Repetitive throwing or other overhead activity places great stress on the shoulder. As a result, the shoulder is a common site of injury in athletes. Addressing throwing-related injuries requires an understanding of throwing biomechanics and pathology. Nonoperative treatment is directed at restoring strength, flexibility, and neuromuscular control to the entire kinetic chain. Surgery is indicated when nonoperative treatment fails, and is directed at correcting labral, capsular, and rotator cuff pathology.
Repetitive throwing places the shoulder in extreme positions in combination with tremendous stresses. In fact, professional pitchers generate up to 92 N·m of humeral rotation torque, greater than the torsional failure limit in human cadaveric shoulders. Throwers are therefore constantly at risk for injury.
Preventing injury begins with maintenance of the “kinetic chain” that coordinates transmission of force from the legs and trunk to the upper extremity. Studies show that muscle imbalances in the “kinetic chain” are common in shoulder impingement, rotator cuff tears, and instability. One study reported that throwers with labral tears commonly have back inflexibility, infraspinatus and teres minor weakness, and core weakness. Injuries to the foot and ankle, tightness of the muscles crossing the hip and knee, weakness of hip abductors and trunk stabilizers, and conditions altering spine alignment influence kinetic chain transmission.
Kinetic chain abnormalities can cause the shoulder to assume a hyperabducted, externally rotated position that moves the arm out of the “safe zone” of glenohumeral angulation described by Pink and Perry. Violent acceleration from hyperabduction increases compressive and shear forces on the glenoid, capsulolabral complex, and rotator cuff. This motion can injure the posterior capsule, damage and peel the labrum off the glenoid, tear and delaminate the rotator cuff, and tear and stretch the anterior restraints.
The phases of the baseball pitch have been extensively studied ( Fig. 1 ). During wind-up, hip stability allows proper balance in preparation for the early cocking, when the hips drive toward home plate. Early cocking ends as the lead foot lands and decelerates the driving lower extremity and trunk. Flaws during this stage include opening up, or abduction of the lead leg, causing poor pelvis rotation with consequent loss of velocity and increased anterior shoulder strain. Most injured pitchers experience pain during the late cocking phase, when the throwing humerus externally rotates from roughly 45° to 170°. During this time, the periscapular muscles, including the trapezius, rhomboids, levator scapula, and serratus anterior, stabilize the scapula, which functions as a fulcrum for energy transfer from the lower extremity and trunk to the humerus.

Periscapular muscle weakness also contributes to shoulder injury. To compensate for diminished serratus anterior strength, the thrower may drop the elbow, thus decreasing the degree of scapular rotation and elevation needed. If the pathologic process continues, the player may attempt to compensate further by moving the humerus behind the scapular plane worsening hyperabduction. Eccentric contraction of the subscapularis muscle then decelerates the externally rotating humerus, preparing it for acceleration.
In acceleration, the humerus reaches maximal external rotation and the lower extremity and trunk energy is transferred through the shoulder to the elbow and wrist as the body falls forward. Just before ball release, the arm internally rotates 80°, reaching peak angular velocities near 7000° per second. Within 0.05 seconds, the ball is released with speeds exceeding 90 mph. If the thrower opens up too quickly, positioning the elbow behind the plane of the scapula, the glenohumeral joint hyperangulates, resulting in more pronounced internal impingement.
In deceleration and follow-through in a right-hander, the ball is released and the right hip rises up and over the left leg. During this phase, the teres minor, infraspinatus, and scapular rotator muscles eccentrically contract, dissipating unused kinetic energy. The glenohumeral distraction force absorbed by the capsule and posterior rotator cuff reaches 1 to 1.5 times the thrower’s body weight. Eccentric contraction by the scapular rotators continue to decelerate the arm, and the posterior capsule experiences tension as the arm adducts.
Asymptomatic throwing shoulder adaptation
Overall Motion
The dominant shoulder of a thrower exhibits increased external rotation and diminished internal rotation compared with the contralateral arm. In asymptomatic throwers, the total arc of shoulder motion is maintained but shifted by 10° into external rotation.
Adaptations in bone and soft tissue are responsible for increased external rotation. Crockett and colleagues showed that professional pitchers show 17° greater humeral retroversion in their throwing shoulder compared with their nondominant shoulder. During development, humeral retroversion decreases from 78° to 30°, and repetitive throwing during growth is hypothesized to restrict this physiologic derotation. Soft tissue adaptations also occur. The anterior capsule and glenohumeral ligaments become lax, whereas the posterior capsule and glenohumeral ligaments stiffen. Repetitive microtrauma to the anterior capsule, particularly during the cocking phase of throwing, leads to anterior laxity and more external rotation.
Injury Patterns
The typical motions and forces around the glenohumeral joint during throwing lead to predictable injury patterns. Superior labral tears are frequent and commonly extend into the posterosuperior labrum. The posterior supraspinatus and anterior infraspinatus are usually partially torn with occasional intratendinous delamination. Andrews and colleagues noted that labral tears were present in 100% of 36 competitive athletes with articular-sided partial-thickness rotator cuff tears, of whom 64% were baseball pitchers. In addition, the anterior capsule may become pathologically lax and the posterior capsule pathologically contracted.
Although the injury patterns are consistent, the exact mechanism is debated. Andrews and colleagues originally theorized that articular-sided tears resulted from repetitive large eccentric forces to the supraspinatus and infraspinatus tendons during the deceleration phase of throwing. Davidson and colleagues hypothesized that repetitive contact between the articular side of the rotator cuff and the posterosuperior glenoid in late cocking caused tears. This pathology is aggravated by anterior subluxation and instability, particularly when dynamic stabilizers fatigue. Burkhart and colleagues proposed that the primary cause of rotator cuff and labral lesions was posterior capsular contracture, leading to posterosuperior migration of the humeral head. This article describes the leading theories.
Internal impingement theory
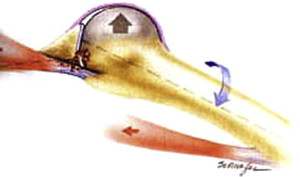
Walch and colleagues initially described internal impingement as occurring in the 90° abducted and 90° externally rotated position. In this position, the posterosuperior rotator cuff contacts the posterosuperior glenoid labrum and can be pinched between the labrum and greater tuberosity ( Fig. 2 ). Although physiologic in a static position, forceful and repeated contact of the undersurface of the rotator cuff and the superior labrum during overhead activity can explain the development of partial-thickness rotator cuff tears and superior labrum anterior posterior (SLAP) lesions, which commonly coexist in throwers. In addition, kinetic chain abnormalities previously described can exacerbate this process when throwers compensate for poor mechanics through “opening up” or hyperangulating the arm.
Posterior capsular contracture theory
Burkhart and colleagues proposed posterior capsular contracture as a consequence of throwing. They reasoned that the posterior capsule must withstand tensile forces of up to 750 N during the deceleration and follow-through phases of throwing. These posterior tensile forces are resisted by both the eccentric contraction of the rotator cuff, primarily the infraspinatus, and the posteroinferior capsule (posterior band of the inferior glenohumeral ligament [IGHL]). With repetitive infraspinatus eccentric contraction, the muscle and the posteroinferior capsule become hypertrophied and stiff. The posterior contracture shifts the center of rotation of the shoulder to a more posterosuperior location, creating posterosuperior instability with shoulder in abduction and external rotation, which has been supported by biomechanical cadaver research. The humeral head can consequently externally hyperrotate, producing increased shear in the rotator cuff tendon and more pronounced internal impingement. In addition, a peel-back phenomenon occurring during late cocking, consisting of a torsional force applied to the biceps anchor, contributes to SLAP lesion development.
Scapulothoracic function
The scapula plays a critical role in energy transfer from the trunk to the humerus. In the asymptomatic thrower, adaptive scapulothoracic changes leading to scapular asymmetry have been described. Altered static and dynamic scapular mechanics arise from overuse and weakness of scapular stabilizers and posterior rotator cuff muscles. With the arm hanging at the side, the throwing shoulder’s scapula has increased upward rotation (abduction), internal rotation (protraction), antetilting in the sagittal plane and inferior translation. During cocking, when the humerus is terminally externally rotated and abducted, upward scapular rotation helps maintain glenohumeral articular congruency. Weakness, inflexibility, or imbalance of the periscapular and posterior rotator cuff muscles disturb the normal anatomic static and dynamic relationships of the scapula. Aberrant scapulothoracic motion has been called scapular dyskenesis . The abnormally positioned thrower’s scapula has been labeled SICK (scapular malposition, inferior medial border prominence, coracoid pain, and dyskinesis of scapular movement) scapula by Burkhart and colleagues.
The SICK scapula predisposes the shoulder to labral and rotator cuff tears because the scapula sits in a protracted and upwardly tilted position, causing the glenoid to face anterior and superior. This position leads to three developments: anterior tension, posterior compression, and increased glenohumeral angulation. First, with glenoid protraction, the anterior band of the IGHL tightens, limiting anterior translation of the humeral head and, over time, becoming susceptible to chronic strain. Second, simultaneously, the posterior edge of the glenoid is brought toward the humerus, placing the posterosuperior labrum and rotator cuff at risk for injury. Finally, excessive protraction increases glenohumeral angulation. The thrower with increased glenohumeral angulation will find that the “arm lags behind the body.” Excessive external rotation in this setting has two harmful consequences. One, it exacerbates the aforementioned biceps peel back effect. Two, with preexisting scapular protraction, external rotation and abduction produce posterosuperior glenoid impingement.
A cascade of pathologic entities explain injuries associated with the SICK scapula: coracoid pain from pectoralis minor contracture and tendinopathy, superior medial angle scapular pain from levator scapula insertional tendinopathy, subacromial origin pain from acromial malposition and decreased subacromial space from upward tilting, acromioclavicular joint pain caused by anterior joint incongruity, sternoclavicular pain, thoracic outlet syndrome radicular pain, and subclavian vascular problems such as arterial pseudoaneurysm or venous thrombosis.
In summary, anterior instability, posterior capsular contracture, and internal impingement in throwers are influenced by alterations in the kinetic chain and scapulothoracic thoracic function. Shoulder pathology should be viewed as a syndrome because the injury cascade is a continuum of interrelated pathomechanics. Although when viewed independently some of the current popular theories on the cause of specific throwing-related shoulder injuries may conflict, they complement each other when they are considered elements of a pathologic continuum.
Evaluation of the overhead athlete
History
A wide variety of disorders may present in the thrower, including those that affect the kinetic chain such as the hip, core, and low back. The goal should be to accurately diagnose and efficiently direct treatment. Initial symptoms may be vague, such as loss of control, velocity, or difficulty warming up. Typical shoulder-related symptoms include anterosuperior or posterosuperior shoulder pain in the late cocking phase. Popping, locking, and snapping may occur with unstable labral tears. Instability symptoms may be related to rotator cuff dysfunction and excessive anterior capsular laxity.
Physical Examination
A systematic physical examination should be performed to assess the knee, hip, and low back. Functional movement may be assessed with single leg squats for hip and trunk control, muscle imbalance, and inflexibilities.
Muscular atrophy and scapular winging should be noted. Tenderness should be assessed at glenohumeral joint lines, the acromioclavicular joint, the long head of the biceps tendon, and the coracoid process. Tenderness over the long head of the biceps tendon suggests tendonitis or a SLAP tear. Coracoid process tenderness suggests pectoralis minor tendonitis or tightness, which has been correlated with scapular protraction and dyskenesis.
Active and passive range of motion of the glenohumeral and scapulothoracic joints are measured. Forward elevation in the plane of the scapula, external rotation, and internal rotation (in 0° of abduction, this is the highest spinal level the patient can reach with thumb behind the back) in both 0° and 90° of abduction should be documented. Kibler measured scapular asymmetry through comparing the distance from the inferior angle of the scapula to the spinous process of the thoracic vertebra in the same horizontal plane (the reference vertebra) in three test positions. In position one, the arm is at the side. In position two, the humerus is internally rotated and abducted 45°, as the hands are placed on the hips. In position three, the shoulder is abducted further to 90°. An asymmetrical difference of greater than 1.5 cm determines a positive lateral scapular slide test (LSST).
With the scapular assistance test, scapular upward rotation is assisted through manually stabilizing the upper medial scapular border and rotating the inferomedial border as the arm is abducted. A positive test will relieve symptoms of impingement, clicking, or rotator cuff weakness present without the manual assistance. The scapular retraction test is performed through manually stabilizing the medial border of the scapula. When manual stabilization increases strength in patients with apparent rotator cuff weakness and a protracted scapula, scapular dyskenesia is present.
Manual muscle strength testing should aim to isolate the muscle being tested and compare the injured with the contralateral, uninjured side. The supraspinatus can be isolated in the “empty can” position. The subscapularis is best assessed using the “lift off” test, or the internal rotation lag sign, which is more sentsitive.
A proper examination assesses range of motion of both shoulders in both adduction and 90° of abduction. An overhead athlete will typically have reduced internal rotation and increased external rotation. The Jobe’s relocation test is also a provocative maneuver that reproduces the symptoms of internal impingement. In this test, the patient is supine and the arm is placed into 90° of abduction and 10° of forward flexion, and the shoulder is forced anteriorly. Pain represents a positive test. Pain subsequently subsides with a posteriorly directed force.
Many tests have been described to assist in diagnosing SLAP lesions. The active compression test has good sensitivity and specificity for type II SLAP lesions. The arm is positioned in 15° of adduction and 90° of forward elevation. The examiner applies downward force on the forearm while the hand is both pronated and supinated, and compares the resulting pain and weakness. A positive test occurs when the patient reports pain that is worse in the pronated position. The compression–rotation test is similar to McMurray’s test of the knee. It is performed through compressing the glenohumeral joint and then rotating the humerus in an attempt to trap the labrum in the joint. This test should be performed in the supine position, so that the patient is more relaxed.
Speed’s biceps tension test is also sensitive for SLAP lesions. This test is performed through having the patient resist downward pressure with the arm in 90° of forward elevation, with the elbow extended and the forearm supinated. Although this test is more suggestive of biceps tendon damage, an unstable biceps anchor will cause the test to elicit pain. A positive apprehension relocation sign for posterior shoulder pain may suggest a SLAP lesion in the posterior labrum as part of a spectrum of internal impingement.
Many other tests have been described, but the authors have found them to be less useful. Finally, external impingement should be assessed with impingement tests such as the Neer and Hawkins tests.
Imaging
Radiographic evaluation includes the standard three views of the shoulder (anteroposterior, axillary, and outlet views) to help exclude other bony abnormalities. MRI-enhanced arthrography outperforms plain MRI when diagnosing SLAP lesions with sensitivity of 89%, a specificity of 91%, and an accuracy of 90%. The diagnostic feature of the MR arthrogram is contrast between the superior labrum and the glenoid that extends around and under the biceps anchor on the coronal oblique view ( Fig. 3 ). The axial views visualize possible extension into the anterior and or posterior labrum. Partial thickness rotator cuff tears will also be identified (see Fig. 3 ).

Some experts have recommended MRI with the shoulder in both the abducted and abducted and externally rotated position. These views may further enhance visualization of the articular side of the rotator cuff and superior glenoid, and may be helpful in diagnosing delaminating tears of the rotator cuff. Up to 40% of professional pitchers have completely asymptomatic partial articular-sided supraspinatus tendon avulsion (PASTA) lesions.
Evaluation of the overhead athlete
History
A wide variety of disorders may present in the thrower, including those that affect the kinetic chain such as the hip, core, and low back. The goal should be to accurately diagnose and efficiently direct treatment. Initial symptoms may be vague, such as loss of control, velocity, or difficulty warming up. Typical shoulder-related symptoms include anterosuperior or posterosuperior shoulder pain in the late cocking phase. Popping, locking, and snapping may occur with unstable labral tears. Instability symptoms may be related to rotator cuff dysfunction and excessive anterior capsular laxity.
Physical Examination
A systematic physical examination should be performed to assess the knee, hip, and low back. Functional movement may be assessed with single leg squats for hip and trunk control, muscle imbalance, and inflexibilities.
Muscular atrophy and scapular winging should be noted. Tenderness should be assessed at glenohumeral joint lines, the acromioclavicular joint, the long head of the biceps tendon, and the coracoid process. Tenderness over the long head of the biceps tendon suggests tendonitis or a SLAP tear. Coracoid process tenderness suggests pectoralis minor tendonitis or tightness, which has been correlated with scapular protraction and dyskenesis.
Active and passive range of motion of the glenohumeral and scapulothoracic joints are measured. Forward elevation in the plane of the scapula, external rotation, and internal rotation (in 0° of abduction, this is the highest spinal level the patient can reach with thumb behind the back) in both 0° and 90° of abduction should be documented. Kibler measured scapular asymmetry through comparing the distance from the inferior angle of the scapula to the spinous process of the thoracic vertebra in the same horizontal plane (the reference vertebra) in three test positions. In position one, the arm is at the side. In position two, the humerus is internally rotated and abducted 45°, as the hands are placed on the hips. In position three, the shoulder is abducted further to 90°. An asymmetrical difference of greater than 1.5 cm determines a positive lateral scapular slide test (LSST).
With the scapular assistance test, scapular upward rotation is assisted through manually stabilizing the upper medial scapular border and rotating the inferomedial border as the arm is abducted. A positive test will relieve symptoms of impingement, clicking, or rotator cuff weakness present without the manual assistance. The scapular retraction test is performed through manually stabilizing the medial border of the scapula. When manual stabilization increases strength in patients with apparent rotator cuff weakness and a protracted scapula, scapular dyskenesia is present.
Manual muscle strength testing should aim to isolate the muscle being tested and compare the injured with the contralateral, uninjured side. The supraspinatus can be isolated in the “empty can” position. The subscapularis is best assessed using the “lift off” test, or the internal rotation lag sign, which is more sentsitive.
A proper examination assesses range of motion of both shoulders in both adduction and 90° of abduction. An overhead athlete will typically have reduced internal rotation and increased external rotation. The Jobe’s relocation test is also a provocative maneuver that reproduces the symptoms of internal impingement. In this test, the patient is supine and the arm is placed into 90° of abduction and 10° of forward flexion, and the shoulder is forced anteriorly. Pain represents a positive test. Pain subsequently subsides with a posteriorly directed force.
Many tests have been described to assist in diagnosing SLAP lesions. The active compression test has good sensitivity and specificity for type II SLAP lesions. The arm is positioned in 15° of adduction and 90° of forward elevation. The examiner applies downward force on the forearm while the hand is both pronated and supinated, and compares the resulting pain and weakness. A positive test occurs when the patient reports pain that is worse in the pronated position. The compression–rotation test is similar to McMurray’s test of the knee. It is performed through compressing the glenohumeral joint and then rotating the humerus in an attempt to trap the labrum in the joint. This test should be performed in the supine position, so that the patient is more relaxed.
Speed’s biceps tension test is also sensitive for SLAP lesions. This test is performed through having the patient resist downward pressure with the arm in 90° of forward elevation, with the elbow extended and the forearm supinated. Although this test is more suggestive of biceps tendon damage, an unstable biceps anchor will cause the test to elicit pain. A positive apprehension relocation sign for posterior shoulder pain may suggest a SLAP lesion in the posterior labrum as part of a spectrum of internal impingement.
Many other tests have been described, but the authors have found them to be less useful. Finally, external impingement should be assessed with impingement tests such as the Neer and Hawkins tests.
Imaging
Radiographic evaluation includes the standard three views of the shoulder (anteroposterior, axillary, and outlet views) to help exclude other bony abnormalities. MRI-enhanced arthrography outperforms plain MRI when diagnosing SLAP lesions with sensitivity of 89%, a specificity of 91%, and an accuracy of 90%. The diagnostic feature of the MR arthrogram is contrast between the superior labrum and the glenoid that extends around and under the biceps anchor on the coronal oblique view ( Fig. 3 ). The axial views visualize possible extension into the anterior and or posterior labrum. Partial thickness rotator cuff tears will also be identified (see Fig. 3 ).
Some experts have recommended MRI with the shoulder in both the abducted and abducted and externally rotated position. These views may further enhance visualization of the articular side of the rotator cuff and superior glenoid, and may be helpful in diagnosing delaminating tears of the rotator cuff. Up to 40% of professional pitchers have completely asymptomatic partial articular-sided supraspinatus tendon avulsion (PASTA) lesions.
Management of specific shoulder conditions in athletes
Nonoperative Treatment
Nonoperative treatment is directed at all observed pathology, such as correcting lower extremity, hip, core, and low back disorders, in addition to scapular function, restoring shoulder range of motion, strength, and flexibility. Several phases of rehabilitation can be used, progressing from inflammation reduction, to range of motion restoration, muscle strengthening, and soft tissue flexibility, and finishing with proprioception and neuromuscular control and a comprehensive return to throwing program. Although nonoperative treatment strategies have been presented comprehensively in other sources, the following discussion focuses on several important pathologic features.
Correction of pathologic posterior capsular contracture is critical. Nonoperative management has proved successful in the management of glenohumeral internal rotation deficit, reported as greater than 20°. Some authors have detailed a series of exercises that, theoretically, improve posterior capsular contracture and fairly reliably decrease glenohumeral internal rotation deficit. These exercises include “sleeper stretches,” which require athletes to lie on their side with the shoulder in 90° of flexion, in neutral rotation, with the elbow also in 90° of flexion. The shoulder is then passively internally rotated by pushing the forearm toward the table around the fixed point of the elbow. In the horizontal adduction stretch, the arm is horizontally adducted while the scapula is stabilized. The pectoralis minor should also be stretched, which can be performed by placing a rolled towel between the shoulder blades while the patient is supine, and steadily pushing posteriorly on the shoulders.
Treatment for SICK scapula consists of scapular stabilizer muscular strengthening, and re-education. The involved side is addressed first, using closed chain exercises followed by open chain exercises. The kinetic chain is incorporated into the rehabilitation. Scapular rehabilitation has been successful in returning patients with SICK scapula to their previous level of competitive play.
For patients with an acute injury, such as a development of a SLAP and or partial thickness rotator cuff tear, initial treatment is directed at eliminating pain, restoring motion, correcting strength deficits, and restoring normal synchronous muscle activity. Initial treatment involves rest from provocative activities, anti-inflammatory medication, and therapeutic modalities. Strengthening is initiated once pain is resolved. For throwing athletes, a gradual return to throwing may begin as muscular balance and range of motion are restored. Failure of a nonoperative program, early suspicion of significant mechanical dysfunction, or seasonal timing may direct treatment toward surgical intervention.
Classic subacromial bursitis symptoms and external impingement may also be present and can be treated with nonsteroidal anti-inflammatory drugs or subacromial corticosteroid injection. Rotator cuff strengthening may proceed only after proper capsular elasticity and scapular dynamics have been restored.
Examination Under Anesthesia and Arthroscopic Evaluation
When the decision is made for surgery, the shoulder should be tested for translation and range of motion under anesthesia because it provides useful laxity measurements. Often, the office examination may be clouded by patient apprehension, muscle tightness, or pain. Examination under anesthesia provides an unobstructed examination and can provide useful preoperative information.
The shoulder should be tested for translation in multiple planes. The arm should be positioned in 90° of abduction and 30° of forward flexion. An axial load should be applied along the humeral shaft, and the humerus is translated in all planes. Translation is graded based on the amount of humeral head translation relative to the glenoid. Grade 1 represents mild translation, grade 2 translates to the glenoid rim, grade 3 translation produces a dislocation that spontaneously reduces, and grade 4 represents translation that results in a fixed dislocation. Range of motion should also be evaluated in all planes, and comparison is ideally made to the contralateral limb.
The diagnosis of SLAP lesions ultimately relies on arthroscopic evaluation. Types I, III, and IV lesions are obvious when fraying or splitting of the labrum is noted. Viewing the joint from both the anterior and posterior portals is mandatory to entirely assess the degree of involvement. Diagnosis of type II lesions is more difficult. The normal superior labrum often has a small cleft between it and the glenoid, especially in the setting of a meniscoid labrum. The stability of the biceps anchor is determined through probing and attempting to elevate the labrum and biceps. The glenoid articular cartilage usually extends medially over the superior corner of the glenoid. Absence of cartilage in this region indicates labral detachment. Traction on the biceps tendon will show any loss of integrity at the superior labral attachment.
Burkhart and Morgan described the arthroscopic examination for peel-back. The arm is placed in a throwing position and, with humeral external rotation, the labrum peels away from the posterosuperior glenoid.
A comprehensive and methodical diagnostic arthroscopy is performed visualizing the entirety of the joint with the assistance of a probe. Typically, two portals are used for the diagnostic arthroscopy: a posterior portal and a rotator interval portal. When planning a SLAP repair, both portals should be made relatively laterally to allow access to the glenoid rim.
Depending on the nature of the expected pathology, the patient is placed into the beach chair position for rotator cuff and external impingement, or the lateral decubitus position for labral tears and capsular laxity. First, the glenoid and humeral head are evaluated for any chondral wear. Next, the biceps is evaluated at its superior attachment and throughout its course in the rotator interval. The probe is used to pull the tendon into the joint and evaluate for synovitis or fraying. Next, the superior and anterior labrum is evaluated from 12 o’clock to 6 o’clock. The arthroscope is then placed in the axillary pouch and the recess evaluated for hemosiderin deposits, synovitis, or excessive volume. At this time, the posterior labrum can be visualized and probed.
Visualization through the anterior portal improves visualization of the posterior labrum and posterior IGHL, and should be performed when any posterior labral pathology is suspected. The arm may be brought into 90° of abduction and maximal external rotation, with the camera in the posterior viewing portal, and abnormal impingement of the rotator cuff and posterosuperior labrum visualized. Evidence of peel-back may also be seen. Finally, the capsule and anterior glenohumeral ligaments can be fully assessed, and the degree of capsular laxity or tears determined. Finally, the subscapularis tendon is evaluated for its integrity in internal and external rotation.
The rotator cuff should be carefully evaluated. In the thrower, special attention should be given to the undersurface of the rotator cuff at the junction between the supraspinatus and infraspinatus tendons. Tears of the rotator cuff at this location are common and care should be taken to evaluate for intratendinous delamination.
The subacromial space should be entered and examined carefully for bursitis and evidence of external impingement, such as fraying or ossification of the coracromial ligament or inflammation of the bursa. Once a careful examination under anesthesia and an arthroscopic evaluation is performed, the surgeon may proceed with operative fixation of the pathology at hand.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







