Medial Patellofemoral Ligament Reconstruction Using the Quadriceps Tendon
William L. Hennrikus
Jay Albright
INDICATIONS AND CONTRAINDICATIONS
Many surgical procedures have been described for treatment of recurrent patella instability. The surgical approach should be individualized for each patient and should address the pathoanatomy contributing to the repeat dislocations. Often, combinations of procedures are needed to correct all patellofemoral problems. Surgical options for patellofemoral instability in adolescents include proximal realignment, distal realignment, lateral release, medial plication, medial patellofemoral ligament (MPFL) reconstruction, guided growth with tension band plates, rotational osteotomies for femoral anteversion or tibial torsion, and combinations of the above procedures. Osteotomies of the proximal tibia or distal femur are reserved for older teenagers who have demonstrated closure of the growth plates.
The goal of MPFL reconstruction is to reestablish the normal checkrein against lateral motion of the patella. When reconstructing the MPFL, it is important to replicate the native anatomy. In most chronic cases, reconstruction is recommended rather than MPFL repair because the chronically injured medial retinacular tissues are usually insufficient to reestablish the normal tether to prevent lateral dislocation. Multiple graft choices have been utilized for MPFL reconstruction including hamstrings, patellar tendon, adductor magnus, allografts, and the quadriceps tendon. Surgical treatment of patellofemoral instability in the adolescent patient has evolved from nonanatomic extensor mechanism realignment procedures such as the Galeazzi procedure to anatomic restorative procedures based on reconstitution of the MFPL. The MPFL is the primary restraint to patellofemoral instability at 0 to 30 degrees of flexion and overall provides greater than 50% of the medial restraint of the patella.
Isolated MPFL reconstruction may not be sufficient to prevent recurrent dislocation if other risk factors such as patella alta, patella tilt, an increased Q angle, a tibial tuberosity-trochlear groove distance of more than 20 mm, or trochlear dysplasia are also present. Treatment of the other risk factors can be combined with an MPFL reconstruction.
Indications for surgical treatment of patella instability in the child and adolescent include repeat patella dislocations that have failed nonoperative treatment. The essential lesion in chronic lateral patellofemoral instability is insufficiency of the MPFL. The ideal indications for an isolated MPFL reconstruction in a child or adolescent would be a recurrent lateral patella dislocation without valgus malalignment, patella alta, or trochlear dysplasia.
Acute patellofemoral dislocation is the most common knee disorder in children and adolescents. Nonoperative management of a first-time traumatic dislocation is recommended except when there is an osteochondral fracture, an avulsion of the vastus medialis obliquus muscle, or additional intraarticular injuries such as a meniscal tear. In these cases, arthroscopic-assisted treatment of the specific injury is addressed. In the setting of recurrent instability that has failed conservative treatment, surgical reconstruction of the MPFL is recommended. MPFL reconstruction using the quadriceps tendon is a prudent alternative for chronic patellofemoral instability in the skeletally immature patient. The technique is simple and safe, avoids drill holes in the patella and femur, and therefore minimizes the risk of patella fracture of physeal injury.
PREOPERATIVE PREPARATION
Careful preoperative clinical evaluation includes measurement of the Q angle, tibial torsion, femoral torsion, ligamentous laxity, gait, and range of motion. Pre-op AP, lateral, and sunrise radiographs of the injured knee are recommended. An MRI scan of the injured knee and a left hand and wrist bone age are indicated on a case-by-case basis. If an MRI is obtained, the tibial tubercle to trochlear groove distance (TT-TG) is measured.
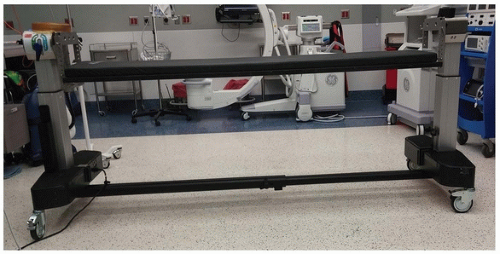
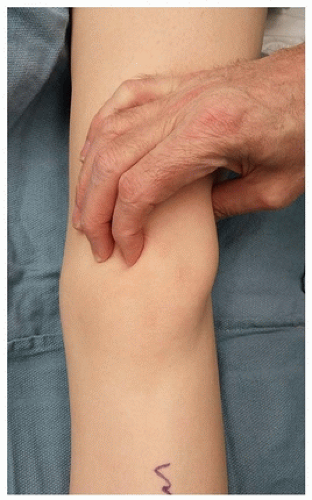
The operation should be performed with the patient under general anesthesia and in the supine position. A radiolucent OR table (Fig. 35-1) is used with the C-arm positioned on the opposite side of the injured extremity. A thorough examination under anesthesia is performed to confirm incompetence of the MPFL. Lateral translation of the patella is assessed with the knee at 0 degrees and 30 degrees of flexion (Fig. 35-2). Greater than 50% lateral translation of the patella is diagnostic of MPFL rupture; in the illustrated case, the patella could be completely dislocated (Fig. 35-3). Assessment of a tight lateral retinaculum is also assessed to determine the need for a lateral release.
PREOPERATIVE PLANNING
OR table: OSI flat top
Position/positioning aids: Supine, radiolucent triangle under knee
Fluoroscopy location: Opposite the side of the injured extremity
Equipment: Basic arthroscopy set, basic orthopedic set, K-wires, 2.5-mm bioabsorbable suture anchor with 3-mm FiberWire suture, no. 2 Ethibond sutures, radiolucent triangle
Tourniquet: Nonsterile
Other: Knee immobilizer for postoperative care
SURGICAL PROCEDURE
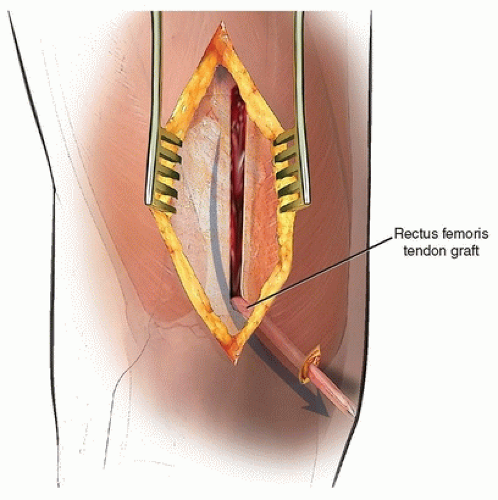
For the adolescent athlete with recurrent patella dislocations, we prefer an anatomic MPFL reconstruction using the medial quadriceps tendon. This technique avoids injury to the growth plates and is particularly applicable to the skeletally immature pediatric and adolescent athlete. This technique is a combination of previously described techniques by Noyes, Steenson, and Goyal. An 8-mm by 70-mm full-thickness strip of medial quadriceps tendon is used to reconstruct the MPFL. The quadriceps graft is left attached to the superior medial border of the patella. The free end of the graft is passed between the synovium and the retinaculum and is sutured to the medial intermuscular septum adjacent to the medial femoral epicondyle (Figs. 35-4 and 35-5). Femoral fixation is augmented with a small absorbable suture anchor placed via C-arm direction to ensure accurate placement of the graft. The remaining medial retinaculum is imbricated when the quadriceps tendon harvest site is closed. This technique avoids large patella and femoral drill holes and minimizes the risk of patella fracture or injury to the distal femoral physis. The graft is tensioned at 30 to 45 degrees of knee flexion. A lateral release is added if tightness of the lateral retinaculum prevents normal medial patella translation or in cases of abnormal patella tilting.
The goal of MPFL reconstruction is to replace the torn ligament with a graft that is stronger than the native MPFL and with a tension similar to the native ligament. Normal patella motion allows about two patella quadrants of lateral translation. Graft tensioning should be performed with the knee in about 30 to 45 degrees of knee flexion. In addition, we use the C-arm to help locate the femoral attachment site. Schottle and Redfern have described radiographic landmarks to locate the anatomic femoral position of the MPFL. “Schottle point” is a reproducible anatomic and radiographic
landmark 2 mm anterior the posterior cortex of the femur, 2 mm distal to the posterior origin of the medial femoral condyle, and just proximal to Blumensaat line. The femoral attachment site is key for achieving a good outcome. In skeletally immature patients, the relationship of the MPFL origin to the distal femoral physis has been controversial. However, in a recently published study using skeletally immature cadaver specimens, Farrow demonstrated that the anatomic site for the femoral attachment of the MPFL lies a few millimeters distal to the medial aspect of the distal femoral physis. Steensen and Stephen, in another elegant cadaver study, demonstrated that the position of the MPFL graft femoral attachment substantially influenced the graft length change pattern. The patella attachment site, on the other hand, had little effect. The most common error in graft placement is to fix the graft too far anteriorly on the femur, which may lead to graft laxity in extension and graft tension in flexion. This graft malposition can lead to overloading of the medial patellofemoral cartilage, anterior knee pain, and loss of flexion. In addition, a nonanatomic MPFL femoral attachment site can result in a high rate of recurrent patella dislocation following MPFL reconstruction. An overtightened graft can combined with a lateral release can result in iatrogenic medial patella subluxation in flexion. After graft fixation, knee motion should be equal to the opposite knee and there should be a good endpoint to lateral patella translation from zero to 30 degrees of knee flexion.
landmark 2 mm anterior the posterior cortex of the femur, 2 mm distal to the posterior origin of the medial femoral condyle, and just proximal to Blumensaat line. The femoral attachment site is key for achieving a good outcome. In skeletally immature patients, the relationship of the MPFL origin to the distal femoral physis has been controversial. However, in a recently published study using skeletally immature cadaver specimens, Farrow demonstrated that the anatomic site for the femoral attachment of the MPFL lies a few millimeters distal to the medial aspect of the distal femoral physis. Steensen and Stephen, in another elegant cadaver study, demonstrated that the position of the MPFL graft femoral attachment substantially influenced the graft length change pattern. The patella attachment site, on the other hand, had little effect. The most common error in graft placement is to fix the graft too far anteriorly on the femur, which may lead to graft laxity in extension and graft tension in flexion. This graft malposition can lead to overloading of the medial patellofemoral cartilage, anterior knee pain, and loss of flexion. In addition, a nonanatomic MPFL femoral attachment site can result in a high rate of recurrent patella dislocation following MPFL reconstruction. An overtightened graft can combined with a lateral release can result in iatrogenic medial patella subluxation in flexion. After graft fixation, knee motion should be equal to the opposite knee and there should be a good endpoint to lateral patella translation from zero to 30 degrees of knee flexion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree