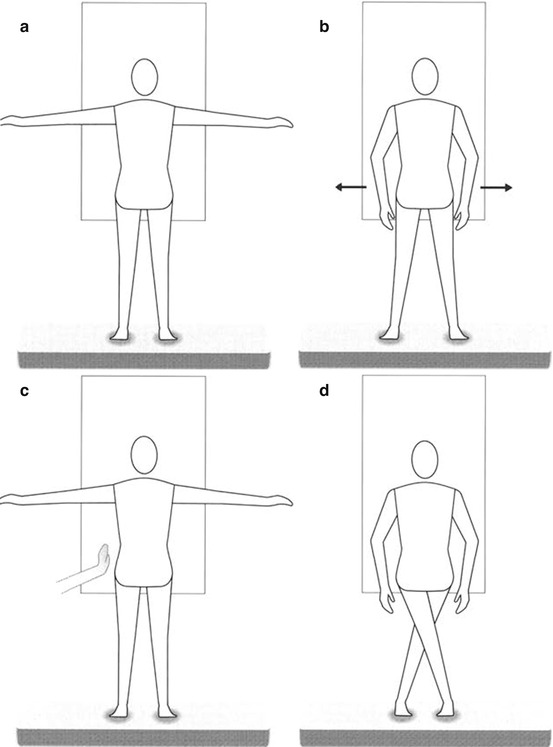
Fig. 10.2
The patient aligns himself looking at a mirror (a), then he oscillates (b), then resists when the therapist destabilizes him (c) or he maintains equilibrium crossing the legs (d) (Originally published in Cesarani and Alpini [38] published by Springer © 1999)
(c)
(d)
The patient holds a small object and then lifts it over her/his head and fixates it. With his arms extended, she/he moves it in circles of increasing width while maintaining the fixation of the object (Fig. 10.4).
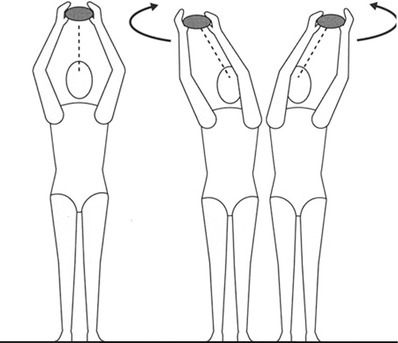
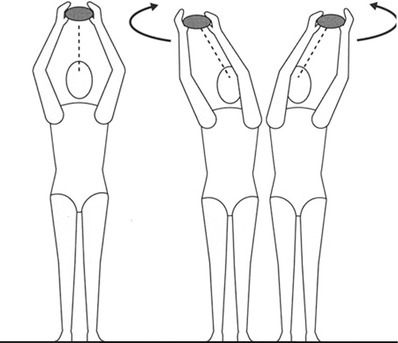
Fig. 10.4
Patient fixates a small object while moving it in circles, standing on a mattress (Originally published in Cesarani and Alpini [38] published by Springer © 1999)
5.
Standing on an oscillating platform (so-called Freeman board, or balance board, etc.), looking in the mirror.
(a)
The patient concentrates on a proper posture using a mirror to see her/his reflection and thus she/he tries to maintain equilibrium as longer as possible (no more than 1′)
(b)
The patients transfers her/his weight from one foot to the other with a smooth flowing motion.
(c)
The patient tries to maintain a proper posture while the therapist destabilizes her/him with gentle pushes
(d)
The patient tries to touch some targets (post-its of different colours) placed in different positions on a facing mirror.
(e)
The patient maintains equilibrium on one leg, the leg on the good side and then the leg on the affected side, as long as possible
(f)
Repeat exercises d and e wearing pinhole glasses.
10.2 Post-operative
Post-operative acute vertigo has to be treated as a form of sudden unilateral vestibular loss as shown in Chap. 5.
10.3 Intercritical Unsteadiness
Intercritical dizziness has to be treated as a form of chronic vestibular loss as shown in Chap. 6.
10.4 Vertigo Attack Fear
Vertigo spells fear has to be treated as a form of phobic postural vertigo as shown in Chap. 13.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree