Management of Pelvic Discontinuity
Scott M. Sporer
Jonathan Christy
Case Presentation
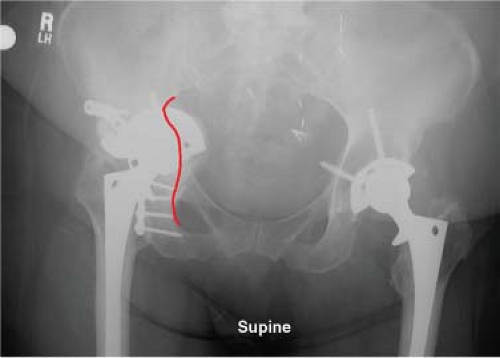
A 75-year-old female 8 years status post primary total hip arthroplasty (THA) and 9 months following an acetabular revision presents with a 2-month history of right hip pain. She was told that her initial socket had loosened and that a newer component with a porous surface was used to reconstruct the defect. She was also told that at the time of surgery, the surgeon noticed that there was a large amount of bone loss and that the upper portion of the pelvis was not connected to the lower portion. As a result, the surgeon placed a plate on the posterior portion of the pelvis. She presents to the office in a wheelchair unable to bear weight with the radiographs shown in (Fig. 116.1). Her laboratory indices for infection (erythrocyte sedimentation rate [ESR] and C-reactive protein [CRP]) were normal.
Introduction
The evaluation and treatment of patients with a failed THA requires a careful systematic approach. A stepwise workup is essential to guarantee an accurate diagnosis, appropriate preoperative planning, and the selection of the optimal reconstruction options to maximize the potential for a successful clinical outcome. This chapter will focus on the identification and management of pelvic discontinuity; one of the most challenging aspects of acetabular revision surgery (1). Pelvic discontinuity has been described by Berry et al. as “an uncommon condition occurring in association with THA when the hemipelvis is separated superiorly and inferiorly by loss of host bone or a fracture through the acetabular columns (2).”
Epidemiology of Revision Hip Arthroplasty
Approximately 300,000 primary THA procedures are performed annually in the United States (3), and that number is expected to increase as the population ages and as younger patients are considered for the procedure. Consequently, the burden of revision THA is projected to increase exponentially (4). Multiple studies have shown that in addition to the substantial increase in prevalence of primary THA procedures, the rates of revision procedures are expected to rise as well (5,6,7). Despite attempts to improve implant design and evade the previous pitfalls of early reconstruction techniques, the prevalence of revision hip arthroplasty cases has not declined (5). In the United States alone, 46,000 hip revisions were performed in 2004 and this number is expected to more than double by 2030 (6). With the widespread use of cementless acetabular components, more and more patients will undoubtedly present with extensive bone loss at the time of revision because of the effects of asymptomatic osteolysis and stress shielding.
As stated above, pelvic discontinuity is a rare clinical entity and thus hard to establish an accurate prevalence. Tanzer et al. (8) reported the results of 140 acetabular revisions in which only three hips had a pelvic discontinuity. Moreland and Bernstein (9) reported that of 175 acetabular revisions only two had a pelvic discontinuity. Berry et al. (1) published data from their institution and found that only 0.9% of all hip revisions had been operatively treated for a diagnosis of pelvic discontinuity. In this series, rheumatoid arthritis, female sex, prior pelvic
radiation, and severe bone loss were considered risk factors for a pelvic discontinuity.
radiation, and severe bone loss were considered risk factors for a pelvic discontinuity.
Patient Evaluation
A thorough preoperative patient assessment is vital in cases requiring acetabular component revision. Infectious etiologies that could preclude a definitive single-stage reconstruction should always be ruled out through the use of baseline serology studies (ESR/CRP)(10). Elevated serum inflammatory markers should prompt a preoperative hip aspiration. Weight-bearing pain is the most common complaint among patients with a pelvic discontinuity along with an antalgic gait and leg length inequality.
X-Ray Evaluation
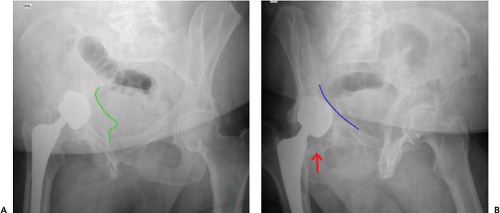
In addition to obtaining a good history and physical examination as stated above, plain radiographs and advanced imaging modalities are useful in defining bone loss both in their extent and location. Anterior–posterior (AP) pelvis, AP hip, and frog-leg lateral views of the involved hip can be supplemented with Judet views for evaluation of the acetabular columns (Fig. 116.2A,B). A shoot-through lateral view can also help assess not only acetabular component anteversion but also may yield clues regarding the integrity of the posterior column (Fig. 116.3). These views can often be sufficient to give clues as to the underlying cause of the failure. Three-dimensional computed tomography (CT) can be helpful in quantifying the presence and severity of osteolytic lesions and bone loss (Fig. 116.4A,B). Knowledge obtained from these studies helps to classify the acetabular defect and thereby guide surgical management.
A pelvic discontinuity can frequently be identified on preoperative plain films. The hallmarks of a pelvic discontinuity include a fracture line which encompasses both columns as well as rotation and medialization of the inferior hemipelvis in relation to the superior hemipelvis (Fig. 116.5). Rotation of the inferior hemipelvis can frequently be observed as asymmetry between the ipsilateral and contralateral obturator foramen.
Classification of Acetabular Defects
The Paprosky acetabular defect classification system is based on four radiographic criteria obtained from an AP pelvis radiograph: superior hip center migration, ischial osteolysis, the position of the implant relative to the Kohler line (Fig. 116.1), and osteolysis in the area of the teardrop (11). Patients demonstrating a type IIC or type IIIB acetabular defect are at the greatest risk of having an associated
pelvic discontinuity. Type IIC defects are those that have distortion of the superior rim less than 3 cm of superolateral migration with medial migration past Kohler line (Fig. 116.6). Type IIIB defects have superior migration greater than 3 cm, severe ischial lysis, and violation of Kohler line (Fig. 116.7) (12).
pelvic discontinuity. Type IIC defects are those that have distortion of the superior rim less than 3 cm of superolateral migration with medial migration past Kohler line (Fig. 116.6). Type IIIB defects have superior migration greater than 3 cm, severe ischial lysis, and violation of Kohler line (Fig. 116.7) (12).
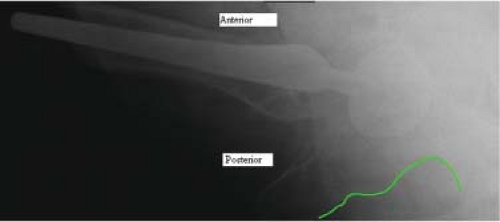 Figure 116.3. Shoot-through lateral of same patient from Fig. 116.2 again showing ischial lysis. Green line again representing posterior column. |
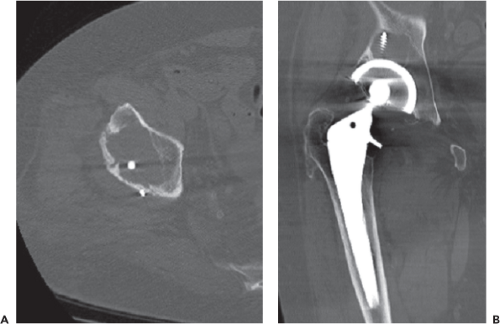 Figure 116.4. Computed tomography (CT) demonstrating severe osteolysis. A: Axial view. B: Coronal view. |
Berry et al. (1) subclassified the AAOS type IV defects into three categories: type IVa (pelvic discontinuity with
cavitary or moderate segmental bone loss), type IVb (severe segmental loss or combined segmental and massive cavitary bone loss), and type IVc (previously irradiated bone with or without cavitary or segmental bone loss).
cavitary or moderate segmental bone loss), type IVb (severe segmental loss or combined segmental and massive cavitary bone loss), and type IVc (previously irradiated bone with or without cavitary or segmental bone loss).
Intraoperative Evaluation
As stated above one needs to have a high clinical suspicion when reviewing plain films in the setting of an upcoming revision. However, pelvic discontinuity must be also ruled out at the time of any acetabular revision surgery. Failure to identify and address a pelvic discontinuity will result in the failure to obtain initial component stability and the subsequent lack of bone ingrowth. Intraoperatively, a pelvic discontinuity can be identified when motion is observed between the superior and inferior hemipelvis. Once the acetabular component has been removed, the inferior hemipelvis can be stressed with a Cobb elevator. If a pelvic discontinuity exists, the inferior hemipelvis will move independently of the superior hemipelvis.
Surgical Treatment Options
The principles of treating a pelvic discontinuity are no different than the approach to any hip revision surgery. The surgeon needs a stepwise approach to the revision: (1) identify the problem, (2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree