Fig. 5.1
Abduction stress testing of the UCL. This is performed with stabilization of the humerus and applying a valgus-directed force to the elbow. The elbow flexed to 20–30°, and a valgus stress applied to the elbow with the patient’s handheld between the examiner’s arm and body. A positive test is when there is increased laxity and may be associated with pain and/or lack of firm endpoint [5, 18] (Courtesy of Marc Safran, MD, Redwood City, CA)

Fig. 5.2
The modified milking maneuver. The patient’s arm is adducted and externally rotated. One hand of the examiner stabilizes the patient’s elbow while also palpating the medial joint line. The patient’s elbow is then flexed to 70° and a valgus stress applied by pulling on the patient’s thumb with the contralateral hand. The examiner can then assess joint line gapping and quality of the end point and compare to the contralateral elbow (Courtesy of Marc Safran, MD, Redwood City, CA)
Fig. 5.3
The moving valgus stress test. O’Driscoll described the moving valgus stress test [19], which places the patient’s shoulder in 90° of abduction and external rotation. A constant, valgus force is applied to the elbow in full flexion, and then the elbow is extended. A positive test is when the patient complains of maximum elbow pain between 70 and 120 degrees of elbow flexion (Courtesy of Marc Safran, MD, Redwood City, CA)
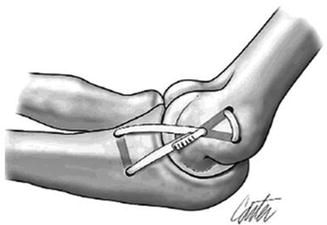
Fig. 5.4
The original figure-of-eight UCL reconstruction technique as developed by Jobe et al. describes transection and subsequent reflection of the flexor-pronator mass of the medial epicondyle and a figure-of-eight graft weave through drill holes in the humerus and ulna, followed by a submuscular ulnar nerve transposition (From Shah et al. [54]; with permission)
Fig. 5.5
The docking UCL reconstruction technique as developed by Altchek. The two ends of the tendon graft are docked into a single blind-ended humeral tunnel, and the sutures are tied over a humeral bone bridge (From Shah et al. [55]; with permission)
Concomitant injuries (such as medial epicondylosis, flexor-pronator mass avulsion, and cubital tunnel syndrome) should always be evaluated and are addressed later in this chapter.
Plain radiographs should initially be obtained and should include anteroposterior (AP) and lateral views. In acute injury, an avulsion fragment may be visible, and in chronic injury, loose bodies, osteophytes of the radiocapitellar and/or ulnohumeral joints, or ossification of the UCL may occur. Stress radiographs of the elbow can also be obtained to assess for widening of the medial joint line. They can be obtained either through manual stress or through commercial devices that apply a uniform force.
Magnetic resonance imaging (MRI) and MR arthrogram of the elbow have emerged as the most sensitive and specific imaging modality for identifying complete and partial UCL tears. MRI is 57–79 % sensitive and 100 % specific for UCL tears [18, 20]. MR arthrogram is 97 % sensitive for UCL tears and is the senior author’s study of choice for suspected UCL tears following completion of plain radiographs [21].
5.2.1 Treatment Options and Results
The initial treatment of UCL injuries includes rest, icing, activity modification, nonsteroidal anti-inflammatory medications, bracing, and physical therapy. Physical therapy should focus on reducing elbow pain and inflammation while also addressing any deficits identified along the throwing kinetic chain, which permits the best chance for successful elbow rehabilitation [22]. After inflammation is reduced and range of motion normalized, strengthening of the wrist and elbow muscles is initiated, followed by a throwing program for gradual return to throwing.
UCL reconstruction is currently the best surgical choice for both acute and chronic UCL ruptures. Indications for reconstruction include (1) acute ruptures in high-level throwers, (2) significant chronic instability, (3) insufficient UCL tissue remaining after UCL debridement for calcifications, and (4) recurrent pain and subtle valgus instability with throwing after supervised rehabilitation [23]. Reconstruction is performed using a free tendon (either autograft or allograft) and tensioning it between the medial humeral epicondyle and the sublime tubercle. Multiple techniques have been described starting with Frank Jobe in 1974 and its subsequent modifications [18, 21, 24–26].
5.2.2 Pearls and Pitfalls of Treatment
The probability of return to sports at the same preinjury level following UCL rupture treated nonoperatively is low (42 % in one study) for overhead athletes. Therefore, for a high-level competitive thrower, surgical reconstruction is usually advocated, as the time to failed nonoperative treatment may be up to 6 months, followed by 12–18 months of postoperative rehabilitation, resulting in up to 2 years time away from sports. Watson et al. in 2014 performed a systematic review comparing the Jobe, modified Jobe, docking, and modified docking techniques of UCL reconstruction [27]. In 1,368 patients, overall results demonstrated a return to play rate of 78.9 %.
5.3 Valgus Extension Overload Syndrome
Athletes with valgus extension overload primarily complain of posterior or posteromedial elbow pain. This is sometimes associated with clicking, grating, or locking if loose bodies are present. The pain is often accentuated during the late acceleration and follow-through phases of throwing, in which the elbow is near full extension [15]. Loose bodies may create temporary locking with a mechanical block to motion, which produces a synovitis that may result in an effusion. On physical examination, palpation may reveal tenderness along the posterior border of the olecranon, and forced extension or applying valgus force against an extended elbow may reproduce the patient’s symptoms.
Plain radiographs, including AP and lateral views of the elbow, are helpful for identifying loose bodies, osteophytes, or enlargement of the olecranon. A flexion-axial radiograph can be obtained that may demonstrate posteromedial olecranon osteophytes [14]. A computed tomographic (CT) scan or CT arthrogram may be better at demonstrating both osteophytes and loose bodies present within the elbow.
5.3.1 Treatment Options and Results
Nonoperative treatment should be considered for the early phase of treatment, especially in the absence of loose bodies. The emphasis should initially focus on reducing pain and inflammation. The second phase of treatment should then focus on improving the functional strength of the elbow followed by a progressive throwing program.
Operative treatment is indicated when conservative treatment fails or for those patients who have loose bodies or persistent symptoms which may be caused by chronic valgus instability [16]. Elbow arthroscopy has replaced arthrotomy as the preferred treatment for removing loose bodies and impinging osteophytes. It has low complication rates while allowing earlier and more aggressive rehabilitation and return to sport [28–30].
5.3.2 Pearls and Pitfalls of Treatment
In the setting of UCL insufficiency, a high reoperation rate of up to 41 % has been found when isolated loose body removal or osteophyte resection has been performed [28]. This is felt to be due to either removal of the osteophyte (1) increases the stresses to the UCL or (2) reveals attenuated/damaged UCL. Therefore, we suggest that careful consideration be given to UCL evaluation for the potential UCL reconstruction in combination with debridement in high-level overhead athletes. Additionally, in the light of unclear evidence regarding how much posteromedial olecranon can be safely resected, we advocate that debridement be limited to removal of the impinging osteophyte, leaving the normal olecranon intact.
5.4 Medial Epicondylosis and Flexor-Pronator Tears
Medial epicondylosis, or golfer’s elbow, is a tendinosis primarily involving the origin of the pronator teres (PT) and flexor carpi radialis (FCR) muscles and, occasionally, the tendon of flexor carpi ulnaris (FCU) [31]. Patients will often present with medial-sided elbow pain and can be accentuated during the early acceleration phase of throwing [32]. There may be a history of acute trauma which may result in an avulsion of the flexor-pronator mass; however, the most common presentation is of an insidious onset [33].
Physical examination may include swelling of the flexor-pronator mass, as well as tenderness over the distal, anterior, and lateral aspect of the medial epicondyle. These patients may have pain with resisted wrist flexion and forearm pronation, in addition to grip weakness relative to the contralateral extremity [34]. It is important to examine for ulnar nerve symptoms, as nearly 60 % of athletes with medial epicondylosis also have ulnar neuropathy [35, 36]. Plain radiographs are usually normal in this condition. MRI remains the best imaging modality for radiographic diagnosis and remains the standard of care [33].
5.4.1 Treatment Options and Results
Nonsurgical management is the mainstay of treatment and emphasizes rest, activity modification, icing, and oral anti-inflammatories. Local corticosteroid injections, extracorporeal shock wave therapy, and dry needling have all been utilized to varying success [33, 37–41]. Once the acute inflammatory symptoms have subsided, the athlete should be placed in a rehabilitation program that emphasizes flexor-pronator mass stretching and strengthening. It should be noted that most patients (85–90 %) improve with nonsurgical management [35–37, 42].
If symptoms persist past 4–6 months of appropriate, conservative management, then surgical options can be considered. Surgery involves release of the flexor-pronator origin, excision of the friable granulation tissue, stimulation of bleeding from the medial epicondylar bone, and repair/reconstruction of the medial musculature [43, 44].
5.4.2 Pearls and Pitfalls of Treatment
The exception to initial nonsurgical management is in elite athletes with a demonstrated full-thickness tear of the flexor-pronator mass seen on MRI [38]. During surgical intervention for medial epicondylosis, the UCL must be identified and protected. It lies just deep and is adherent to the flexor-pronator muscle group and serves as a partial origin for one of the muscles. In patients with medial epicondylosis and associated ulnar neuropathy, surgical management has not been shown to be as effective as those without neuropathy [45].
5.5 Cubital Tunnel Syndrome
The ulnar nerve is most commonly injured around the elbow, likely due to its superficial location in the subcutaneous tissue, as well as the relatively tight path it follows when it courses around the medial aspect of the elbow. In throwers, the physical examination for cubital tunnel syndrome does not have the classic presentation – they will usually only be symptomatic while throwing.
Radiographs of the elbow may identify potential bony sources of ulnar nerve compression, and MRI may evaluate for soft tissue masses that may cause nerve compression [46]. Electrodiagnostic testing including electromyography (EMG) may be helpful in identifying cases of advanced neuropathy; however, negative testing does not exclude the diagnosis of ulnar neuropathy [10].
5.5.1 Treatment Options and Results
For mild to moderate cases of ulnar nerve compression, nonoperative treatment should be the initial management. This includes rest, activity modification, and nonsteroidal inflammatory medication [13].
Failure of conservative treatment necessitates surgical intervention. Multiple surgical options exist, including in situ decompression, medial epicondylectomy, and anterior transposition (subcutaneous, submuscular, or intramuscular).
A meta-analysis of four randomized, controlled trials comparing in situ decompression to anterior transposition involving 335 patients found no difference in motor nerve conduction studies or clinical outcome scores between the two groups [47–51]. The authors concluded that in situ decompression of the ulnar nerve is a reasonable alternative to anterior transposition. However, in throwing athletes, the senior author prefers subcutaneous transposition to reduce the risk of ulnar nerve subluxation and, for contact athletes, a submuscular transposition to reduce the risk for injury due to direct contact.
5.5.2 Pearls and Pitfalls of Treatment
During the initial physical examination, close attention should be paid to differentiating ulnar nerve subluxation from snapping triceps syndrome. Failure to identify the latter prior to performing cubital tunnel release may lead to failed surgery [52]. Ulnar neuritis often occurs concomitantly with, or is a result of, valgus elbow instability; thus, it is important to recognize and treat the associated pathology. Finally, intraoperative care and time should be taken to ensure that all potential sites of ulnar nerve compression are adequately released. Persistent ulnar nerve symptoms postoperative are most commonly due to incomplete decompression [53].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








