Fig. 7.1
Contact between the thumb and forearm during passive wrist flexion may indicate generalized ligamentous laxity
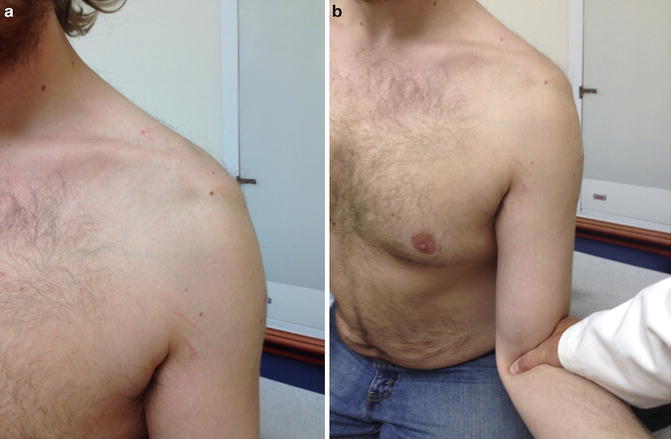
Fig. 7.2
(a) Sulcus sign. (b) Sulcus sign persisting in external rotation
Radiographic evaluation begins with plain radiographs. We routinely obtain internal and external rotation AP views, a scapular “Y” and an axillary view. Glenoid pathology may include bone loss, dysplasia with a shallow concavity, or abnormal version. The humeral head may have a posterolateral impaction fracture consistent with prior dislocations. Computed tomography is used to guide surgical planning or for diagnostic support when plain film bony detail is inadequate.
Magnetic resonance imaging or arthrography may be used to evaluate the glenohumeral soft tissue envelope. Its primary role is to rule out the presence of other pathology that may contribute to glenohumeral instability. Arthrography can distend the capsule and potentially improve visualization of the labrum, rotator interval, and capsular ligaments [26, 27]. While not diagnostic, a patulous glenohumeral capsule [5, 28, 29], increased glenohumeral volume, or labral pathology may be identified. Provencher and colleagues noted that rotator interval dimensions were the same in normal shoulders as well as those with anterior instability, posterior instability, or MDI [30]. Kim et al. did not study shoulders with MDI, but found increased rotator interval dimensions in patients with anterior instability [31]. Both investigators used MRA measurements to evaluate rotator interval widening as a pathologic feature of instability. However, Kuhn et al. did demonstrate that sectioning of the CHL increased external humeral rotation appreciably [32].
The evaluation of glenoid morphology in conjunction with the labrum should be taken into account. Relative glenoid hypoplasia or retroversion may contribute to posterior instability; in addition, the labrum contribution to version should be assessed. Chondrolabral retroversion can greatly contribute to posterior instability in the absence of bony deformity secondary to a blunted or atrophic posterior labrum [33].
Treatment Considerations
Glenohumeral instability occurs when the static and dynamic joint stabilizers cannot prevent symptomatic subluxation and/or dislocation. The objective of any rehabilitation, repair, or reconstruction is to impart sufficient stability to static and/or dynamic stabilizers to eliminate symptomatic subluxation and dislocation. The initial treatment of MDI patients is proprioceptive and strengthening physiotherapy. Rotator cuff strengthening and coordination may improve humeral head centering and compression while increasing resistance to subluxating shear forces. Scapulothoracic coordination may enhance glenoid positioning. Most investigators recommend a minimum of 6 months of physiotherapy before considering surgical management for symptomatic capsular laxity. When or if physical therapy fails, the majority of patients will respond favorably to arthroscopic capsular plication. It is imperative, however, that the patient is educated regarding the outcome of the procedure. A successful outcome typically results in a pain-free shoulder that has diminished range of motion or near normal when compared to the preoperative state. Patients that engage in overhead sports should be counseled that it may be difficult to continue that sport postoperatively due to loss of external rotation. Switching positions (for throwers) or modifying technique may be necessary in the absence of full cessation of overhead sports.
Rehabilitation
In their landmark study, Burkhead and Rockwood reported that muscle strengthening exercises yielded good or excellent results in 35 of 39 patients with MDI [34]. In contrast, Misamore et al. found that only 8 of 38 young athletic patients remained pain-free and instability-free after 8 years of follow-up [35]. There are also reports that shoulder kinematics and electromyographic function return to normalcy more closely in patients treated with capsular shift and physiotherapy when compared to physiotherapy alone [36, 37]. Despite these findings, the possibility of successful symptomatic management followed by a maintenance program remains attractive as it may obviate the need for surgical intervention.
Arthroscopic Techniques for Capsular Instability
Improvements in arthroscopic techniques and instrumentation have advanced arthroscopic procedures as the dominant modality to address MDI and capsular laxity. When compared with open treatment, arthroscopy offers the advantages of improved visualization and direct confirmation of capsular laxity or other glenohumeral pathology. There is decreased surgical morbidity as the subscapularis need not be compromised. Also, anterior and posterior pathology can be addressed through the same approach. Whether treatment is open or arthroscopic, an examination under anesthesia (EUA) is mandatory as a final preoperative assessment. The magnitudes and directions of glenohumeral translation are established. Cofield and colleagues reported 100 % sensitivity and 93 % specificity in diagnosing shoulder instability-based intraoperative EUA comparing the surgical and normal sides [38]. It should be noted, however, that other studies have demonstrated a consistent ability to subluxate the humeral head over the glenoid rim under anesthesia in patients without a diagnosis of instability [39]. It is paramount, therefore, that correlation to the patient’s history, examination findings both under and out of anesthesia, and imaging findings are used concurrently to arrive at an accurate diagnosis.
The earliest technique described for arthroscopic management of capsular instability was a glenoid-based inferior capsular shift, which was conceptually similar to the humerus-based open inferior shifts [40]. Capsular plication and capsulolabral augmentation (capsular plication which incorporates the labrum) were introduced later [41, 42]. The common threads of all surgical techniques for decreasing capsular instability are shortening and reinforcing the capsule while reducing capsular volume [2]. Several cadaveric models have sought to demonstrate changes in capsular volume with specific surgical techniques. Wiater and coworkers reported that progressive humerus-based open inferior capsular shifts decreased capsular volume in a linear fashion [43]. Lubowitz et al. also demonstrated decreased capsular volume with open inferior shift, but the amount of change varied when measured with MRI, ultrasound, and saline injection [44].
Several investigators have quantified capsular volume reduction in cadaveric models. Flanigan and coworkers reported that 10 mm of capsular plication decreased capsular volume by 33.7 % [45]. Volume can be reduced incrementally with sequential plications. Karas and colleagues found that four capsulolabral plications from 4 to 8 o’clock decreased capsular volume 19 % [46]. Incremental capsular plication has also been shown to reduce capsular volume but in a nonlinear fashion [47]. After 4 cm of total plication, additional plication becomes less effective. Volume reduction was not affected by the use of suture anchors or suture alone [47]. Suture anchor-based capsular plication has been demonstrated to reduce capsular volume at least as well as traditional open capsular shift techniques in cadavers [48].
Capsulolabral augmentation involves incorporating intact labrum into the plication. It has analogous effects on the capsule, but is also hypothesized to enhance stability via increased glenoid depth and labral width. Cadaveric models demonstrate decreased humeral head displacement following capsulolabral augmentation [41].
Inferior Shift
Arthroscopic glenoid-based inferior capsular shifts secured to the glenoid via a bone anchor have been described by several authors [40, 49]. In one series of 25 patients, 3 had recurrent instability at an average 5-year follow-up [40, 49]. Fleega and El Shewey described an arthroscopic inferior shift technique for isolated anteroinferior capsular instability with lower recurrence [50]. At a minimum of 7 years follow-up, 3 of the 75 patients had dislocations after significant trauma.
Capsular Plication and Capsulolabral Augmentation
Successful capsular plication for patients with multidirectional instability and capsular redundancy has been reported by Wichman [42], and Whitehurst [51]. Gartsman and colleagues described a similar technique, but his patients did not have isolated capsular instability [52]. In 47 shoulders, 28 labral tears requiring repair were identified. When treating traumatic or atraumatic instability in two directions in the absence of structural lesions, arthroscopic capsular plication and open capsular shift have comparable recurrent instability, return to sport, loss of external rotation, and complications [53].
Baker et al. described an approach for young athletic patients, where each direction of instability was addressed sequentially. Shoulders with isolated patulous capsules received capsulolabral plication with or without suture anchors. All patients with labral tears received a capsulolabral plication with suture anchors. Two patients had failures based on low ASES score (American Shoulder and Elbow Surgeons standardized shoulder assessment score). Two more had failures based on WOSI scores (University of Western Ontario shoulder instability index percentage) [54]. It is not clear if the failures had isolated capsular or capsulolabral pathology.
Ma and colleagues reported on 23 overhead athletes with multidirectional instability and isolated capsular laxity who were treated with pan-capsular plication and interval closure. At a minimum 2-year follow-up, all patients were satisfied with stability, but only five returned to the same level of competitive sport [28].
Capsulolabral augmentation with suture anchors has been shown to be at least as strong and as stiff as using suture alone [55, 56]. While capsulolabral repair is distinct from capsulolabral augmentation, many of the repair techniques, like the multiple pleated plication method [57], can easily be adapted for augmentation.
Interval Closure
Since Harryman and colleagues demonstrated that imbrication of the rotator interval capsule increased resistance to posterior and inferior humeral translation in an open surgery cadaveric model [58], investigators have debated the clinical importance of interval closure in glenohumeral instability. An arthroscopic cadaveric model suggested that interval closure reduces anterior humeral translation and external rotation at 90° of abduction [59], but the impact on stability in other directions is unclear. Furthermore, the preponderance of arthroscopic studies employs a “north-south” interval closure which does not mimic the “east-west” course of the CHL. Gartsman recommended interval closure if laxity remained after arthroscopic capsular shift [52]. Several arthroscopic techniques for interval closure have been described [60–63]. Almazan and coworkers suggested that interval closure may address laxity created by the placement of arthroscopic cannulas during capsular plication or labral repair surgery [60]. While no clear clinical benefit has been demonstrated, some investigators believe interval closure may be appropriate when capsular plication does not produce adequate stability in MDI patients [28, 54]. Similar to plication, interval closure can result in loss of external rotation [59]. The closure should be tensioned with the humerus in 30° of external rotation to minimize loss of motion.
Thermal Capsulorrhaphy
Thermal capsulorrhaphy offered the possibility of speed, simplicity, and direct visual assessment of capsular shrinkage. Early reports suggested that it was viable alternative to capsular shift techniques [29, 64], but long-term results were plagued by chondrolysis, thermal nerve injury, and high rates of recurrent instability [65–68]. We mention this technique for historical completeness, but it is not recommended for the treatment of MDI.
Author’s Preferred Technique
A preoperative interscalene anesthetic block is used for analgesia and muscle relaxation. In addition, we use general endotracheal anesthesia for definitive airway control because patients are placed in the lateral decubitus position. The lateral decubitus position affords greatly enhanced access to the inferior and posterior joint recesses.
We employ a systemic sequential approach , similar to that described by Bradley [54]. All patients receive an EUA, and directions and magnitudes of humeral head translation are recorded. We prefer the lateral decubitus position with an upper extremity traction boom for glenohumeral instability procedures. Lateral decubitus position is maintained with a bean bag. An axillary roll is placed to improve thoracic excursion and to relieve pressure on the brachial plexus and axillary neurovascular structures. All nonoperative extremities are padded to protect bony prominences and superficial nerves. The traction boom is attached anterior to the patient at the foot of the operating table. The arm covered with a stockinette that has a distal strap to connect with the traction boom. We usually apply 15 lbs of in-line traction. The shoulder is placed in slight flexion (20–30°) and abduction (45°), which helps to open the posterior capsule and axillary recess respectively (Fig. 7.3). Diagnostic arthroscopy identifies redundant capsule, labral abnormalities, and any other intra-articular pathology. For the majority of patients, a balanced plication is in order. The shoulder joint appearance also lends clues to principal directions of instability. Labral fraying, fissuring, and chondral changes of the glenoid and humerus indicate directions of increased translations. In essence, a surgical goal is to effect a balanced plication with the humeral head resting in a neutral position with traction released. Based on the degree of sulcus sign, the rotator interval is closed in a medial to lateral direction (to effectively shorten the CHL) if the sulcus sign does not diminish with external rotation. Prior to plication, the IGHL, posterior band of the IGHL, and capsule are gently debrided with an arthroscopic rasp to promote healing. Plication begins in the direction of the largest translation. Gerber et al. have demonstrated predictable patterns of motion decrease with selective glenohumeral capsule plication in cadavers [69]. We typically begin inferior and work superior, since each plication decreases capsular volume and working space. This avoids the inconvenience of working in the distant inferior pouch through a narrow superior glenohumeral interval. We prefer to secure the capsular plication with suture anchors to prevent loosening of the plication in patients who may not be as compliant postoperatively. If possible, two working portals are usually established for the arthroscopic technique. The less puncture holes that are placed in the glenohumeral joint capsule for working, the better able we are to restore capsular stability. The anterior portal and 7 mm cannula are placed in the rotator interval, while the posterior portal and cannula are placed in line with the lateral edge of the acromion at the level of the posterior “soft spot ” to facilitate anchor placement along the posterior glenoid rim.


Fig. 7.3
Lateral decubitus position with traction boom placed anteriorly at the foot of the operating table. Shoulder is abducted 45° and forward flexed 20°. The posterior superior shoulder is visible and the surface anatomy has been marked
The labrum is only gently debrided and single-threaded anchors (typically size 2.3 mm) are placed along the glenoid margin with nonabsorbable #2 suture. The sutures are shuttled through the capsule and labrum using a suture hook shuttle device and tied down individually after passage (Fig. 7.4). Each suture limb can be passed multiple times for a pleated plication to titrate the repair based on the degree of laxity as described by Sekiya (45°). After each stage of plication is complete, a repeat EUA is performed to confirm adequate stability in the treated direction and to determine the direction of maximum residual stability. For patients with primarily posterior and global laxity, the posterior portal is closed using standard suture passage techniques with the cannula backed just beyond the capsule. For those patients with significant rotator interval laxity (as described prior), the rotator interval portal is closed instead. The goal of capsular plication is to restore glenohumeral alignment and prevent subluxation of the humeral head beyond the glenoid margin. This must be confirmed before completing the procedure. Aggressive plication can result in a preferential loss of external rotation.
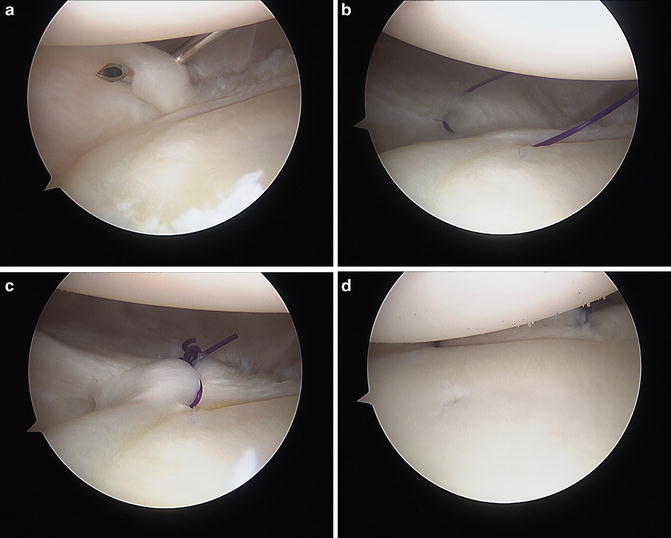
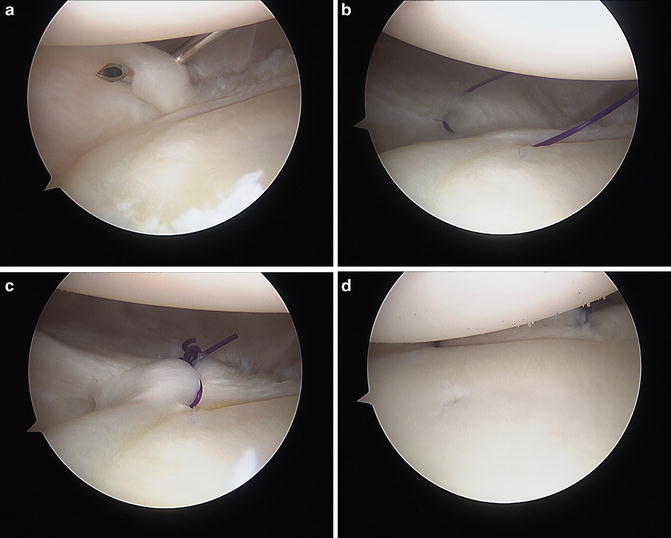
Fig. 7.4
(a) Suture hook through inferior glenohumeral ligament. (b) PDS plication stitch through inferior glenohumeral ligament and labrum. (c) Capsulolabral plication. (d) Two anterior capsulolabral plication sutures with humeral head reduced to glenoid fossa
Postoperative Management
The rehabilitation protocol following arthroscopic management of MDI must be tailored to the directions of instability and the quality of the stabilization procedure. Following stabilization, we routinely place patients in an abduction sling for 4 weeks. Pendulum exercises are begun at 2 weeks along with active wrist and elbow motion. A passive range of motion protocol is initiated at 4 weeks and continued until near full range of motion is achieved. Active-assisted range of motion is initiated at 6 weeks, and full active motion of the shoulder is advanced by 6–8 weeks. Gentle strengthening begins at 10 weeks or when 80 % of range of motion has been attained. For athletes, sport-specific training begins at 4 months. We restrict full participation in sports until nearly 80 % of strength has been achieved with near-normal glenohumeral range of motion.
Complications
Recurrent instability following arthroscopic management of capsular instability has been reported to be 0–21 % [28, 42, 49, 53, 54, 70]. These studies are challenging to interpret as they include some patients with unidirectional capsular instability [42] and labral lesions requiring repair [54]. The surgical techniques also vary. Treacy and colleagues [49] described a glenoid-based inferior shift secured through a transglenoid tunnel, while Hewitt et al. [70] and Ma et al. [28] used a capsular plication secured around the labrum with suture only. Treacy [49] and Ma [28] routinely closed the rotator interval, while Hewitt [70] reserved closure for patients with a persistent sulcus following stabilization. Treacy [49] reported 2 failures of 11 patients with 60 months follow-up. Hewitt [70] had 3 recurrent instabilities in 30 shoulders with follow-up of 57 months. Ma’s [28] series reported that they did not have recurrent instability in 23 patients with 36 months of follow-up. Of these five collective episodes of recurrent instability, four were traumatic and one patient had previous surgery. While these are not large samples, the data suggest that trauma is the major risk factor for recurrent instability.
Ma et al. did not find any difference in pre- and postoperative external rotation following arthroscopic stabilization with capsulolabral augmentation and interval closure in athletes [28]. However, the group of patient who returned to sport averaged 10° more of preoperative external rotation. This difference was not compared statistically. Treacy and colleagues [49] reported that no patients lost external rotation. Hewitt [70] found a mean loss of 8.5°.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








