This review discusses challenges faced by clinicians and researchers when measuring ambulation in individuals with central neurologic disorders within 3 distinct environments: clinical, laboratory, and community. Even the most robust measure of ambulation is affected by the environment in which it is implemented and by the clinical or research question and the specificity of the hypothesis being investigated. The ability to accurately measure ambulation (one of the most important metrics used to show transition into a community environment) is essential to measure treatment effectiveness and rehabilitation outcomes in populations with central neurologic disorders.
Key points
- •
Examine strategies for appropriate measurements of ambulation in individuals with central neurologic disorder within three distinct environments: 1) clinical; 2) laboratory; and 3) community.
- •
Discuss common challenges and solutions for clinicians and researchers when selecting appropriate outcomes for measuring ambulation.
- •
Description of technology-driven assessment tools for measuring ambulation to obtain objective, quantifiable outcomes.
- •
Explore techniques and research related to measurement of quantitative and qualitative ambulation in the community for persons with central neurologic disorder.
Introduction
Throughout rehabilitation medicine, there is an emphasis on the ability to ambulate as a functional outcome and as an overall indicator of quality of life. When ambulation is affected by central neurologic disorders (CND), it is typically as a result of a combination of impairments and the compensatory strategies used to accommodate these impairments. Pathologic ambulation can result from impairments within a single system or within a combination of systems, such as musculoskeletal, neuromuscular, sensory/perceptual, and cognitive/behavioral.
Functional ambulation is the extent to which an individual is capable and willing to move around in their environment. Measuring ambulation is a complex task involving clinical expertise, laboratory technology, and the ability to translate information to a community setting.
Measuring ambulation can be challenging, because walking occurs in multiple environments and must be assessed at multiple time points to indicate improvement or decline. There is an added complexity, because, in a traditional clinical environment, a single numerical value or scale score is preferred to summarize a series of complex movements, whereas in a laboratory environment, researchers typically prefer quantifiable continuous data, which allow for complex analysis of multiple outcome variables. Measuring ambulation in a community also presents unique challenges and often requires a combination of strategies to obtain valid outcomes. This review examines strategies for appropriate measurements of ambulation in individuals with CND within 3 distinct environments: (1) clinical, (2) laboratory, and (3) community. The purpose of this article is not to provide an exhaustive list of the measures that can be used to assess ambulation but rather to describe the most frequently used measures and to discuss common challenges faced by clinicians and researchers in establishing an accurate picture of an individual’s ability to ambulate.
Introduction
Throughout rehabilitation medicine, there is an emphasis on the ability to ambulate as a functional outcome and as an overall indicator of quality of life. When ambulation is affected by central neurologic disorders (CND), it is typically as a result of a combination of impairments and the compensatory strategies used to accommodate these impairments. Pathologic ambulation can result from impairments within a single system or within a combination of systems, such as musculoskeletal, neuromuscular, sensory/perceptual, and cognitive/behavioral.
Functional ambulation is the extent to which an individual is capable and willing to move around in their environment. Measuring ambulation is a complex task involving clinical expertise, laboratory technology, and the ability to translate information to a community setting.
Measuring ambulation can be challenging, because walking occurs in multiple environments and must be assessed at multiple time points to indicate improvement or decline. There is an added complexity, because, in a traditional clinical environment, a single numerical value or scale score is preferred to summarize a series of complex movements, whereas in a laboratory environment, researchers typically prefer quantifiable continuous data, which allow for complex analysis of multiple outcome variables. Measuring ambulation in a community also presents unique challenges and often requires a combination of strategies to obtain valid outcomes. This review examines strategies for appropriate measurements of ambulation in individuals with CND within 3 distinct environments: (1) clinical, (2) laboratory, and (3) community. The purpose of this article is not to provide an exhaustive list of the measures that can be used to assess ambulation but rather to describe the most frequently used measures and to discuss common challenges faced by clinicians and researchers in establishing an accurate picture of an individual’s ability to ambulate.
Measuring ambulation in the clinical environment
In a clinical environment, it is important to select measures that can evaluate changes in impairment, function, and performance. Test selection is often dependent on nonclinical criteria such as cost, time to administer, and available equipment. It is also important for the patient to understand the test instructions, because unfamiliarity with the test can alter performance and outcomes. Some examples of typical clinical assessments commonly used for measuring ambulation can be found in Table 1 .
| Name of Scale | Description | Measurement |
|---|---|---|
| Functional Independence Measure | A 7-level ordinal scale that describes stages of complete dependence to complete independence in performance of basic activities of daily living | Ordinal scores based on clinical observation |
| Fugl-Meyer Motor Assessment | Evaluates movement, reflexes, coordination, and speed, derived from the Brunnstrom stages of poststroke recovery. Frequently used to measure motor deficits | Ordinal scores are based on clinical observation and observed movements |
| Ambulation Index | An ordinal rating scale designed to assess independent mobility by evaluating the time and degree of assistance required to walk 7.62 m (25 ft). The scale ranges from 0 (asymptomatic and fully active) to 9 (restricted to wheelchair; unable to transfer independently) | Ordinal scores are based on clinical observation, including observed performance, and timed walking speed |
| Emory Function Ambulation Profile, Modified Emory Functional Ambulation Profile | The time (s) to ambulate through 5 common environmental terrains with or without an assistive device or manual assistance | The sum of the time (s) required to complete the 5 tasks |
| Walking Tests (2-minute, 6-minute, 10-minute, and 12-minute) | Distance walked in meters in a given time is measured to indicate performance | Distance walked (m) |
| Dynamic Gait Index | A tool to assess gait, balance, and fall risk. Eight abilities are graded on a 4-point scale (0–3) from normal performance to severely impaired. The rating is based on the individual’s ability to maintain a healthy gait pattern and pace, without deviating or stumbling | Ordinal scores are based on clinical observation and observed performance |
| Timed Up and Go | The time (s) required to rise from an arm chair, walk 3 m, turn, walk back, and sit down again | A categorical scale based on the time (s) required to accomplish the described task |
| 10-m Walk Test, Timed 7.62 m (25-ft) Walk Test | A measure of ambulation capacity including the time (s) to walk 10 m or 7.62 m (25 ft) at maximum but safe gait speed | Time and distance to calculate maximum gait speed (m/s) |
| Gait Speed | The rate (s) a given distance (m) is covered to determine self-selected or fastest gait speed | Time and distance to calculate speed (m/s) |
The Functional Independence Measure (FIM) was designed to measure burden of care in multiple rehabilitation populations. The scores are based on clinical observation of 18 items of activities of daily living (ADLs) (13 motor and 5 cognition items). Although there are motor items associated with this measure (including 1 item labeled locomotion and 1 labeled stairs), the overall FIM score is often not sensitive enough to reflect improvements in ambulation (particularly in situations in which walking performance has improved without a change in the level of assistance needed). Previous research also revealed a ceiling effect, and the FIM shows poor sensitivity to change in individuals with better walking abilities. The FIM is typically used to determine independence at admission and discharge from inpatient rehabilitation. Another example of a frequently used clinical measure of motor deficits is the Fugl-Meyer Motor Assessment, which has previously been shown to correlate with length of stay in inpatient rehabilitation, and has been found to be predictive of discharge FIM scores and performance in ADLs. The disadvantage of this measure is that it assesses only gross limb movement and not fine or complex movements or coordination. Both the FIM and Fugl-Meyer Motor Assessment as a whole do provide reliable information about the results of rehabilitation, but it is difficult to specifically determine if, and how much, ambulation has improved using either of these assessment tools.
The Ambulation Index (AI) is an ordinal rating scale designed to assess independent mobility by evaluating the time and degree of assistance required to walk 7.62 m (25 ft), as well as the ability to transfer. Previous research has found the AI to be useful as a grouping variable when measuring ambulation in individuals with stroke. The measure is useful in rehabilitation medicine, but it is not sensitive enough to measure small changes in ambulation. Overall, the FIM, Fugl-Meyer, and AI measure impairment and function but have limited usefulness in describing and evaluating ambulation.
When measuring ambulation in a clinical environment, it is important to consider that individuals with CND may have difficulty adapting to the demands of walking in the community, such as rising from a chair, stepping over an obstacle, ascending stairs, and navigating various terrains. The challenge is to select tasks and terrains that mimic community ambulation that are easy to administer and provide relevant clinical information. The Emory Functional Ambulation Profile (EFAP) and the modified EFAP (mEFAP) were designed to provide quantitative information about ambulation by measuring the time to walk over a standardized array of community obstacles and surfaces, accounting for the use of assistive devices. The EFAP and mEFAP are reliable and valid clinical tests of ambulation that are sensitive to changes in ambulation speed. Research in individuals with stroke found that the mEFAP is sensitive to changes in gait function during inpatient rehabilitation and therefore could be used to supplement traditional subjective measures of clinical ambulation.
Walking tests measure the distance walked in a given amount of time to indicate walking performance. These tests are generally 2, 6, 10, or 12 minutes in duration and are widely used in clinical and research applications for individuals with CND. These measures are more quantitative and provide information directly related to ambulation, including walking endurance. Previous research in this area suggests that individuals must negotiate a distance of between 332 and 360 m to access goods and services in the community. Walking distance is therefore a key indicator of ambulation.
For individuals with CND, it is important to have clinical assessments that identify individuals who are at risk for falling and may benefit from interventions designed to improve balance. The Dynamic Gait Index (DGI) was developed as a clinical tool to assess an individual’s ability to modify gait in response to changing task demands. The limitation of the DGI is that scores are reduced for those individuals using an assistive device, regardless of performance. The DGI has been applied to individuals with CND as a reliable measure of dynamic balance and potential fall risk. The Timed Up and Go (TUG) is a screening test of balance that is commonly used to evaluate functional mobility. The time to complete the test is strongly correlated to the level of functional mobility. Adults who complete the TUG in less than 20 seconds are considered to be independent in transfer tasks associated with ADLs and can maintain walking speeds sufficient for community ambulation.
In individuals with CND, alterations in gait mechanics, strength, and balance have a direct effect on gait speed. The 10-m walk test and timed 7.62 m (25-ft) walk are measures of ambulation capacity in which gait speed is the primary outcome variable. These tests have been widely used in populations with CND and are easy to administer in a clinical environment. When measuring ambulation, it is important for clinicians to select measures capable of detecting changes that reflect real life function. Gait speed is an important and reliable measure of ambulation for individuals, because safe navigation of community crosswalks mandates that an individual be able to complete a prescribed distance in a defined time period. Previous research in stroke found that when an ankle foot orthotic was worn on the paretic limb, individuals gained the ability to modulate gait speed. The orthotic intervention provided individuals with stroke with the functional ability to increase speed in the community, which is essential for negotiating obstacles and safely crossing community streets. Gait speed is used in clinical and research applications as the hallmark of recovery, it is simple to implement, and it has robust psychometric properties. Several studies have provided evidence to support the predictive validity of gait speed, and it has been shown to be positively correlated with level of disability, function, and quality of life in individuals with stroke. However, what represents a clinically meaningful change in gait speed has not been defined in all patient populations.
Measuring ambulation in a laboratory environment
In a laboratory, ambulation is measured using traditional clinical assessments in conjunction with technology-driven mobility assessment tools, to create quantifiable outcomes that can be used to describe mechanisms that may lead to improved ambulation. For example, increased gait speed may indicate improved ambulation, but does not necessarily indicate improved gait mechanisms or functional recovery. The goals of laboratory-based outcomes for measuring ambulation are to enhance traditional clinical measures, or to become fully integrated into routine clinical care to help direct treatment options and accurately measure changes in ambulation throughout the rehabilitation process.
History and Evolution of Measuring Ambulation
Gait is the way ambulation is achieved using human limbs, and gait analysis is the systematic evaluation of a person’s walking pattern. The origins of the science of gait analysis began in the seventeenth century in Europe, when scientists and researchers provided a solid scientific foundation of our current knowledge and the understanding of human ambulation. Research in the twentieth century benefited from technological advancements, including the development of three-dimensional (3D) force plates, and kinesiological electromyography (KEMG), which moved the measurement precision of gait analysis significantly forward. A summary of the evolution of these early techniques into the systems used today is described in Table 2 .
| KEMG | J.R. Close, 1959 | Studied the phasic action of muscles using a 16-mm movie camera with a sound track and was able to record single-channel muscle action potentials on cine film |
| R.W. Vreeland and D.H. Sutherland, 1961 | Used a 16-mm movie camera mounted on a turntable above an oscilloscope with a 3-channel EMG | |
| J.V. Basmajian, 1962 | Developed the technique of inserting 2 very fine electrodes (50-μm) through a single small needle (fine-wire EMG) | |
| J.U. Baumann, 1974 | Obtained an 8-channel Honeywell tape recorder with 6 channels for KEMG transmitted through telemetry | |
| S.R. Simon, 1977 | Electromyography permitted simultaneous recording from 12 channels transmitted through a cable from subject to computer | |
| Current | Various commercially available multichannel surface and fine-wire EMG systems, including telemetered and wireless EMG capability and integrated software for comprehensive outcome analysis. Capable of measurements inside (clinical or laboratory) and outside (community) in various environments | |
| Kinematics | M.P. Murray, 1964 | Attached reflective targets to anatomic landmarks of subjects walking in illumination of strobe light |
| P.V. Karpovich and G.P. Karpovich, 1959 | Electrogoniometry | |
| R. Linder, 1965 | Vanguard motion analyzer: developed methods to measure yaw, pitch, and roll using mathematical formulae, 2 or more cameras and a two-dimensional coordinate system | |
| E.H. Furnee, 1967–1989 | Primas system: TV/motion analysis systems with automated recording of reflective marker positions | |
| Current | Multiple commercially available real-time optical motion capture systems with: (1) infrared HD cameras; (2) markerless motion capture; (3) active light-emitting diode technology; (4) wired and wireless systems and integrated software for comprehensive outcome analysis. Capable of measurements inside (clinical or laboratory) and outside (community) in various environments | |
| Kinetics | M. Carlet, 1872 | Developed and used air reservoirs to measure force applied to the heel and forefoot |
| E.J. Marey, 1894 | Developed first true force plate, which measured vertical component of ground reaction using a pneumatic mechanism | |
| J. Amar, 1916 | Produced the world’s first 3-component (pneumatic) force plate, Trottoire Dynamique | |
| J. Hawthorn, 1971 | Dynamic force plate (piezoelectric force transducers) | |
| Current | Several multichannel force (6° of freedom) and pressure measurements systems. Capable of measurement in various environments indoors, outdoors. and under water |
Although the early principles of gait analysis are recognized as the foundation of measuring ambulation, the methods used were too labor-intensive for practical application in a clinical setting. Technology-driven systems for measuring ambulation continue to evolve in the laboratory, with the goal of translating these outcome measures into the clinical and community setting.
Techniques for Measuring Ambulation in a Research Laboratory
Gait analysis is a widely used measurement technique to assess, plan, and treat individuals with conditions affecting their ability to walk. Gait analysis emerges from the combined interaction of the human eye (image capture) and the human brain (image processing) used for recognition and identification of changes in ambulation. A complete gait analysis can be achieved using visual observation to interpret human locomotion. Therapists frequently use observational gait analysis to evaluate patient ambulation, because instrumented measurement systems are not feasible during time-limited clinical visits. Observational gait analysis typically reveals compensations or impairments from underlying diseases but it is limited by the experience of the observer. Instrumented gait analysis is a more technical method that involves collection of quantifiable information through the use of cameras, force plates, electromyography (EMG), pressure sensors, and computer analysis to objectively measure an individual’s walking pattern. Quantitative state-of-the-art methods of analysis and equipment offer greater precision, specificity, and sensitivity to change. It is within the laboratory environment that the comparison of observational versus instrumented gait analysis must continue to be explored to advance clinical outcomes.
Healthy walking is the standard against which disease is measured. The key gait parameters that the clinician needs to compare against disease are described in Table 3 .
| Spatial-temporal characteristics | Spatial | Step length, stride length, step width, velocity, cadence |
| Temporal | IDS (initial double support time), SS (single support time), TDS (terminal double support time), swing time | |
| Symmetry | Temporal-spatial symmetry ratios between limbs | |
| Joint kinematics | Rotations | 3D joint angular rotations |
| Angular velocities | Rate of change of 3D joint angles | |
| Center of mass | Excursion of the 3D center of mass | |
| Joint kinetics | Forces | 3D joint forces (effect of ground reaction forces on joint motions) |
| Torques | 3D joint torques (a combination of joint rotations and forces) | |
| EMG | Muscle firing | EMG analysis to assess muscle activation patterns (timing and amplitude) as it relates to joint kinematics |
| Co-contraction | Simultaneous activation of agonist and antagonist muscles, if any | |
| Pedobarography | Plantar pressures | Measuring the magnitude and timing of pressure acting between the plantar surface of the foot and a supporting surface to quantify loading, weight transfer, and area during walking |
Measuring Ambulation Using Temporal-Spatial Characteristics
Temporal
Temporal parameters are calculated using the timing characteristics within a gait cycle, where each gait cycle is further divided into individual gait phases to make comparisons across several cycles. The complete gait cycle includes initial double support (the time between foot contact and contralateral toe off), single support (the time between contralateral toe off and contralateral foot contact), terminal double support (the time between contralateral foot contact and ipsilateral toe off), and swing (the time between ipsilateral toe off and ipsilateral foot contact).
Spatial
Spatial parameters are measured using the linear measurements (displacement of markers) during a gait cycle. They include step length (the forward linear distance between the heel markers from foot contact to subsequent contralateral foot contact), stride length (the forward linear distance between the heel markers from foot contact to ipsilateral foot contact), and step width (the linear medial-lateral distance between heel markers from foot contact to contralateral foot contact).
Symmetry
Symmetry measures are used to compare characteristics between the limbs. Temporal-spatial gait symmetry indices are calculated using mean swing (seconds) and stance times (seconds) on both limbs to calculate the following variables: overall temporal symmetry; temporal swing symmetry; temporal stance symmetry; temporal swing stance symmetry; and spatial step symmetry (the ratio of step lengths on both limbs in millimeters). A normative range for temporal-spatial symmetry is assumed to be 0.9 to 1.1. This technique has been effectively used in stroke to assess the behavior of the paretic and nonparetic limbs during gait, where an overall temporal symmetry value greater than 1 indicates a preference to rely on the nonparetic limb during walking.
Quantifying Ambulation with Kinematic and Kinetic Analysis
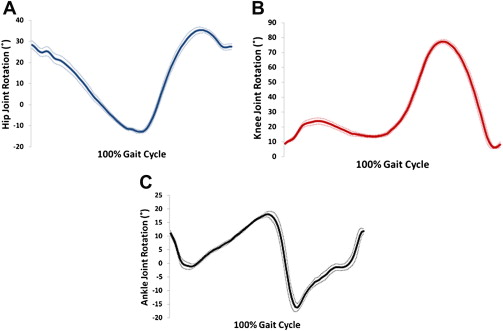
Kinematic
Kinematic data consist of temporal, linear, and angular variables. They quantify the features of gait describing the movements of the body segments and joint angles: temporal (timing), linear (displacement), and angular measurements. Temporal data describe the stride duration and the limb coordination patterns. Distance data, computed from the coordinates of the markers, describe the stride length, the distances between limb placements, and the flight paths of the body parts. Angular data describe the displacements, velocities, and accelerations of the body segments and joints. Kinematic output from the motor control system is useful for measuring the movement variance during walking and helps to classify gait diseases. Fig. 1 shows sagittal plane joint angles at the hip, knee, and ankle during healthy walking.