Management of Posterolateral Corner Injuries
Richard J. Thomas
Mark D. Miller
DEFINITION
The posterolateral corner (PLC) of the knee is a complex area, both anatomically and functionally, that has the potential to cause great disability when injured.
Injuries to the structures of the PLC are uncommon, accounting for only 2% of all acute ligamentous knee injuries.6
Because of the high incidence of combined ligament injuries associated with PLC injuries,2 other ligament injuries in the knee always should be suspected when treating the PLC.
Conversely, cruciate ligament reconstructions have a tendency to fail if PLC injuries are left untreated,8,17 so one must always have a high index of suspicion for PLC injuries when treating other injuries in the knee.
The significance of a PLC knee injury can be great.
Chronic instability due to the untreated PLC injury can be debilitating.
The complex biomechanical relationships among the structures of the PLC are important in resisting varus and external rotation forces.
Insufficiency in the posterolateral structures of the knee can lead to a varus-thrust gait and the sensation of instability, especially when the knee is in extension during the toe-off phase of walking.2
The convexity of the lateral tibial plateau and lateral femoral condyle may contribute to this instability.17
This instability may hinder stair-climbing or cutting activities, and patients may complain of lateral knee pain.
Chronic PLC insufficiency also may lead to tricompartmental degenerative joint disease.2
An increase in patellofemoral joint contact pressure has been found to occur with PLC and posterior cruciate ligament (PCL) sectioning in cadaveric studies.26
ANATOMY
Before treating a patient with a PLC injury, one must be familiar with the complex anatomy of the area.
The PLC is made up of both dynamic and static stabilizers.5
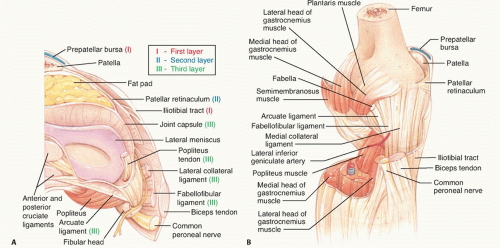
The superficial layer is made up of the iliotibial (IT) tract anteriorly and the biceps femoris posteriorly.
The common peroneal nerve lies deep and posterior to the biceps femoris in this layer at the level of the distal femur.
The IT tract or band, which inserts on Gerdy tubercle on the tibia, is tight and moves posteriorly in knee flexion. It actually places an external rotation force on the tibia during knee flexion. During knee extension, the IT band moves anteriorly and becomes less taut. Because of its relaxed state in knee extension, this structure rarely is injured in PLC injuries, so it is a good reference point for the location of other structures in surgery.
The middle layer of the PLC consists of the quadriceps retinaculum anteriorly, the patellofemoral ligaments posteriorly, and the patellomeniscal ligament.25
These structures add accessory static stability to the PLC.
The deep layer, which is the most important (FIG 1B), consists of the lateral part of the joint capsule and the coronary ligament, which inserts on the lateral meniscus; the popliteus tendon and the popliteofibular ligament; the arcuate ligament; the LCL; and the fabellofibular ligament.25
The popliteus originates on the posterior tibia, passes through the hiatus of the coronary ligament, and inserts on the lateral femoral condyle.2 It also has attachments to the lateral meniscus.
The popliteofibular ligament exists as a direct static attachment of the popliteus tendon from the posterior fibular head to the lateral femoral epicondyle.
The arcuate ligament is a Y-shaped ligament that reinforces the posterolateral capsule of the knee and runs from the fibular styloid to the lateral femoral condyle. In radiographs, the arcuate fracture shows an avulsion of this ligament off of the fibular styloid.14
The LCL originates on the lateral epicondyle of the femur and inserts on the fibular head. This ligament is the primary static restraint to varus stress from 0 to 30 degrees of knee flexion.6,7,17 The LCL becomes progressively more lax in greater degrees of flexion, however. Aponeurotic layers of the biceps femoris provide tension to the LCL to assist in dynamic resistance to varus stress.7,17 The LCL also provides resistance to external rotation stress.2
Much anatomic variation has been noted in the structures of the deep layer, especially the arcuate and fabellofibular ligaments.25
Hughston et al 9 described the importance of an arcuate ligament complex consisting of the LCL, arcuate ligament, popliteus, and the lateral head of the gastrocnemius. This complex acts as a “sling” of static and dynamic restraint to rotation of the lateral tibiofemoral articulation.
PATHOGENESIS
PLC knee injuries most commonly are caused by sports injuries (40%), motor vehicle accidents, and falls.2,5
Any mechanism that can cause a knee dislocation theoretically can cause an injury to the PLC.
The most common mechanism for an isolated PLC injury is hyperextension of the knee with a varus moment. This mechanism can be caused by blunt posterolaterally forced trauma to the medial proximal tibia, such as a helmet to the knee in football.
Other mechanisms of injury include hyperextension alone, hyperextension with an external rotation force, a severe varus force alone, or a severe external rotation torque to the tibia.
As mentioned earlier, an isolated PLC knee injury is rare.6
A flexed knee with tibial external rotation and posterior translation can cause a PCL/PLC combined injury.
NATURAL HISTORY
Posterolateral knee injuries rarely occur as isolated ligament disruptions.
They most often are associated with injury to the PCL, the anterior cruciate ligament (ACL), or both. Therefore, the true natural history of these injuries is unknown.
If left untreated, they will contribute to failure of other ligament reconstruction.
Repair, and often supplementation with exogenous grafts, is recommended in all cases of combined PLC injury.
PATIENT HISTORY AND PHYSICAL FINDINGS
Methods for examining the PLC include the following:
Dial test. More than 10 degrees difference between limbs is consistent with ligamentous PLC injury.28 Increased rotation at 30 degrees but not at 90 degrees indicates isolated PLC injury. Increased rotation at both 30 degrees and 90 degrees indicates PLC and PCL injuries.
Posterolateral external rotation test.25 Increased posterior translation and external rotation at 90 degrees are suspicious for PLC or PCL injury. Subluxation at 30 degrees is consistent with isolated PLC injury.
Posterior drawer test (PCL testing). More than 10 mm translation is highly suggestive of multiligamentous knee injury.
Varus stress test (LCL testing). An isolated tear of the LCL causes maximal varus angulation at 30 degrees.
Quadriceps active test. Forward translation of the tibia after attempted knee extension is positive for PCL insufficiency (reduction of posterior tibial sag).
Gait. The patient may walk with a slightly flexed knee to avoid pain and instability with hyperextension of the knee.25 Varus thrust also may be present.
Reverse pivot shift test. Palpable shift of the lateral tibial plateau is positive but not specific for PLC injury. This test is difficult to perform on the awake patient.
External rotation recurvatum test.2 Hyperextension and increased varus of the knee and external rotation of the tibia are positive for PLC injury.
Range of motion (ROM). The normal range is 0 to 135 degrees of motion. Loss of extension may be due to a displaced meniscus tear. Loss of flexion may be due to effusion.
Effusion. A large effusion suggests other intra-articular pathology, such as an ACL or PCL tear or a peripheral meniscus tear. Effusion may be diminished if the capsule is torn.
Neurovascular examination (serial). The incidence of popliteal artery injury is increased in knee dislocations. An arteriogram should be obtained if the vascular examination
is different from that in the contralateral leg. The incidence of peroneal nerve injury is increased by 10% to 33% with PLC injuries.1,6,16
It is important to obtain a good history from the patient with an acute PLC injury. A history of a tibiofemoral dislocation should cause suspicion of a PLC injury.
Pain and swelling of the posterolateral knee are common.
A rapid knee effusion suggests the possibility of concurrent intra-articular pathology.
Patients with chronic posterolateral instability commonly present with the sensation of instability with the knee in extension and lateral or posterolateral aching pain in the knee.
PLC injuries can be graded5 as 1, 2, or 3.
Grade 1 injuries involve minimal tearing of the ligaments and are not associated with abnormal joint motion.
Grade 2 injuries have partial tearing but still have no abnormal joint motion.
Grade 3 injuries have complete tearing of the ligaments and abnormal joint motion.
Hughston et al 28 graded PLC injuries based on ligamentous instability. Cases of mild, moderate, and severe instability are graded as 1+, 2+, and 3+, respectively.
Because PLC knee injuries have such a high association with combined ligament injuries, a careful examination for other knee pathology is necessary.
PCL injury can be recognized by a positive posterior drawer test, tibial sag or recurvatum, and hemarthrosis.
A positive Lachman test is the most sensitive test for an ACL tear. The examiner should not be fooled by a false end point caused by a tight effusion or a displaced meniscal tear. A positive pivot shift also is a sensitive test for an ACL tear, although it is difficult to perform on an acute patient because of discomfort and apprehension.
Meniscal tears can also be associated with PLC injuries. Joint line tenderness is the most sensitive test for meniscal tears. A lateral meniscus tear may give lateral-sided knee pain, which could be confused with a posterolateral knee injury. Mechanical symptoms also raise concern for meniscal tears. Loss of full extension of the knee hints at the possibility of a locked bucket-handle meniscus tear.
Although it is rare to have LCL and medial collateral ligament (MCL) tears from the same injury, one must examine all ligaments after trauma to the knee. The MCL is tested by valgus stress at 0 and 30 degrees of knee flexion. Medial knee tenderness and ecchymosis are often present in an MCL injury.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The initial diagnostic imaging examination should begin with standard anteroposterior (AP) and lateral radiographs of the knee.
Laprade and Wentorf17 recommend obtaining full-length standing AP radiographs to evaluate for varus malalignment in chronic patients.
Plain radiographs also can be obtained to evaluate associated fractures, such as an arcuate avulsion fracture of the fibular head, a Gerdy tubercle avulsion, and a Segond fracture, which is an avulsion of the lateral capsule off of the tibia.5
Segond fractures typically are thought to be associated with ACL injuries, but they also can be associated with posterolateral ligament injuries.
Patellofemoral or tricompartmental arthritis may be associated with chronic instability. Typically, the lateral compartment is more involved than the medial compartment.2
An effusion in the suprapatellar pouch also can be visualized on plain radiographs and hints at the presence of an intra-articular pathology, such as an ACL or PCL tear.
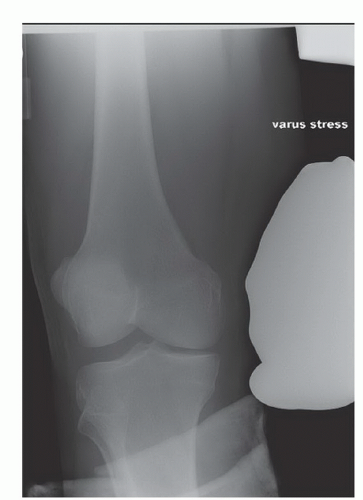
Varus stress films may be used to evaluate the integrity of the LCL as well (FIG 2).
MRI is useful in evaluating the soft tissues of the knee and in looking for bone contusions or edema.
Laprade et al 14 recommend obtaining not only the standard coronal, sagittal, and axial cuts of the knee but also coronal oblique 2-mm thin cuts to include the entire fibular head and styloid, to better evaluate the popliteus tendon and the LCL.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree