CHAPTER 12 Medial Unicompartmental Knee Replacement
Cementless Options
 Cementless fixation in unicompartmental knee replacement has the theoretical potential of very long-term biologic fixation.
Cementless fixation in unicompartmental knee replacement has the theoretical potential of very long-term biologic fixation. Initial fixation is of paramount importance; implant design should allow an initial stable construct to allow effective osseointegration to occur.
Initial fixation is of paramount importance; implant design should allow an initial stable construct to allow effective osseointegration to occur.Rationale
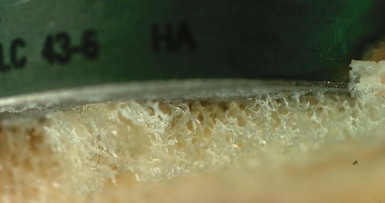
The development of cementless UKR has mirrored that of total knee replacement (TKR), with the use of porous coatings, with and without hydroxyapatite, and, in some designs, the addition of cancellous screw augmentation. All designs have utilized a keel on the tibial component, although the shape, size, and direction have shown considerable variation (Figs. 12–1 and 12–2). The femoral component has usually mirrored the cemented equivalent for each design, although those femoral designs with a single peg had a second peg added for rotational stability.
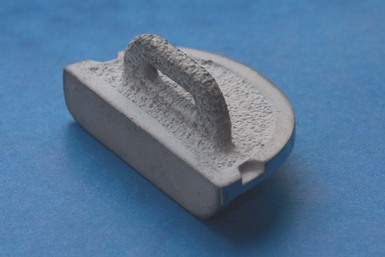
Figure 12–1 A cementless Oxford tibial component demonstrating a porous titanium layer with a hydroxyapatite coating.

(Photograph courtesy of Jean-Alain Epinette.)
One of the first advocates of cementless UKR was Jean-Alain Epinette,1 who designed and developed a hydroxyapatite-coated tibial component. This component differed from most designs by employing a horizontal keel that slotted beneath the tibial spines, thus maintaining bone stock beneath the tibial tray. In addition, there were cancellous screws to augment the initial fixation. Kaiser and Whiteside further highlighted the importance of initial stability in 1990, with a cadaveric in vitro study demonstrating the additional stability provided by cancellous screws in a unicompartmental tibial component, compared with a posteriorly angled peg.2
Cementless fixation in UKR has mainly been used in the few centers that are strong advocates of unicompartmental surgery. The latest reports from the Australian and New Zealand joint registries show that cementless UKR accounts for 11% and 6% of all UKR procedures, respectively.3,4 The Swedish register reported that all the UKRs performed in 2009 had both components cemented.5 Neither the National Joint Registry of England and Wales nor the Canadian registry gives information regarding fixation method for UKR.6,7
Although the presence of thin, nonprogressive, radiolucent lines (Fig. 12–3) has long been recognized in knee arthroplasty, with no associated increase in failure rate, the exact cause and effect of these lines is still unknown. There is, however, a perception that a radiolucent line is indicative of suboptimal fixation. The incidence of radiolucency differs beneath different implants, suggesting that the mechanical environment is important in their development. Forsythe et al.8 reported an incidence of over 50% with the cementless Whiteside Ortholoc II UKR, whereas Pandit et al.9 reported just 7% of cementless Oxford tibial components had a partial radiolucency, with none with a full radiolucency. There is also a reported increase in incidence of radiolucent lines with cemented Oxford components compared to the cementless version.9 There is no clear consensus on the role or importance of thin (≤1 mm), stable, so-called physiologic radiolucent lines, although there is evidence that they are not associated with either loosening or a decrease in clinical outcome scores. However, the greatly reduced incidence in cementless UKR is encouraging and suggests good bony fixation (Fig. 12–4). The Oxford UKR is particularly suited to cementless fixation because of the fully mobile bearing. The bearing movement causes a marked reduction in shear forces being transmitted through the tibial tray, and therefore the tray is mostly subjected to compression. This is an almost ideal mechanical environment for cementless fixation. Radiostereometric analysis studies of cementless fixation in TKR have shown a consistent pattern of migration, which differs from cemented fixation. Cemented components usually demonstrate continuous early migration, but the magnitude is small and stability is achieved by 2 years. In contrast, cementless components usually migrate a larger amount in the first few months before stabilizing. Onsten and Carlsson have demonstrated a reduction in the movement between 1 and 2 years postoperatively with the addition of a layer of hydroxyapatite to a porous-coated PFC tibial component.10,11 Likewise, Regner et al. demonstrated the reduction in maximum total point movement at 5 years in the Freeman-Samuelson TKR tibial component with the addition of hydroxyapatite to the undersurface.12
Indications
The indications for UKR are controversial and vary according to the surgeon’s philosophy. At Oxford, our view is that there should be full-thickness cartilage loss on both the medial tibial plateau and femoral condyle (bone-on-bone osteoarthritis), any intra-articular varus deformity should be correctable, and the anterior cruciate ligament (ACL) should be intact. Patello-femoral joint damage is ignored unless there is severe damage laterally. Cartilage damage on the lateral femoral condyle is permissible provided there is full-thickness cartilage present on a valgus stress radiograph and there is no full-thickness loss centrally. Full-thickness damage on the medial side of the lateral femoral condyle is not a contraindication.13 We do not consider age, gender, activity level, or Body Mass Index to be contraindications. These indications are our routine for both cemented and cementless UKR. Bontemps also noted that the indications for cemented and cementless UKR are the same; however, due to cost saving, he favors cemented fixation in the elderly.14 The suitability of cementless UKR in cases of osteonecrosis or areas of bone loss is less easily described. The consensus in our group is that, if the knee is suitable for cemented UKR once the bony surfaces are prepared, then cementless UKR is also indicated. Our rationale for this is based on evidence that one does not require total bony ingrowth to maintain implant stability and therefore, if the bony surface can support the implant, then either fixation method is acceptable. Epinette’s group demonstrated implant stability in cementless UKR when the amount of bony contact between tibia and component was between 38% and 52%1 (Fig. 12–5).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree