Management of Traumatic Wounds: Complex Soft Tissue Reconstruction
Christopher A. Park
Joseph A. Molnar
Open wounds are often the most obvious physical finding on the trauma patient. Regardless of how dramatic the wound, the treating physician must realize that this may not be the most life-threatening injury. To avoid the pitfall of being distracted by the most obvious, but perhaps not the most urgent injury, maintaining adherence to the fundamental principles taught in the other chapters of this book are essential.
Initially, the patient must undergo an initial assessment following the Advanced Trauma Life Support (ATLS) principles of primary survey with control of airway, breathing, and circulation; complete secondary survey, and radiographic examinations.1 In the course of this overall evaluation, all wounds will be identified in a systematic and thorough manner. During this process, prioritization must be determined and constantly reassessed. At this stage, the major role of traumatic wounds is to serve as a locator of sites of major impact. They are usually of lower importance, except for wounds associated with potential exsanguination or life-threatening injuries.
INITIAL MANAGEMENT
In the initial survey, the primary goals of wound management include control of hemorrhage, preventing further injury, and limiting contamination. Pressure should be held to bleeding wounds. It is rare that direct pressure will not control bleeding. Tourniquets are not recommended unless bleeding is life threatening and unable to be controlled with direct pressure. One should avoid using clamps in wounds in a nonsurgical setting because one may inadvertently damage nerves or other structures near a bleeding vessel. Bleeding from fractures is best managed by stabilizing the fracture with reduction and splinting or traction. This is true even of open Le Fort facial fractures where bleeding may be controlled with disimpaction, closed reduction, and wrapping with a pressure dressing such as an ace wrap.
To avoid further contamination, a sterile, moist dressing should be applied to all open wounds as soon as other priorities are addressed. In a similar manner, amputated parts should be kept clean and preserved in moist, sterile saline-soaked gauze, placed in an impermeable barrier such as a plastic bag or specimen cup, and submerged in iced water.
As part of the initial survey, one must limit further injury of tissues. For example, compartment syndrome requires immediate operative release with fasciotomies of the involved compartments. Injured limbs should be elevated as feasible to prevent progressive edema and loss of circulation. Fracture reduction will frequently assist
to improve vascular inflow to an injured extremity by eliminating vascular stretch or pinching of the vessels.
to improve vascular inflow to an injured extremity by eliminating vascular stretch or pinching of the vessels.
After the control of hemorrhage and treatment of life-threatening injuries, management of traumatic wounds rises in priority. It must be determined whether the wound can be managed in the primary setting (emergency room, field, clinic, etc) or if the wound requires surgical management. Key factors include amount of contamination, extent of devitalized tissue, proximity to important structures, and comfort of the patient.
Tetanus
Patients with wounds at risk for tetanus who have not had a booster within 5 years, are not sure of immunizations, or cannot provide a history of immunization status, require a tetanus booster. Non-tetanus-prone wounds reduce the cutoff to 10 years since last booster. If a patient with a high-risk wound has never been immunized or has not completed the three-dose tetanus immunization, tetanus immune globulin should be administered.
Antibiotics
The administration of systemic antibiotics in acute trauma patients is controversial. With the rapid proliferation of antibiotic-resistant organisms, prophylactic antibiotics are not indicated except for selected cases, including open fractures, open joints, exposed cartilage, heavy contamination, bite wounds, delayed wound management, and patients with impaired wound healing (immunosuppressed, diabetic, and severe atherosclerosis). Topical antibiotics, including antibiotic ointments, silver impregnated dressings, or saline dressings, are more often appropriate.
Wound Preparation
In wounds amenable to management in the priority setting, the principles are wound preparation, local anesthesia, decontamination, and closure. The area surrounding the wound should be prepared with topical bactericidals such as iodine or chlorhexidine products. These products are cellular toxins in the concentrations used to prepare the skin surrounding the wound and as such are detrimental to wound healing.2 They are not recommended for open wound application. Shaving the surrounding area is not necessary and has actually been shown to increase wound infections in some cases.3 4
TABLE 1 LOCAL ANESTHETICS | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||
Anesthesia
Before wound manipulation, adequate anesthesia must be obtained. This can be accomplished in smaller wounds with local injection or nerve blocks because topical anesthetics are of limited benefit in traumatic wounds. Dosages, durations, and adverse reactions of local anesthetics vary depending on the anesthetic and the physician must be aware of these (see Table 1). Local anesthetic central nervous system (CNS) toxicity begins with tinnitus, tremors, metallic taste in the mouth, numbness, and can progress to seizures. Cardiovascular toxicity is the result of myocardial depression, leading to hypotension, altered heart rate, and ultimately arrhythmias.
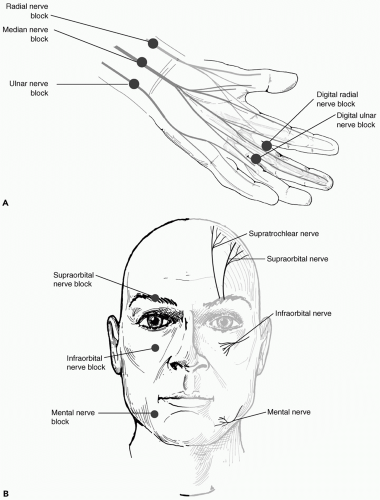
Larger areas can be anesthetized with minimal anesthetic with knowledge of the anatomy of sensory nerves. The most common regional blocks performed include digital blocks (radial and ulnar digital nerves), wrist blocks (median nerve, ulnar nerve, and radial sensory nerve), and facial blocks (supraorbital, infraorbital, or mental nerve) (see Fig. 1). Ears, nose, and genitalia are frequently anesthetized with field blocks of anesthetic without epinephrine to avoid vascular compromise.
Finally, the largest wounds will require general anesthetics and must be explored in the operative suite to allow adequate exposure, to control hemorrhage, and to have access to needed operative tools to do the procedure in an optimal manner. Indeed, the test of whether one must
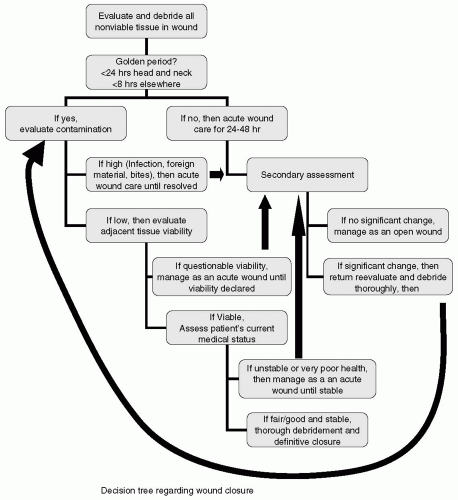
treat the wound in the operative suite must be judged by whether the operative surgeon can do the procedure just as well in the setting of the emergency department (see Fig. 2).
treat the wound in the operative suite must be judged by whether the operative surgeon can do the procedure just as well in the setting of the emergency department (see Fig. 2).
Debridement
After obtaining adequate anesthesia, the open wound requires exploration for additional injuries, removal of contamination and foreign bodies, irrigation, and debridement of nonviable or heavily contaminated tissue. As stated, topical antiseptics impair wound healing unless used in a very dilute solution. Surgical debridement and copious irrigation are necessary and sufficient to decontaminate the open wound. The decision regarding how much to debride requires multifactorial analysis. Obviously, nonviable tissue should be debrided as it impairs
healing and increases the risk of infection. Marginal tissue may best be managed by preservation with plans for repeat debridement and delayed closure unless it is of minimal functional benefit. Once the wound has been irrigated and debrided, the physician must determine whether the wound is amenable to closure based on size, available tissue, and level of contamination.
healing and increases the risk of infection. Marginal tissue may best be managed by preservation with plans for repeat debridement and delayed closure unless it is of minimal functional benefit. Once the wound has been irrigated and debrided, the physician must determine whether the wound is amenable to closure based on size, available tissue, and level of contamination.
Decision Regarding Closure
The decision to dose a wound or to manage it as an open wound requires a determination of the likelihood of success of primary closure. The risk of failure of primary closure can lead to more damage and a worse outcome than open wound care with delayed healing. An important factor to consider in this decision is the length of time since injury. Six to eight hours is considered the “golden period” during which primary closure is possible. After this period of time, bacterial counts are significantly higher. Longer periods of time (typically 24 hours) are acceptable for injuries above the neck as these wounds are cosmetically more apparent and relatively resistant to infection due to better blood supply.
The degree of contamination either based on mechanism, history, or examination is another important variable to weigh. Relative contraindications to primary closure include human bites, nonhuman bites (except for the face), and embedded foreign material.
Systemic factors must also be considered in the decision for wound closure. Associated conditions to consider
include patient age, diabetes, immune function, vascular status, immunization history, coagulation status, and associated injuries. For example, a patient with intra-abdominal hemorrhage may be too unstable to undergo wound closure on the face until fluid resuscitation is complete.
include patient age, diabetes, immune function, vascular status, immunization history, coagulation status, and associated injuries. For example, a patient with intra-abdominal hemorrhage may be too unstable to undergo wound closure on the face until fluid resuscitation is complete.
Questions of the viability of adjacent tissues should preclude primary closure. This is an important variable in thermal burns, electrical injury, crush injury, and “missile” injury. In each of these situations there is frequently found a zone of nonviable tissue and an area of tissue of questionable viability. This is similar to the zones established in burns, which Jackson referred to as the zone of coagulation, the zone of stasis, and the zone of hyperemia.5 The zone of coagulation in burns is quite similar to the zone of necrotic tissue found in a crush or avulsion type injury. This tissue is dead at the time of first observation and must be removed from the wound to avoid progressive sepsis or myoglobinuria. Adjacent to this is an area of edema and tissue of questionable viability, which is the zone of stasis. In this tissue, the blood flow is sluggish and depending upon the events of the next few days may go on to survive or die. As a result, in many complicated injuries such as open tibial fractures, serial debridements are necessary before closure. In some cases, this may take several surgeries over a period of 2 weeks or more. It is the authors’ experience that in these situations, the temptation is to dose the wound sooner than is biologically safe leading to infection, dehiscence, and increased morbidity and hospital stay. As a result, the “rule-of-thumb” is to debride the wound “N + 1” times. That is, it is recommended that in order to minimize the risk of failure of closure that the wound be debrided one more time after the wound appears that it “might” be able be closed safely.
The “N+1” rule
An additional surgical debridement is usually beneficial before closure and rarely harmful
THE RECONSTRUCTIVE LADDER
Numerous decisions are made in the management of traumatic wounds. A plethora of options exist for dealing with a particular wound. Each option has its own advantages and disadvantages, requirements and costs, side effects, and complications. Expert management requires a large amount of experience as many options and priorities must be weighed. The principles can be practiced by anyone. In general, the goal is to obtain a clean, closed wound with the lowest physical, emotional, and temporal cost to the patient. It is essential to bear in mind that no method has complete success. It is important to consider and protect options that can be implemented if initial attempts are unsuccessful. The advantage of obtaining early closure is not only of obvious financial and psychological benefit but also shortens the wound healing process.
The three phases of wound healing are inflammatory, proliferative, and remodeling. The inflammatory phase occurs in the first several days after injury and the major events are hemostasis and recruitment of inflammatory cells. The proliferative phase proceeds until wounds are closed and consists of granulation, contraction, and epithelialization. The remodeling phase can last years and the major event is collagen maturation. The inflammatory and proliferative phases of wound healing are minimized when early closure of clean wounds is obtained. This improves overall medical status because these phases utilize significant metabolic energy and cause considerable pain and disability. Traditional thinking taught that wound reconstruction should occur early before significant inflammation. Subatmospheric pressure has been shown to limit inflammatory mediators and has adjusted this timeline, allowing serial debridements to prepare wounds before definitive reconstruction.6
Principles of Traumatic Wound Reconstruction
Reduce contamination
Expedite phases of wound healing
Minimize morbidity
Minimize complications
Maximize long-term function
Preserve future options
Methods of Wound Closure
Increasing Complexity
Wound Closure Techniques
Primary intention (primary closure)
Secondary intention
Tertiary intention (delayed primary closure) Reconstruction
Autograft
Local flaps
Free tissue transfer
Primary Intention
In healing by primary intention (primary closure), the wound can be reapproximated in one or multiple layers. Deeper wounds require closure of structures of strength. Fascial layers that have been violated should be dosed in order to reduce tension on the skin. If necessary, the skin edges can be undermined or fascias can be incised and released remotely from the wound to allow closure of the wound.
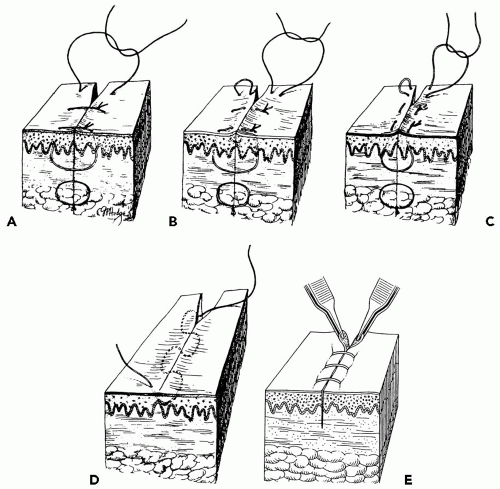
The cutaneous edges can be closed in many ways. The strongest closure is closure of the deep dermis with
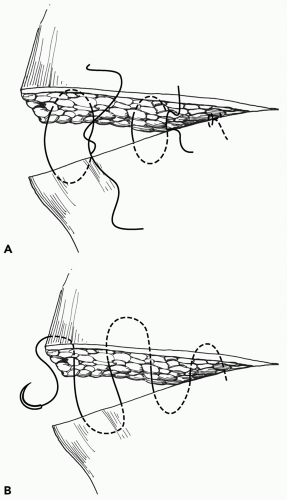
an absorbable suture (i.e., polyglycolic acid) followed by closure of the epidermis with subcuticular or intercuticular suture. This is called a layered closure. The least amount of observable scar is created with a running, nonabsorbable, subcuticular suture with the least inflammatory response (i.e., polypropylene). However, this suture does require removal (see Table 2). An absorbable subcuticular suture (i.e., poliglecaprone 25) can be used but has a prolonged inflammatory phase during suture degradation. Small, clean, simple lacerations with minimal retraction can be managed with noninvasive techniques, including suture strips and cutaneous adhesive (i.e., Dermabond, Ethicon: Cornelia, GA). If external sutures are used in an interrupted, mattress, or running fashion, they should be removed as early as possible to minimize scarring from the suture. Staples can also be used and are preferred in the scalp to expedite closure and reduce pain of application and removal without compromising cosmesis.7 Vertical mattress sutures are used for extra strength and eversion of wound edges. Horizontal mattress sutures provide additional hemostasis (see Figs. 3 and 4).
an absorbable suture (i.e., polyglycolic acid) followed by closure of the epidermis with subcuticular or intercuticular suture. This is called a layered closure. The least amount of observable scar is created with a running, nonabsorbable, subcuticular suture with the least inflammatory response (i.e., polypropylene). However, this suture does require removal (see Table 2). An absorbable subcuticular suture (i.e., poliglecaprone 25) can be used but has a prolonged inflammatory phase during suture degradation. Small, clean, simple lacerations with minimal retraction can be managed with noninvasive techniques, including suture strips and cutaneous adhesive (i.e., Dermabond, Ethicon: Cornelia, GA). If external sutures are used in an interrupted, mattress, or running fashion, they should be removed as early as possible to minimize scarring from the suture. Staples can also be used and are preferred in the scalp to expedite closure and reduce pain of application and removal without compromising cosmesis.7 Vertical mattress sutures are used for extra strength and eversion of wound edges. Horizontal mattress sutures provide additional hemostasis (see Figs. 3 and 4).
TABLE 2 STANDARD SUTURE REMOVAL RECOMMENDATIONS | ||||||
|---|---|---|---|---|---|---|
|
Replantation
The most complex form of primary closure occurs when an appendage is amputated in such a way that it can be replanted. This is frequently performed for thumbs, fingers, hands, penises, and scalps. It has also been used for ears, nose, hands, feet, and entire extremities. Replantation requires repair of support structures (bones/tendons/fascia) followed by microvascular arterial and venous anastamoses and nerve repair. The skin is closed last. To be suitable for replantation, the amputated part must meet certain general criteria. Specific criteria are beyond the scope of this chapter. The amputated part must be present, preserved appropriately, recently amputated, minimally contaminated, and presumed to be viable. The patient must be medically stable and informed of the prognosis and need for prolonged postoperative care and therapy. Maximum ischemia time is frequently quoted to be 6 hours based on muscle damage at room temperature beyond 6 hours, but when preserved appropriately, cold ischemia can be extended even beyond 24 hours in amputated parts with minimal muscle (i.e., hands/digits). Preservation should include wrapping the part in sterile gauze moistened with lactated Ringers, sealing the part in a plastic bag, and placing the plastic bag in a container of water and ice at 4°C. Viability is compromised by crush injuries, avulsion injuries, and injuries at multiple levels.8,9
Secondary Intention
Healing by secondary intention is necessary when wounds are too large and/or too contaminated to close by other means. The wound is debrided and left open to heal secondarily. Healing is by a combination of contraction, proliferation of granulation tissue, and epithelialization. Epithelialization occurs from wound edges and skin appendages if still present. Secondary healing can be dramatically augmented by subatmospheric pressure therapy (see subsequent text).
Tertiary Intention
Healing by third intention is also known as delayed primary closure and is typically performed in smaller wounds that are contaminated. The patient undergoes initial debridement followed by open wound care for typically 3 to 5 days, at
which point the local phagocytic activity is maximized. The wound is then closed. These wounds are typically drained. This technique reduces infection rates in high-risk wounds. Wounds treated initially with wound care followed by skin grafting or flap closure as discussed in the next section could be considered a variation of tertiary intention healing.
which point the local phagocytic activity is maximized. The wound is then closed. These wounds are typically drained. This technique reduces infection rates in high-risk wounds. Wounds treated initially with wound care followed by skin grafting or flap closure as discussed in the next section could be considered a variation of tertiary intention healing.
AUTOGENOUS TISSUE RECONSTRUCTION
Many wounds require more complex forms of closure due to size of wound, exposed structures, or limited adjacent tissue. The options of reconstruction are best viewed as a ladder of increasing complexity, morbidity, and risks. The first principle of reconstruction is to start with the simplest approach with a reasonable possibility of success. The best treatment plan for any wound is always the technique with the best outcome with the least amount of sacrifice. If the simple technique fails, the more complex options are still available. That leads to the second principle of reconstruction; reconstructive efforts should not violate, or at least minimize violations of future reconstructive options. All reconstruction has physical costs in that uninjured tissues are used to cover the existing wound. The final principle of reconstruction is to minimize the harm or morbidity that the reconstruction costs the patient
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree