Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Instability
Introduction
Recent emphasis on additional soft-tissue restraints including medial quadriceps tendon femoral ligament (MQTFL), medial patellotibial ligament (MPTL), and medial patellomeniscal ligament (MPML)
MPFL reconstruction is performed to restore patellar stability
Patient Selection
Indications
Symptomatic recurrent patellar instability with medial soft-tissue insufficiency
Indicated as a concomitant procedure when bony procedures alone do not restore functional stability
Patient apprehension with lateral translation on physical examination; best candidates are those who report recurrent painful episodes of lateral subluxation or dislocation associated with twisting mechanism
Contraindications
Medial patellar instability due to
Iatrogenic overaggressive lateral retinacular release
Hyperlaxity syndromes
Skeletal immaturity requires modification of procedure
Active infection
Preoperative Imaging
Radiography
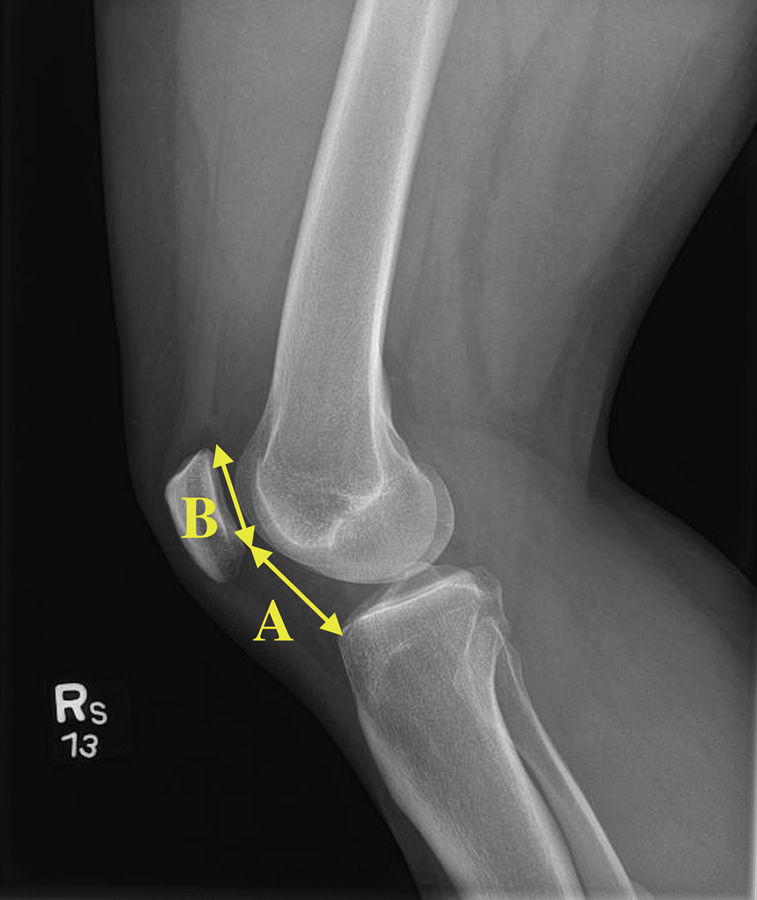
Figure 1The lateral radiograph is used to determine relative patellar height. The Caton-Deschamps index is a measurement of patellar height, calculated by dividing the distance from the inferior articular pole of the patella to the anterior margin of the tibia (A), by the articular length of the patella (B).
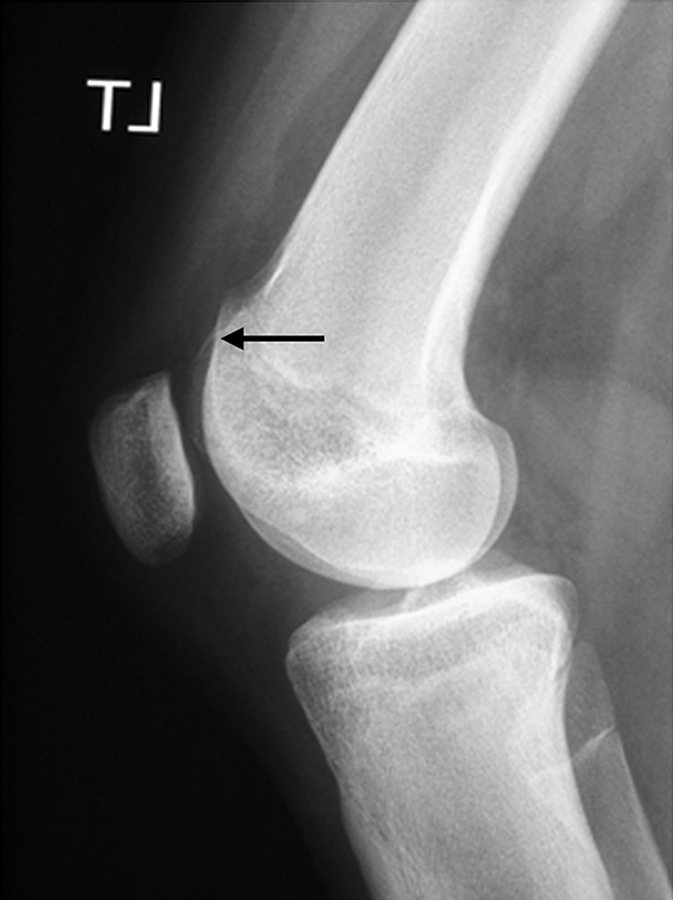
Figure 2Lateral radiograph of a knee shows the “crossing sign” (arrow), indicative of trochlear dysplasia.
Standard AP, notch view, PA in 45° (the latter only in suspected tibiofemoral osteoarthritis)
Lateral at 30° flexion
Used to quantify patellar height using Caton-Deschamps index (Figure 1); surgeon can perform distalizing tibial tuberosity osteotomy to correct extreme patella alta
Can identify trochlear dysplasia as “crossing sign” (Figure 2)
Sunrise view at 45°—May suggest need for an anteromedializing osteotomy to reduce reactive joint forces in those with arthritic patellofemoral joint
Magnetic Resonance Imaging
Can assess integrity of articular surfaces
May lead to additional procedures if necessary, including
Cartilage débridement, marrow stimulation, osteochondral replacement procedures
For lateral patellofemoral lesions—Medialization osteotomy (eg, Elmslie-Trillat) to unload lateral patellofemoral joint
For inferior pole patella lesions—Unload inferior pole with osteotomy (eg, Fulkerson anteromedialization osteotomy)
Computed Tomography
Determine trochlear morphology, measure malalignment
Measure tibial tuberosity–trochlear groove distance on superimposed axial CT cuts at Roman arch and proximal tibia at level where tuberosity is most prominent
Dynamic CT can quantify amount of maltracking and determine flexion angle where lateral translation of the patella is greatest
Procedure
Patient Positioning/Examination Under Anesthesia
Supine position
Examination under anesthesia
Assess limb alignment, hip rotation; perform knee ligament evaluation
Glide test assesses amount of lateral translation of patella; quantified in quadrants; compare with contralateral knee
Tilt test determines tightness of lateral retinaculum
Surgical Technique
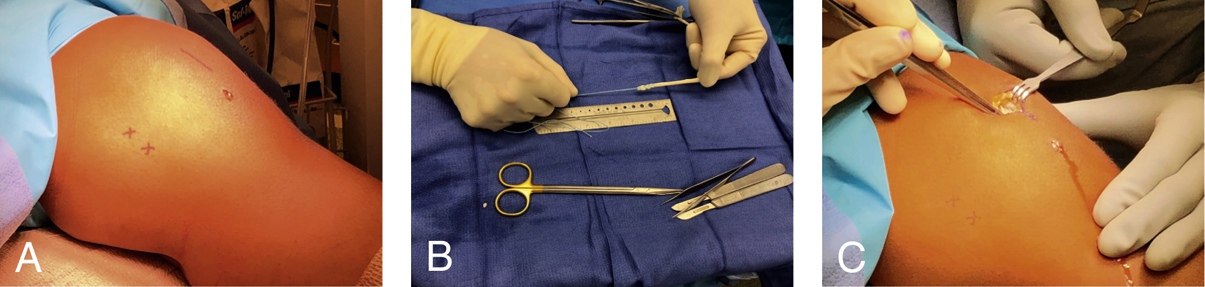
Figure 3Intraoperative photographs of medial patellofemoral ligament (MPFL) reconstruction. A, Bony landmarks are marked on the surface of the skin. The proximal X is over the adductor tubercle, and the distal X is over the medial femoral epicondyle. B, A locking stitch is woven through the patellar end of the graft. C, An incision is made along the medial border of the patella.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


