CHAPTER 10 Medial Unicompartmental Knee Arthroplasty
Fixed-Bearing Techniques
Introduction
The potential advantage of unicompartmental knee arthroplasty (UKA) over tricompartmental replacement is the preservation of the bone stock in the remaining compartment and the preservation of the ligaments. This concept requires an accurate and reproducible surgical technique. The most important evolution in UKA during the last decade is minimally invasive surgery, which can be defined as the ability to implant the components without an incision in the quadriceps tendon or the vastus medialis and without everting the patella.1,2 When performing UKA, surgeons must bear in mind that proper implant positioning should not be compromised by using too small an incision.
Success of the procedure will be related not only to proper surgical technique but also to proper patient selection.1–5 The indications for UKA are painful osteoarthritis or osteonecrosis limited to one compartment of the knee associated with significant loss of joint space on the radiographs on a stable knee.5–9 Age and weight still represent debatable issues for the indication of UKA as the procedure is often presented as an alternative to either osteotomy or total knee arthroplasty (TKA).5–9 Obesity itself is consequently not a contraindication. We do use the “SAW” concept (stability, alignment, and wear) to confirm the indication of UKA. Therefore, the knee should be stable and aligned and cartilage wear should be limited to one compartment of the knee. These criteria are checked preoperatively, and the physical examination should ensure that the knee is stable in the anteroposterior and sagittal planes and that the range of knee flexion is greater than 100° with a full knee extension. The patellofemoral joint should be clinically asymptomatic to confirm that wear is limited to one compartment.
To complete the physical examination, a systematic radiologic analysis should include anteroposterior and mediolateral views of the knee, full-length radiographs, stress radiographs,10 and skyline views (Fig. 10–1). The radiographic analysis should ensure that there is no patellofemoral loss of joint space on skyline views at 30°, 60°, and 90° of flexion; the presence of full-thickness articular cartilage in the nonaffected compartment; and full correction of the deformity to neutral on stress radiographs performed with the patient supine using a dedicated knee stress system. The angle between the mechanical axis of the femur and the anatomic axis of the femur, as well as the mechanical axis of the lower limb, should be calculated on the full-length radiograph. A varus or valgus deformation of the lower limb greater than 15° may represent a contraindication for UKA as the correction of such deformation may require soft tissue release, which should not be performed when doing UKA.11,12 When there is a question regarding the status of the anterior cruciate ligament (ACL) following the clinical examination, magnetic resonance imaging may be useful to confirm that the ACL is intact. This step, including patient selection and confirmation of the indication, represents probably the most important step and is really a basic warranty to the success of the procedure.
Setup and Equipment
The procedure can be performed under general or epidural anesthesia. We do use a tourniquet inflated at the proximal part of the thigh. We perform the procedure on a routine operating table using two leg holders, one below the foot and one against the thigh at the level of the tourniquet (Fig. 10–2). The leg holder below the foot should be positioned to maintain the knee flexed at 90° when the foot is resting on the leg holder and the knee flexed at 110° when the foot is placed below the leg holder.
Approach
It is important to maintain proper visualization throughout the procedure to optimize implant positioning even when using a minimally invasive technique. Therefore, the length of the skin incision varies from 8 to 10 cm depending on skin elasticity and patient morphotype. Sufficient visualization is required throughout the procedure and can be achieved by frequent extension-flexion manipulations to preferentially visualize either the femoral side or the tibial side. The upper limit of the incision is the superior pole of the patella, and the incision extends distally either toward the medial side of the tibial tuberosity for a medial UKA or toward the lateral side of the tibial tuberosity for a lateral UKA, ending 2 cm under the joint line previously located (Fig. 10–3). The proximal part of the incision is more essential for the procedure, and two thirds of the incision should be located above the joint line. For the medial UKA, a medial parapatellar approach is performed, extended proximally 1 or 2 cm in the quadriceps tendon. Once the synovial cavity is opened, the part of the fat pad in the way of the condyle is excised to properly visualize the condyle, the ACL and the corresponding tibial side of the tibial plateau. It is important to note that the principles of ligament balancing existing in TKA cannot be applied to UKA because the collateral ligaments should not be released in UKA. To protect the collateral ligament and safely perform the cuts, a dedicated curved, thin Hohmann retractor is placed on the medial or lateral side of the incision.
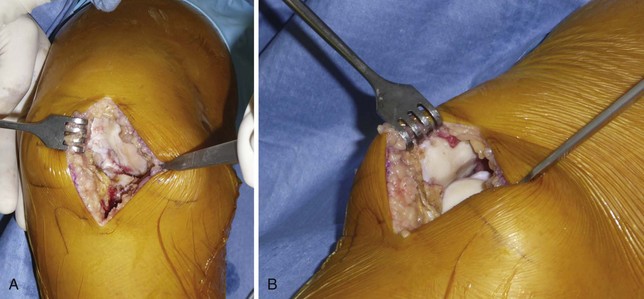
Before proceeding to the bone cuts, the first step is to bring the knee to 60° of flexion to evaluate the joint by checking the resistance of the ACL with an appropriate hook and evaluating the state of both the opposite tibiofemoral joint and the patellofemoral joint (Fig. 10–4). The osteophytes are then removed on the medial femoral condyle, after which a relative lengthening of the medial collateral ligament and capsule is performed, allowing passive correction of the deformity. Then, osteophytes located in the intercondylar notch should also carefully be removed to avoid late impingement with the ACL on the notch (Fig. 10–5). This point is very important to preserve the ACL and avoid any so-called Marie-Antoinette effect related to the osteophytes developed in the intercondylar notch, which have a guillotine-like effect on the ACL.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree