Many people with multiple sclerosis MS (PwMS) have impaired balance and walking, and fall frequently. High-quality measures of imbalance and fall risk are essential for identifying who may benefit from interventions to improve balance and prevent falls, and for selecting the most appropriate interventions. We recommend the International Classification of Functioning, Disability and Health (ICF) model. Many measures are available to assess factors affecting balance, fall risk, and walking at the different levels of the ICF. Combining these measures provides the most complete assessment of the individual and the best guidance for interventions by the health care team.
Key points
- •
Impaired balance and walking are common in people with multiple sclerosis (MS).
- •
The International Classification of Functioning, Disability and Health provides an ideal framework for organizing the examination and assessment of imbalance, fall risk, and impaired walking in people with MS.
- •
Balance and fall measures make important contributions in directing therapeutic interventions and potentially for assessing the effectiveness of both disease-modifying and symptomatic interventions.
Introduction
Multiple sclerosis (MS) is the most common nontraumatic neurologic disease of young adults. Worldwide, approximately 2.5 million people are diagnosed with MS. MS is characterized by variable neurologic symptoms, disease activity, and progression of functional limitations over time. Many people with MS (PwMS) report that ambulation is affected by their disease. PwMS walk more slowly than healthy controls and their balance is also impaired compared with healthy controls. PwMS also fall frequently. Even before walking is slowed, PwMS have balance impairments, which can be detected by clinical and instrumented measures. The focus of this article is the measurement and treatment of imbalance and fall risk in PwMS.
Balance measures can identify individuals with impaired balance and at increased risk for falls. Some measures also identify specific impairments of body function and structure contributing to imbalance and can assess the impact of imbalance and falls on a person’s level of activity and ability to participate in usual activities. High-quality (precise, reliable, and valid) measures of imbalance and fall risk are essential for identifying who may benefit from interventions to improve balance and reduce fall risk, and for selecting the most appropriate interventions. In addition, balance and fall measures may overcome some of the limitations of tools currently used to assess the effectiveness of disease-modifying and symptomatic interventions, as discussed in detail later in this article.
Imbalance, or reduced postural control, is present and detectable in most PwMS. Imbalance can be the initial symptom of MS and has been found even in those with minimal changes on clinical examination. Balance impairment also generally persists and becomes more pronounced as MS progresses. Studies have found consistent differences in balance control between PwMS and healthy individuals. PwMS have 3 related balance control abnormalities. First, they have decreased ability to maintain position when attempting to stand still ; second, they have limited and slowed movement toward their limits of stability when attempting to lean or reach ; and third, they have delayed automatic postural responses when displaced or perturbed. In quiet stance, PwMS sway more than healthy controls and this postural sway increases even more than in controls with eyes closed and is greater in those with more impairment (higher Expanded Disability Status Scale [EDSS] scores) and in those with progressive MS. When initiating a step to start to walk, or when reaching, PwMS move less far and less quickly than healthy controls. Furthermore, PwMS have delayed automatic postural responses when the support surface they are standing on moves.
Imbalance affects quality of life and the performance of almost all daily activities. Imbalance not only affects walking but can also cause falls or near falls, both of which are common in PwMS, and falls can cause injury and fear of falling. Up to 63% of randomly selected samples of PwMS report having fallen at least once over the past 1 to 12 months, and many fall more often. Falls can occur early in the course of MS, although the risk seems to increase with increasing level of disability as long as the person is ambulatory (although falls may also occur during transfers in nonambulatory PwMS). Falls in PwMS are associated with injuries, most commonly fractures. In a Danish cohort of more than 11,000 PwMS, there were 22.8 fractures per 1000 person-years. Hip fractures were the most common followed by fractures of the radius/ulna, tibia, and femur. In middle-aged and older PwMS, an injurious fall is associated with increased fear of falling and activity curtailment. Whether or not a PwMS has fallen in the past 6 months, more than 70% report being concerned about falling. Fear of falling and the consequent inactivity can perpetuate a pattern of deconditioning, further balance impairment, and increased fall risk, as well as accelerated bone loss and an increased risk for fall-related fractures. Although near falls rarely result in injury and may prompt a PwMS to take steps to prevent future falls, near falls also likely increase fear of falling and reduce activity, self-esteem, and self-confidence. Poor postural control can also increase the energy demand of walking and other daily activities and thus increase fatigue and limit a person’s activity.
The high prevalence of imbalance and its significant consequences in PwMS makes imbalance important to recognize, quantify, and treat. Certain balance measures may also be able to guide intervention by determining the mechanisms contributing to imbalance. Various mechanisms have been proposed to underlie imbalance and falls in MS, including slowed somatosensory conduction, impaired central integration, weakness, and spasticity. In interviews, PwMS also report that impairments of attention, muscular endurance, gait pattern, vision, and proprioception, as well as heat sensitivity and fatigue, cause them to fall. Being able to identify, quantify, and understand the contributors to imbalance and increased fall risk in PwMS is essential for optimizing treatment. In this article, the roles and advantages of balance and fall measures in PwMS are discussed, specific balance and fall measures at different levels of the International Classification of Functioning, Disability and Health (ICF) model are identified, and the multidimensionality of falls is shown using the ICF model.
Assessment of Imbalance and Fall Risk Using the ICF Model
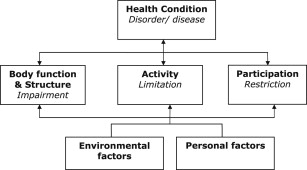
We recommend using the ICF model to structure the assessment of imbalance and fall risk in PwMS. The ICF model is also recommended for structuring the assessment of walking limitations in PwMS and for the assessment of imbalance, fall risk, and walking limitations in people with other central nervous system (CNS) disorders such as Parkinson disease or Alzheimer disease. This model was developed by the World Health Organization to provide a standardized language and structure for describing health and health-related conditions. According to the ICF model, health is the result of a complex interaction between functioning, disability, and contextual factors. Functioning and disability are made up of 3 components: body function and structure, activities, and participation. Contextual factors include environmental and personal factors ( Fig. 1 ). The ICF model facilitates clear and complete communication among health care providers concerning complex health problems. Imbalance, falls, and walking limitations in people with CNS disorders are complex health problems that can affect performance of a wide range of activities and participation in roles at home, at work, and in the community and that generally involve several professions to achieve optimal solutions. The ICF model can help identify possible causes, contributors, and ameliorators of imbalance, falls, and walking problems and may suggest solutions that can be provided by various health care team members to address 1 or more components of the model.
Roles and advantages of balance and fall measures in MS
Although balance and fall measures focus only on certain specific consequences of MS and do not provide information about the status or changes in processes underlying MS, including inflammation, demyelination, and neurodegeneration, these measures are suited to identifying PwMS with imbalance and at risk for falls and for directing interventions to address these problems. In addition, in PwMS, particularly those with progressive MS, these measures may represent useful adjunctive tools for assessing disease progression and the impact of other interventions, because they overcome some of the limitations of current measurement tools, including magnetic resonance imaging (MRI), relapse rate, EDSS, and MS Functional Composite (MSFC) scale.
MRI is an excellent tool for assisting in the diagnosis of MS and can be used to assess disease progression and activity. Most PwMS have characteristic lesions on brain MRI, and MS is almost uniquely associated with spinal cord lesions appreciable on MRI. During the relapsing phase of the disease, disease activity is reflected by an increase in the number, size, and overall volume of lesions on MRI and the presence of gadolinium-enhancing lesions. However, MRI is expensive and time-consuming, lesions generally evolve slowly over time, there is poor correlation between MRI lesion volume and location with physical abilities, and MRI is relatively insensitive to changes associated with progressive MS. The EDSS, a measure of neurologic function in 8 functional systems (visual, brainstem, pyramidal, cerebellar, sensory, bowel and bladder, cerebral, and other) in which a significant part of the scoring range is based on ambulation status, can be used to quantify MS progression and response to treatment and captures some aspects of body structure and function and some aspects of activity. However, it has poor intrarater and interrater reliability, does not assess other aspects of activity or any aspects of participation, and has limited precision, being a 20-point scale (0–10 including half-points). The MSFC, a 3-part multidimensional standardized composite clinical measure designed for use in clinical trials in MS, includes a simple timed measure of ambulation (the timed 7.62-m [25-ft] walk), a measure of upper extremity function (the 9-hole peg test), and a measure of cognitive function (the Paced Auditory Serial Addition Test [PASAT]). Although the MSFC may be more responsive to change than the EDSS, captures a range of activities, and correlates with MRI changes, it is limited by practice effects and floor and ceiling effects and does not assess participation or contextual factors.
In contrast to traditional MS measures, balance and fall measures can be inexpensive and quick, may detect change over a short period, are direct measures of physical abilities, and may also be more sensitive to gradual changes occurring in the absence of relapses, which can be particularly helpful in people with progressive MS. Balance and fall measures have also been found to correlate with EDSS scores and, although focused on lower extremity function, may provide more information than traditional measures do about activities and about the impact of activity limitations on participation; they can also predict who is at increased risk for falls.
Balance and fall measures at different levels of the ICF
A wide range of measures are available to assess balance and falls in PwMS. These measures include simple patient-completed questionnaires and a range of clinical tests and test batteries, as well as technologically advanced instrumented measures. Early in the course of MS, when imbalance can be subtle, patients may report imbalance despite current clinical measures not being sensitive enough to detect problems. In this circumstance, instrumented measures can be helpful because they often detect objective balance control deficits. Measure selection depends on the purpose of the measurement and the technical, personnel, and time resources available. The measures discussed in this article are those most often reported being used in published articles indexed in PubMed to February 2012 using the search strategy: “postural balance” OR “accidental falls” AND “multiple sclerosis,” and other measures that may provide substantial advantages over these commonly used measures.
Introduction
Multiple sclerosis (MS) is the most common nontraumatic neurologic disease of young adults. Worldwide, approximately 2.5 million people are diagnosed with MS. MS is characterized by variable neurologic symptoms, disease activity, and progression of functional limitations over time. Many people with MS (PwMS) report that ambulation is affected by their disease. PwMS walk more slowly than healthy controls and their balance is also impaired compared with healthy controls. PwMS also fall frequently. Even before walking is slowed, PwMS have balance impairments, which can be detected by clinical and instrumented measures. The focus of this article is the measurement and treatment of imbalance and fall risk in PwMS.
Balance measures can identify individuals with impaired balance and at increased risk for falls. Some measures also identify specific impairments of body function and structure contributing to imbalance and can assess the impact of imbalance and falls on a person’s level of activity and ability to participate in usual activities. High-quality (precise, reliable, and valid) measures of imbalance and fall risk are essential for identifying who may benefit from interventions to improve balance and reduce fall risk, and for selecting the most appropriate interventions. In addition, balance and fall measures may overcome some of the limitations of tools currently used to assess the effectiveness of disease-modifying and symptomatic interventions, as discussed in detail later in this article.
Imbalance, or reduced postural control, is present and detectable in most PwMS. Imbalance can be the initial symptom of MS and has been found even in those with minimal changes on clinical examination. Balance impairment also generally persists and becomes more pronounced as MS progresses. Studies have found consistent differences in balance control between PwMS and healthy individuals. PwMS have 3 related balance control abnormalities. First, they have decreased ability to maintain position when attempting to stand still ; second, they have limited and slowed movement toward their limits of stability when attempting to lean or reach ; and third, they have delayed automatic postural responses when displaced or perturbed. In quiet stance, PwMS sway more than healthy controls and this postural sway increases even more than in controls with eyes closed and is greater in those with more impairment (higher Expanded Disability Status Scale [EDSS] scores) and in those with progressive MS. When initiating a step to start to walk, or when reaching, PwMS move less far and less quickly than healthy controls. Furthermore, PwMS have delayed automatic postural responses when the support surface they are standing on moves.
Imbalance affects quality of life and the performance of almost all daily activities. Imbalance not only affects walking but can also cause falls or near falls, both of which are common in PwMS, and falls can cause injury and fear of falling. Up to 63% of randomly selected samples of PwMS report having fallen at least once over the past 1 to 12 months, and many fall more often. Falls can occur early in the course of MS, although the risk seems to increase with increasing level of disability as long as the person is ambulatory (although falls may also occur during transfers in nonambulatory PwMS). Falls in PwMS are associated with injuries, most commonly fractures. In a Danish cohort of more than 11,000 PwMS, there were 22.8 fractures per 1000 person-years. Hip fractures were the most common followed by fractures of the radius/ulna, tibia, and femur. In middle-aged and older PwMS, an injurious fall is associated with increased fear of falling and activity curtailment. Whether or not a PwMS has fallen in the past 6 months, more than 70% report being concerned about falling. Fear of falling and the consequent inactivity can perpetuate a pattern of deconditioning, further balance impairment, and increased fall risk, as well as accelerated bone loss and an increased risk for fall-related fractures. Although near falls rarely result in injury and may prompt a PwMS to take steps to prevent future falls, near falls also likely increase fear of falling and reduce activity, self-esteem, and self-confidence. Poor postural control can also increase the energy demand of walking and other daily activities and thus increase fatigue and limit a person’s activity.
The high prevalence of imbalance and its significant consequences in PwMS makes imbalance important to recognize, quantify, and treat. Certain balance measures may also be able to guide intervention by determining the mechanisms contributing to imbalance. Various mechanisms have been proposed to underlie imbalance and falls in MS, including slowed somatosensory conduction, impaired central integration, weakness, and spasticity. In interviews, PwMS also report that impairments of attention, muscular endurance, gait pattern, vision, and proprioception, as well as heat sensitivity and fatigue, cause them to fall. Being able to identify, quantify, and understand the contributors to imbalance and increased fall risk in PwMS is essential for optimizing treatment. In this article, the roles and advantages of balance and fall measures in PwMS are discussed, specific balance and fall measures at different levels of the International Classification of Functioning, Disability and Health (ICF) model are identified, and the multidimensionality of falls is shown using the ICF model.
Assessment of Imbalance and Fall Risk Using the ICF Model
We recommend using the ICF model to structure the assessment of imbalance and fall risk in PwMS. The ICF model is also recommended for structuring the assessment of walking limitations in PwMS and for the assessment of imbalance, fall risk, and walking limitations in people with other central nervous system (CNS) disorders such as Parkinson disease or Alzheimer disease. This model was developed by the World Health Organization to provide a standardized language and structure for describing health and health-related conditions. According to the ICF model, health is the result of a complex interaction between functioning, disability, and contextual factors. Functioning and disability are made up of 3 components: body function and structure, activities, and participation. Contextual factors include environmental and personal factors ( Fig. 1 ). The ICF model facilitates clear and complete communication among health care providers concerning complex health problems. Imbalance, falls, and walking limitations in people with CNS disorders are complex health problems that can affect performance of a wide range of activities and participation in roles at home, at work, and in the community and that generally involve several professions to achieve optimal solutions. The ICF model can help identify possible causes, contributors, and ameliorators of imbalance, falls, and walking problems and may suggest solutions that can be provided by various health care team members to address 1 or more components of the model.
Roles and advantages of balance and fall measures in MS
Although balance and fall measures focus only on certain specific consequences of MS and do not provide information about the status or changes in processes underlying MS, including inflammation, demyelination, and neurodegeneration, these measures are suited to identifying PwMS with imbalance and at risk for falls and for directing interventions to address these problems. In addition, in PwMS, particularly those with progressive MS, these measures may represent useful adjunctive tools for assessing disease progression and the impact of other interventions, because they overcome some of the limitations of current measurement tools, including magnetic resonance imaging (MRI), relapse rate, EDSS, and MS Functional Composite (MSFC) scale.
MRI is an excellent tool for assisting in the diagnosis of MS and can be used to assess disease progression and activity. Most PwMS have characteristic lesions on brain MRI, and MS is almost uniquely associated with spinal cord lesions appreciable on MRI. During the relapsing phase of the disease, disease activity is reflected by an increase in the number, size, and overall volume of lesions on MRI and the presence of gadolinium-enhancing lesions. However, MRI is expensive and time-consuming, lesions generally evolve slowly over time, there is poor correlation between MRI lesion volume and location with physical abilities, and MRI is relatively insensitive to changes associated with progressive MS. The EDSS, a measure of neurologic function in 8 functional systems (visual, brainstem, pyramidal, cerebellar, sensory, bowel and bladder, cerebral, and other) in which a significant part of the scoring range is based on ambulation status, can be used to quantify MS progression and response to treatment and captures some aspects of body structure and function and some aspects of activity. However, it has poor intrarater and interrater reliability, does not assess other aspects of activity or any aspects of participation, and has limited precision, being a 20-point scale (0–10 including half-points). The MSFC, a 3-part multidimensional standardized composite clinical measure designed for use in clinical trials in MS, includes a simple timed measure of ambulation (the timed 7.62-m [25-ft] walk), a measure of upper extremity function (the 9-hole peg test), and a measure of cognitive function (the Paced Auditory Serial Addition Test [PASAT]). Although the MSFC may be more responsive to change than the EDSS, captures a range of activities, and correlates with MRI changes, it is limited by practice effects and floor and ceiling effects and does not assess participation or contextual factors.
In contrast to traditional MS measures, balance and fall measures can be inexpensive and quick, may detect change over a short period, are direct measures of physical abilities, and may also be more sensitive to gradual changes occurring in the absence of relapses, which can be particularly helpful in people with progressive MS. Balance and fall measures have also been found to correlate with EDSS scores and, although focused on lower extremity function, may provide more information than traditional measures do about activities and about the impact of activity limitations on participation; they can also predict who is at increased risk for falls.
Balance and fall measures at different levels of the ICF
A wide range of measures are available to assess balance and falls in PwMS. These measures include simple patient-completed questionnaires and a range of clinical tests and test batteries, as well as technologically advanced instrumented measures. Early in the course of MS, when imbalance can be subtle, patients may report imbalance despite current clinical measures not being sensitive enough to detect problems. In this circumstance, instrumented measures can be helpful because they often detect objective balance control deficits. Measure selection depends on the purpose of the measurement and the technical, personnel, and time resources available. The measures discussed in this article are those most often reported being used in published articles indexed in PubMed to February 2012 using the search strategy: “postural balance” OR “accidental falls” AND “multiple sclerosis,” and other measures that may provide substantial advantages over these commonly used measures.
Body function and structure
Impairments in body function and structure, such as reduced muscle strength, altered muscle tone and coordination, altered gait pattern, reduced joint mobility, impaired sensation, impaired vision, fatigue, and impaired attention and cognitive function, are common in PwMS and may contribute to fall risk individually or in combination. Many measures are available to assess body function and structure, including posturography, MRI, the EDSS, and neurologic examination.
Muscle strength is required for body movement, and lower extremity muscle strength is required for standing and walking. Reduced lower extremity strength is associated with an increased risk of falling in women with MS. Strong abdominal and back muscles are also needed to stabilize the trunk when moving the extremities while walking. Weak proximal muscles can contribute to reduced lower extremity movement during the swing phase of gait and reduced stability during stance phase and can also impair knee stabilization during stance, leading to hyperextension. Weak ankle dorsiflexors, or increased ankle plantarflexor or hip adductor tone, may also cause tripping and stumbling. Upper extremity spasticity may also increase fall risk for people who use hand-held assistive devices for mobility. Muscle strength and tone can be tested using manual resistance of the tester, functional tests (eg, getting up from a chair), and with various devices (eg, spring or isokinetic dynamometers). Spasticity should be assessed both at rest and during functional activities because tone may change with position and activity. The modified Ashworth scale is commonly used to quantify spasticity at rest. Poor coordination, often as a result of cerebellar ataxia, may also contribute to an altered gait pattern, gait instability, and falls.
Altered gait pattern and reduced joint mobility may be the result of reduced strength, spasticity, ataxia, or sensory (including proprioceptive) loss. Gait pattern changes common in PwMS include reduced stride length, prolonged double limb support time, abnormal muscle recruitment, and gait initiation, as well as reduced maximum hip and knee extension and ankle plantar flexion range of motion. Gait pattern can be analyzed visually by observational gait analysis, or using an instrumented walkway. Instrumented walkways can measure various spatiotemporal parameters of gait and have shown that specific gait patterns are associated with EDSS functional scores. More sophisticated motion analysis systems, as provided in a gait laboratory or using gyroscopes and accelerometers worn by the patient, may provide additional useful information about gait kinetics and kinematics for research but are not available routinely in clinical practice.
Impaired touch and position sensation in the lower extremities is also associated with impaired postural control in PwMS and increases the risk for falls. Proprioception can be quickly assessed by estimating or matching the position of the great toe. Somatosensory-evoked potential testing can be used to more precisely quantify and localize somatosensory conduction abnormalities in the CNS. Although use of another reliable sensory input, usually vision, can compensate for impaired lower limb proprioceptive function to facilitate balance, in PwMS, visual dysfunction caused by optic neuritis (which can cause blurred vision and blind spots), and internuclear ophthalmoplegia or other oculomotor dysfunction (which can cause diplopia), often limit the use of visual substitution to improve balance. Visual impairment alone increases the risk for falls and further increases fall risk when combined with loss of proprioception. Visual acuity and oculomotor function are both evaluated as part of the EDSS and in the typical neurologic examination.
Fatigue can contribute to fall risk in PwMS by exacerbating other symptoms. In a systematic review of measurement properties of self-report fatigue questionnaires validated in individuals with a neurologic diagnosis, the Fatigue Scale for Motor and Cognitive (FSMC) functions and the Unidimensional Fatigue Impact Scale (U-FIS) were recommended for PwMS. The FSMC contains 10 cognitive and 10 motor dimensions rating fatigue in general using a 5-point Likert scale, giving a score range between 20 and 100. The U-FIS captures the impact of fatigue in the last week using 22 items covering one dimension rated by a 4-point Likert scale with a score ranging from 0 to 66. Other reliable fatigue scales developed for PwMS are the Modified Fatigue Impact Scale (MFIS) and the Fatigue Severity Scale (FSS). The MFIS is an MS-specific 21-item questionnaire evaluating the impact of fatigue on cognitive, physical, and psychosocial functioning. The MFIS is based on items derived from interviews with PwMS about how fatigue affects their lives. Scores on the MFIS range from 0 to 84, with lower scores indicating less fatigue. There is no published cutoff score for defining fatigue with the MFIS. The FSS is a 9-item questionnaire, which asks individuals to rate the degree to which fatigue affects their lives. Scores on the FSS range from 1 to 7, with lower scores indicating less fatigue. A cutoff score of greater than or equal to 5 on the FSS has been suggested to discriminate between fatigued and nonfatigued individuals. These fatigue measures are both validated and commonly used in drug and rehabilitation treatment trials in MS.
Impaired attention and cognitive function can also affect postural control, as shown by the worsening of postural control and gait impairment during dual task performance in PwMS. Gait slows and other spatiotemporal parameters of gait worsen more in PwMS than in healthy controls when a cognitive task is performed while walking. These changes are more pronounced in those with severe (EDSS 6.0–6.5) and moderate disability (EDSS 4.0–5.5) than in those with mild disability (EDSS 2.0–3.5). Postural control for other tasks also declines during dual task conditions in PwMS, with the greatest declines in those with higher EDSS scores. Attention and processing speed can be assessed by several tests, including the PASAT, which is a component of the MSFC. The Symbol Digit Modalities Test (SDMT, oral form) is another widely used test of attention and processing speed. Compared with the PASAT, the SDMT is less time-consuming, requires less equipment, and has good psychometric properties. The SDMT is recommended for use when personnel with neuropsychological training are lacking.
Computerized dynamic posturography (CDP) is the balance measurement tool most commonly used in published research. CDP uses a motorized platform and visual surround to assess static and dynamic balance directly. CDP equipment has the advantage of providing precise information about standing balance, postural sway and responses to perturbations of visual, proprioceptive, and vestibular input. However, use of CDP is limited by the expense of the equipment (∼$100,000 US) as well as the significant dedicated space requirements, specialized software products, and advanced training needs. These resource requirements have generally limited the use of CDP to research or specialty clinical settings. CDP has been used extensively to study postural control in MS as well as in many other populations and many control and comparison data are available. Recently, less expensive (∼$15,000 US) small wearable devices with gyroscopes and inertial sensors that precisely monitor movement to assess dynamic balance during walking have become commercially available. These newer devices also provide detailed information about postural control and have been shown to detect postural control deficits in PwMS whose walking is not slow. Use of these devices is limited by the lack of standard testing protocols and the absence of established reliability and validity in specific populations. Once standard testing protocols are developed and reliability and validity are established, it is likely that these wearable devices will contribute significantly to the study of postural control as well as walking in PwMS and people with other CNS disorders.
In addition to the specific measures of body function and structure discussed earlier, a clinical test battery, the Postural Physiologic Assessment (PPA), which involves simple tests of vision, peripheral sensation, muscle force, reaction time, and postural sway, has been developed to predict fall risk in elderly individuals. This battery has proven validity in older adults, and its validity in PwMS is currently being studied. For the PPA, postural sway in standing is assessed with the sway meter, a simple device with a pen attached to a horizontal bar extending from a belt worn around the pelvis ( Fig. 2 ). The PPA uses other portable inexpensive low-tech equipment for other components of testing, and a computer program is available to compare individual data with normative data.









