Managing Simple Wound Problems
Steven Moran
Nho V. (Bill) Tran
Bernard F. Morrey
INDICATIONS
The thin and pliable soft tissue envelope covering the elbow is prone to trauma. Most elbow soft tissue defects can be closed primarily due to the laxity of the skin surrounding the joint; however, the mechanism of the trauma will dictate the optimal management of any soft tissue injury. As a general rule, wounds should be clean and fractures and ligamentous injuries should be stabilized prior to soft tissue closure. Clean surgically created wounds can be closed immediately in layers with excellent success (1). In a trauma patient, a simple laceration in a clean setting can also be irrigated and closed primarily. In contrast, a patient involved in a high-speed motor vehicle accident can have a simple laceration with underlying soft tissue devascularization or extensive tissue ischemia. These cases can be further complicated by embedded debris and extensive contamination. Such wounds may require multiple surgical débridements until they are fit for closure. Concomitant life-threatening injuries in trauma cases can delay elbow management until the patient is stabilized. This chapter reviews the basic principles of soft tissue management to help one obtain primary wound healing.
CONTRAINDICATIONS TO PRIMARY CLOSURE
For elective procedures and routine trauma, contraindications to primary closure are excessive tension on the wound edges, extensive tissue loss preventing primary closure, and gross contamination or infection. The contaminated or infected wound will require serial debridement until a clean (bacterial count less than 105 organisms) wound is obtained. Blanching at the wound edges and skin tearing during wound closure are both signs of extensive tension. Newer imaging modalities, including laser-assisted indocyanine green angiography can be used to assess the blood flow to the incision once the incision is closed (2). If the wound appears ischemic or if tension is too great, the wound can be covered with an occlusive dressing, vacuum-assisted wound closure (VAC), or wet sterile dressing, and the wound can be reassessed in the operating room in 24 to 48 hours (3). Over the course of 24 to 72 hours, swelling will often subside, allowing for primary wound closure.
Wound Vacuum-Assisted Wound Closure
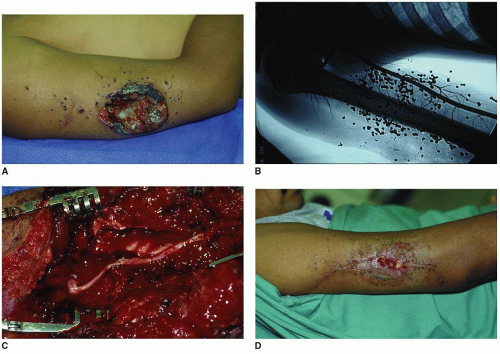
Negative pressure therapy (VAC) is known to decrease wound edema and bacterial load and improve tissue perfusion. Its use may allow delayed primary closure in simple cases and can effectively prepare the wound for complex reconstruction (Fig. 13-1). The elbow can be extended and splinted in an extended position to take tension off the wound edges during the first 10 to 14 days of wound healing.
General contraindications to immediate wound closure would include life-threatening injuries, compartment syndrome, and vascular injuries with associated limb ischemia (Fig. 13-2). Skeletal stability should ideally be obtained prior to soft tissue closure.
PREOPERATIVE PREPARATION
Once the patient is hemodynamically stable, a complete history and physical exam of the extremity is obtained. The patient’s tetanus vaccination history is obtained. Patients with prior vaccinations are revaccinated with Tdap, tetanus and pertussis combined vaccine (2,3 and 4). For those without a history of tetanus vaccination, human tetanus immunoglobulin should be given. Appropriate radiographs are obtained and reviewed, and the neurovascular examination of the limb is performed to verify there are no nerve injuries. A detailed upper limb examination may be too painful for the patient to tolerate in the emergency room. Nevertheless, simple inspection of the skin color, capillary refill, the finger cascade, as well as testing of gross finger sensation can usually help one determine if major structures are injured. When the patient is medically cleared, he or she may be taken to the operating room for a formal debridement of the elbow. Wound probing and formal examination should be reserved for an OR setting where local hemostasis can be achieved and the surgeon can clearly assess all injured structures.
For low-energy urban trauma, preoperative antibiotics may be given to cover routine skin flora. For farm wounds, wide spectrum coverage is necessary until appropriate intraoperative culture result becomes available. Subsequent wound cultures can be used to target later therapy to specific pathogens. Patzakis et al. (5,6) have shown that patients receiving antibiotics within 3 hours of injury had a lower rate of infection than did those who did not, and treatment should ideally be initiated immediately. Routine organisms are by far the most frequent cause of severe infections in the upper limb with Staphylococcus aureus being the most common infecting organism. Streptococci and Pseudomonas are also commonly cultured. The recommended duration for antibiotic use in grade III open fractures is 5 days (7).
Injuries sustained in an agricultural setting or in industrial machinery are subject to heavier and deeper contamination. Mechanical roller injuries involving crush, avulsion, or degloving will result




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree