Massive Tears of the Posterosuperior Rotator Cuff
Laurence D. Higgins
Jon J. P. Warner
L. D. Higgins: Department of Orthopaedic Surgery, Duke University, Durham, North Carolina.
J. J. P. Warner: Department of Orthopaedic Surgery, Harvard Medical School, Boston, Massachusetts.
INTRODUCTION
Tears of the posterosuperior rotator cuff account for the majority of surgically treated massive rotator cuff tears. In Neer’s series81 of 340 rotator cuff tears operated over a 13-year period, 145 were classified as massive. Bigliani et al.10 operated on 61 massive rotator cuff tears in a 6-year period. During a 12-year period, Ellman31 performed 50 rotator cuff tear repairs (of which 9 [18%] were massive51), reviewed 105 cases (of which 28 had a tear involving the supraspinatus and infraspinatus, and an additional 22 involved the subscapularis52), reported that, of 100 consecutive cases during a 5-year period, 27 were massive rotator cuff tears,39 and reported a series of 50 massive rotator cuff tears operated during a 3-year period. Warner surgically treated 53 massive rotator cuff tears among 213 such injuries undergoing surgery during a 5-year period.120
Although the prevalence of these tears may seem low, their impact on patient function and pain is profound. The purpose of this chapter is to consider treatment approaches to massive rotator cuff tears involving the supraspinatus, infraspinatus, and teres minor (i.e., posterior rotator cuff tear). The anatomy, biomechanics, and natural history of these types of rotator cuff tears play a critical role in patient selection for reconstructive and salvage procedures. Special technical approaches, presented in the form of characteristic cases, highlight some of the problems with surgical repair and offer alternative solutions in cases of massive tears and revision situations.
Anatomically, most massive tears involve the posterior portion of the rotator cuff. Antero-superior rotator cuff tears involving the subscapularis with or without the supraspinatus are discussed in another chapter in this book. Although there is no universal agreement on the definition of massive rotator cuff tears, a consensus appears to be developing. In North America, the definition of Cofield27 is generally employed, with a massive tear being greater than 5 cm in its maximum diameter. In Europe, tears that encompass two or more of the rotator cuff tendons are considered massive.39,55,60 This definition is more functional than simply measuring the length of the tear. To accurately measure the extent of the rotator cuff tear, the degenerated rim of tissue is debrided. Because arm position may determine the appearance of the tear’s diameter, the length is measured in centimeters when the arm is at the side, and the tendons involved are recorded. Some advocate that the size of the tear not only reflects the anterior to posterior distance but represents the mediolateral retraction of the cuff (by creating an index that is the product of the anterior to posterior dimension multiplied by the medial to lateral retraction).108 This last gauge is unlikely to provide significant data because the tears are rarely rectangular, and the mediolateral distance is subject to arm position, especially rotation. Because there is
no consensus for measureing either pre- or postdebride-ment of the nonviable tendon stump, no standard exists; however, the authors believe that post-debridement measurements are superior and clinically more meaningful. Furthermore, if the humerus is pushed proximally, the dimensions of the mediolateral distance will increase (and similarly decrease with distal traction). Importantly, the dimension of the tear as a percentage of the size of the humeral head may be a more prognostic indicator because there is significant variation in patient size. Additionally, tissue quality is at least as important as tear size in determining the potential for a secure surgical repair. Acute massive tears may be much larger than 5 cm diameter but have robust, elastic tendon tissue that is easily repaired to its anatomical insertion, while chronic, smaller tears may have thin, friable, inelastic tendon tissue that mobilizes poorly and is repaired only tenuously.39,56
no consensus for measureing either pre- or postdebride-ment of the nonviable tendon stump, no standard exists; however, the authors believe that post-debridement measurements are superior and clinically more meaningful. Furthermore, if the humerus is pushed proximally, the dimensions of the mediolateral distance will increase (and similarly decrease with distal traction). Importantly, the dimension of the tear as a percentage of the size of the humeral head may be a more prognostic indicator because there is significant variation in patient size. Additionally, tissue quality is at least as important as tear size in determining the potential for a secure surgical repair. Acute massive tears may be much larger than 5 cm diameter but have robust, elastic tendon tissue that is easily repaired to its anatomical insertion, while chronic, smaller tears may have thin, friable, inelastic tendon tissue that mobilizes poorly and is repaired only tenuously.39,56
As in any surgical procedure, the surgeon must be selfcritical about patient selection, surgical treatment, and the ultimate functional outcome to measure the benefits of surgery. The standard outcome of these kinds of rotator cuff tears after surgery is good pain relief but some moderate to severe residual weakness and limitation of upper extremity endurance for work and sport activities. Keeping this in mind, it is possible to remain aware of the potential pitfalls in patient selection and treatment. Successful tendon healing is not always directly correlated with a good clinical outcome; however, powerful shoulder function usually requires an intact tendon repair. The use of arthroscopic repair for massive tears has been evolving and few studies14,18, 19, 20 and 21,67,72 document the success of this approach. Galatz et al.36 reported on the outcome and repair integrity of large and massive rotator cuff tears. Ultrasound documented recurrent tears in 17 of 18 patients at a minimum of 1 year postoperatively, and functional results deteriorated over a 2-year period. Gerber et al.39 documented repair integrity of 75% 2 years after massive rotator cuff tear repaired with open technique. Thus, it seems that structural integrity after arthroscopic repair is not as assured as with open repair. However, newer techniques of arthroscopic repair promise to bring this method on par with open from the standpoint of tendon healing. Regardless of the operative technique, the patient can anticipate improved function and reduced pain if the preoperative, surgical, and postoperative rehabilitation plans are well formulated and executed.
PREOPERATIVE CONSIDERATIONS
Treatment plans must be formulated on an individualized basis, accounting for functional needs, disability, and patient goals. It is critical that the physician consider whether pain or functional difficulties are the major problem. Coexistent medical conditions may argue against aggressive reconstructive surgery because of the higher risks of morbidity or mortality. For example, an elderly, frail, female patient with cardiac problems or diabetes mellitus can be treated with a less aggressive surgical approach than an otherwise healthy 50-year-old man, even though they have similar rotator cuff injuries (i.e., similar-sized tears). These patients have different functional needs and goals. The former may have a problem with pain and need functional recovery for activities of daily living only, while the latter may require strength for forceful overhead activities or sports. Surgeons must consider their experience and ability to address these tears with an arthroscopic or open technique and whether salvage procedures are indicated.
PATHOANATOMY AND PATHOMECHANICS
The force potential of each of the four rotator cuff muscles has been determined based on the individual physiological cross-sectional areas.61,66,69,110,113 Each muscle’s leverage can be determined based on a perpendicular drawn from its line of action to the center of rotation of the humeral head.6 If each muscle’s force potential is multiplied by the muscle’s leverage, its functional contribution can be determined. Tables 7-1 and 7-2 show the supraspinatus’s relatively small physiological cross-sectional area and rotational potential compared with the other rotator cuff muscles. This is because of its smaller size and closer insertion to the axis of rotation of the joint. Keating et al.61 demonstrated that the supraspinatus makes a small (14%) contribution to the overall abduction moment arm. In comparison, the infraspinatus and teres minor, together, contribute 32% and the subscapularis contributes 52%. This illustrates the primary importance of the anterior and posterior components in shoulder joint rotation.
Arm position is critical in determining the role of each muscle. The moment arm of the supraspinatus is largest in the first 30 degrees of abduction. Its mechanical advantage is reduced as the shoulder is abducted above this level.
During simple scapular plane abduction, the tendon excursions of the rotator cuff muscles are minimal compared with the deltoid muscle (Table 7-3).69 They function more as stabilizers than as prime movers, providing a fixed fulcrum for concentric rotation of the humeral head on the glenoid.58,92 During early abduction, the deltoid creates a relative upward shearing moment that must be resisted by a force couple with the combined rotator cuff muscles. Disruption of the rotator cuff weakens the stabilizing effect that resists this superior translation.9,65,83,125,126 In vitro59,64 and in vivo122 studies have shown that the long head of the biceps brachii resists anterior and superior translation of the humeral head on the glenoid, and is often enlarged or “hypertrophied” in patients with large rotator cuff tears.81,83
During simple scapular plane abduction, the tendon excursions of the rotator cuff muscles are minimal compared with the deltoid muscle (Table 7-3).69 They function more as stabilizers than as prime movers, providing a fixed fulcrum for concentric rotation of the humeral head on the glenoid.58,92 During early abduction, the deltoid creates a relative upward shearing moment that must be resisted by a force couple with the combined rotator cuff muscles. Disruption of the rotator cuff weakens the stabilizing effect that resists this superior translation.9,65,83,125,126 In vitro59,64 and in vivo122 studies have shown that the long head of the biceps brachii resists anterior and superior translation of the humeral head on the glenoid, and is often enlarged or “hypertrophied” in patients with large rotator cuff tears.81,83
TABLE 7-1 PHYSIOLOGIC CROSS-SECTIONAL AREAS DETERMINED FOR ROTATOR CUFF TEAR MUSCLES | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 7-2 ROTATIONAL POTENTIAL OF THE ROTATOR CUFF | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
TABLE 7-3 TENDON EXCURSIONS OF THE ROTATOR CUFF AND DELTOID DURING SCAPULAR PLANE ABDUCTION | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Clinical18, 19, 20 and 21,97,99 and experimental110 observations have shown that even large tears of the rotator cuff can remain well compensated with the appearance of good motion and concentric rotation of the glenohumeral joint (Fig. 7-1). Extension of the tear into the infraspinatus and teres minor or into the subscapularis usually results in complete loss of containment and superior translation of the humeral head.19, 20 and 21,38,44,110,118,123 Nevertheless, some patients with symptomatic small tears have very poor function, while others with larger tears retain reasonable function (see Fig. 7-1). Tears that extend inferior to the equator
result in biomechanical decompensation, with loss of the stabilizing effect of the rotator cuff and, therefore, the fixed fulcrum for rotation of the humeral head on the glenoid.19,38,44,110 In advanced grades, fatty atrophy plays a significant role and appears to herald the irreparability of the involved tendons and will be discussed later. It should be stressed that atrophy may occur, particularly in the infraspinatus, when the tendon is still intact.76,80,103,113,129 These findings, and others yet to be elucidated, may help explain the disparity of experience in surgical treatment of massive rotator cuff tears that is found in the literature.4,7,10,15,18, 19, 20 and 21,24, 25 and 26,28,29,31,38,39,42,44,45, 46 and 47,49,50,68,84, 85, 86 and 87,91, 97,100,106,119,129
result in biomechanical decompensation, with loss of the stabilizing effect of the rotator cuff and, therefore, the fixed fulcrum for rotation of the humeral head on the glenoid.19,38,44,110 In advanced grades, fatty atrophy plays a significant role and appears to herald the irreparability of the involved tendons and will be discussed later. It should be stressed that atrophy may occur, particularly in the infraspinatus, when the tendon is still intact.76,80,103,113,129 These findings, and others yet to be elucidated, may help explain the disparity of experience in surgical treatment of massive rotator cuff tears that is found in the literature.4,7,10,15,18, 19, 20 and 21,24, 25 and 26,28,29,31,38,39,42,44,45, 46 and 47,49,50,68,84, 85, 86 and 87,91, 97,100,106,119,129
Role of Muscle Atrophy and Fatty Degeneration
The term massive rotator cuff tear describes a heterogeneous population of patients with varying degrees of shoulder dysfunction. Goutallier46 was the first to point out that overall shoulder function and external rotation weakness correlated with the degree of fatty degeneration and muscle atrophy of the infraspinatus muscle, and that such changes were usually chronic and irreversible after surgery47 Goutallier also recently validated a global fatty degeneration index (GFDI) that predicts the likelihood for recurrent tear after surgery. By using a grading scale from 0 to 4 (in order of severity), the subscapularis, supraspinatus, and infraspinatus are each assigned a score. The mean value for these three muscles determines the GFDI. A GFDI of less than 0.5 was necessary for a retear rate less than 25%, and a GFDI greater than 2 had a 100% retear rate. Of the 220 patients who underwent rotator cuff repair, the highest percentage of recurrent tears were noted in the posterosuperior tears (56% vs. a mean of 36% for all other tears). Although Goutallier has used computed tomography (CT) to assess and grade atrophy, the use of magnetic resonance imaging (MRI) has been similarly investigated.
Warner124 studied patients with massive rotator cuff tears of similar size and found a correlation between the magnetic resonance imaging (MRI) appearance of atrophy and fatty degeneration and the overall shoulder function and biomechanics (Fig. 7-2). Fuchs et al.35 compared MRI to CT to assess the validity of MRI as the imaging tool to assign a grade of fatty degeneration according to Goutallier.46 While interobserver and intraobserver reliability was good for each imaging modality, the correlation between CT and MRI was only fair to moderate. Nevertheless, MRI has replaced CT as the most common imaging modality to assess the rotator cuff.35,113,120,123
The amount of muscle atrophy and the acromiohumeral interval are critical preoperative considerations in determining the course of treatment for these patients. If the acromiohumeral interval on a true anteroposterior radiograph with the arm in neutral rotation is less than 5 mm, and if there is marked muscle atrophy and fatty degeneration on MRI,88 then surgical repair of the rotator cuff cannot recenter the humeral head in the glenoid, and restoration of strength and function is unlikely. Patients need to be counseled regarding this enhanced risk of tendon retear, if repair is pursued. Furthermore, wanton disregard for this basic tenet of rotator cuff repair and an ill-advised attempt at repair with disruption of the coracoacromial ligament can lead to a disastrous clinical outcome including significant degradation of patients’ function and worsening pain. In fact, the occurrence of fixed anterosuperior escape of the humeral head is a difficult and vexing clinical problem, without adequate orthopedic solution.
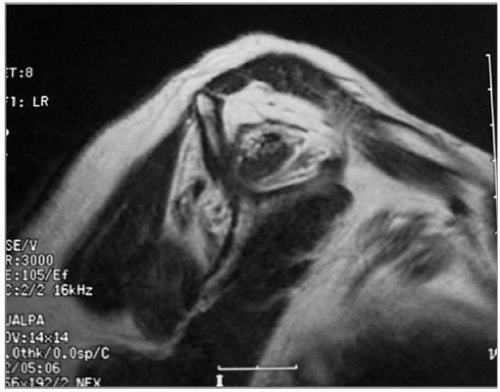 Figure 7-2 Oblique sagittal plane on MRI demonstrates severe fatty degeneration of supraspinatus and infraspinatus muscles. |
Surgical relevance of fatty muscle changes have also recently been clarified. Meyer et al.40,42,74 demonstrated that muscle compliance decreased (the tendon became stiffer and less mobile) in chronic tendon tears, and this precluded direct repair to bone in many cases.54,75 Warner (unpublished data, 2000) found a correlation between the degree of muscle fatty change on preoperative MRI, and the tendon quality observed intraoperatively. In general, if the fatty muscle change were Goutallier stage 3 or 4, the tendon would be friable and stiff. This was usually associated with inability to repair the tendon to bone.
More recently, Meyer and Gerber74 described the etiology of fatty muscle atrophy. They observed that when the tendon tears, the pennation angle between the individual muscle fibers decreases, and there is an increased space between muscle fibers that fills with fat. The muscle then becomes retracted and stiff. This was observed to be irreversible after late tendon repair in sheep.
Role of the Coracoacromial Ligament
The coracoacromial ligament has been shown clinically4,111 and experimentally33 to have an important secondary stabilizing role preventing anterosuperior translation when the rotator cuff containment function is lost. In these situations, it acts as a last barrier to unchecked anterosuperior translation of the humeral head, and it must be preserved.4,15 The type III (hooked) acromion shape is probably a compensatory phenomenon that attempts to reduce superior humeral head displacement in cases of massive rotator cuff tears. Routine acromioplasty may be biomechanically inadvisable in cases of chronic, long-standing massive rotator cuff tears because it may destabilize the coracoacromial ligament with resultant anterosuperior escape4,102 (Fig. 7-3).
Role of the Long Head of the Biceps
Whether the biceps serves as an important stabilizer of the shoulder in rotator-cuff-deficient shoulders is a matter of continued debate. It is becoming increasingly clear that the biceps does not have an active role in the setting of massive rotator cuff tears, and there may be a passive tenodesis effect as supported by others.59,64,116,117,128,130 If there is significant biceps disease, most authors advocate tenodesis or tenotomy because this may be a significant pain generator in the setting of cuff disease. Indeed, Walch et al.116 has provided strong evidence that simple biceps tendon tenotomy may significantly improve pain in patients with irreparable massive rotator cuff tears.
DIAGNOSTIC CONSIDERATIONS
History
Most posterior rotator cuff tears occur in individuals in their 6th through 8th decades of life, and they occur as a result of multiple biological and mechanical factors. The exact cause of full-thickness rotator cuff tear remains a subject of debate; however, the following explanations form the basis of current treatment recommendations. Gradual attrition of the supraspinatus tendon insertion from “outlet impingement” against the anterosuperior acromion and an arthritic clavicle is enhanced by a paucity of blood supply in this region.81,82,95,98 Intrinsic degeneration in the rotator cuff probably also reduces its structural strength, putting it at greater risk for failure even with trivial trauma.96
Some predictions can be made about the size of the tear and quality of tendon tissue based on the history given by the patient. If a patient reports no specific traumatic event and the loss of function and onset of pain as insidious and chronic, then the quality of the tendon tissue is likely poor, and these individuals may also have significant atrophy and fatty degeneration of the spinate musculature.46,47 Patients who have had multiple steroid injections often have thin, friable tendon tissue, and those with a history of chronic tobacco use also tend to have larger tears and poorer tendon tissue for repair. A chronic, massive rotator cuff tear may also result in disuse osteopenia of the proximal humerus. This can make secure tendon-bone repair more difficult. In some individuals with a long-standing massive rotator cuff tear, there is tendon involution or loss, and the remaining muscle and tendon are inelastic because of scarring and fatty degeneration (Fig. 7-4).38,44 Surgical
mobilization of the tendons for repair can be very difficult in these cases.7,31
mobilization of the tendons for repair can be very difficult in these cases.7,31
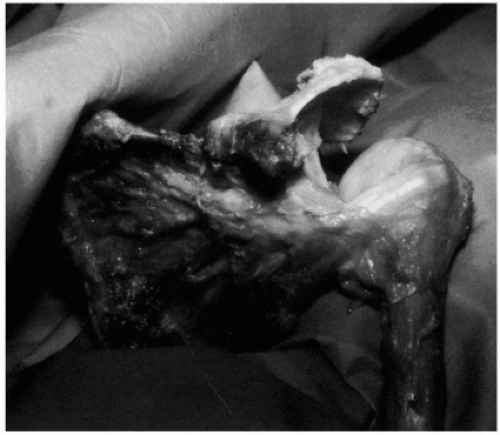 Figure 7-4 A cadaver shoulder from a 78-year-old man demonstrates a chronic massive rotator cuff tear with loss of tendon tissue and atrophy of muscle. |
When the patient is in his or her fifth or sixth decade and reports a specific traumatic event preceding the onset of shoulder pain and poor function, it is more likely that the quality of the torn tendon and muscle is good, with elastic, easily mobilized tissue. Hersche and Gerber54 have demonstrated that the duration of the rotator cuff tear is associated with increased stiffness and passive tension of the muscle-tendon unit.
Clinical Appearance
Not all of these patients have a painful arc and positive impingement signs.82 Massive rotator cuff tears involving the supraspinatus, infraspinatus, and teres minor may often present as a painless pseudoparalysis.
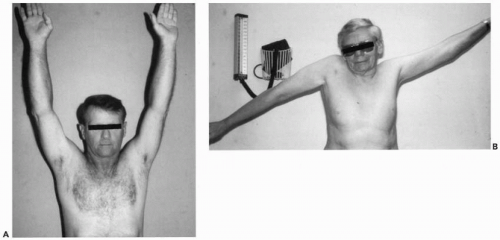
Several physical findings are specific for massive rotator cuff tears involving the posterosuperior tendons. First, in those with a painful and weak shoulder, strength testing may greatly overestimate the true limitations of that individual, because pain inhibition prevents a good effort by the patient.8 We perform an impingement test by injecting 10 to 15 mL of 1% Xylocaine into the subacromial space 10 minutes before examining a patient’s strength and active motion.81,82 Active motion should be assessed with specific attention to scapulothoracic and trunk substitution patterns in individuals with poor glenohumeral motion due to a massive rotator cuff tears (Fig. 7-5). It is imperative to assess any differences between passive and active motion arcs, because this gives valuable information about which portions of the rotator cuff are involved. A patient who has a significant lag of active external rotation when the arm is positioned in abduction has a massive tear extending into the infraspinatus and teres minor tendons. The hornblower’s sign (signe du clairon) is pathognomonic for a massive rotator cuff tears involving the infraspinatus and teres minor tendons (Fig. 7-6).38,44,115 The patient is asked to abduct his shoulders while keeping his hands at mouth level. He then externally rotates his shoulders to put his hands on top of his head. The normal side allows this combined abduction and external rotation, and the side with a massive rotator cuff tear is not able to externally rotate with the shoulder in abduction, giving the appearance that the patient is blowing a horn. Alternatively, the patient’s hand can be placed in the position of abduction and external rotation and then released (Fig. 7-6). Failure to maintain the arm in this position against gravity confirms the presence of a non-functioning posterosuperior rotator cuff. This test can be repeated for external rotation with the arm at the side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree