Management of Bony Insufficiency of the Glenoid and Humerus with Arthroplasty
Julie Y. Bishop
Evan L. Flatow
J. Y. Bishop: Clinical Shoulder Fellow, Department of Orthopaedic Surgery, Mount Sinai Medical Center, New York, New York.
E. L. Flatow: Lasker Professor of Orthopaedic Surgery, Chief of Shoulder Surgery, Department of Orthopaedic Surgery, Mount Sinai Medical Center, New York, New York.
INTRODUCTION
Unconstrained shoulder arthroplasty has become a commonly performed procedure for many acute and chronic shoulder disease processes. Its success has been well established and largely depends on the status of the soft tissues, especially the rotator cuff and deltoid. However, the bone stock available for implant fixation is also of great importance. In the primary shoulder arthroplasty, glenoid bone loss is more often a problem than humeral loss. Patients with severe osteoarthritis may have significant posterior glenoid erosion, and the rheumatoid patient may have an eroded or medialized glenoid. Dramatic glenoid or humeral bone loss may be encountered during revision shoulder arthroplasty and with reconstruction after en bloc resection of bone for tumors of the shoulder girdle, especially in relation to the proximal humerus. In the revision situation, glenoid loosening is more common than humeral loosening and overall has been found to be the most common long-term complication of total shoulder replacement.2,5,6,7,11,17,36,49,51
Concern for glenoid component survival has prompted many to consider humeral replacement without glenoid resurfacing (“hemiarthroplasty”) for glenohumeral arthritis, especially in cases in which poor glenoid bone stock would make glenoid resurfacing difficult. However, recent studies, including randomized prospective trials comparing humeral head replacement with the nonconstrained total shoulder replacement, have reported better pain control and function in patients undergoing total shoulder arthroplasty.21,36,39 Thus, the reconstructive shoulder surgeon requires strategies to deal with the difficulties of bony deficiency in the primary arthroplasty setting, as well as in the revision situation.18,48,50,51,53
PATTERNS OF BONY LOSS
Preoperative evaluation for patients undergoing total shoulder arthroplasty consists of the standard medical history, preoperative examinations, and radiographic imaging. Although the radiographic and intraoperative evaluations are the key to assessing glenoid deficiency, certain clues as to glenoid bone stock may come from the history
and examination. The patient’s diagnosis, in particular, may provide the most insight into the type of potential bone loss that may be present.
and examination. The patient’s diagnosis, in particular, may provide the most insight into the type of potential bone loss that may be present.
Osteoarthritis
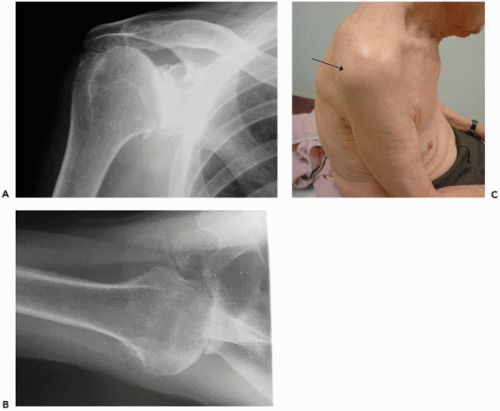
Some conditions are less likely to lead to glenoid bone erosion such as posttraumatic arthritis or avascular necrosis. In contrast, osteoarthritis or secondary arthritis resulting from previous instability repair are prone to posterior glenoid erosion (Fig. 27-1). In these patients, the case is often complicated with an instability pattern. This is classically described in patients undergoing previous stabilization procedures who have posterior subluxation because of an overly tightened anterior capsule and, thus, the subsequent posterior glenoid erosion (Fig. 27-2). In patients with primary osteoarthritis, the shoulder is usually stiff and not “unstable” in the sense of having uncontrolled translations, but they have stiff anterior tissues, a fixed posterior humeral subluxation, eccentric posterior glenoid wear, and a large posterior capsule. Therefore, in these patients, not only must the bony loss be addressed, but, to avoid recurrent posterior subluxations and an overall failure, the soft tissues must be balanced3,56 and the glenoid not implanted in retroversion.
Rheumatoid Arthritis
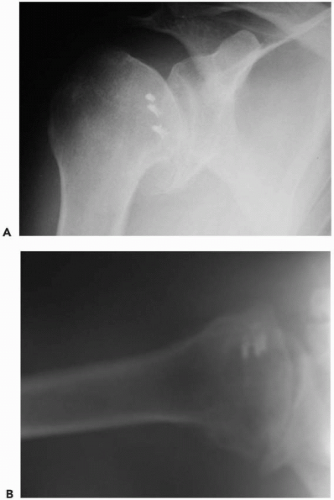
The pathology seen in shoulders with rheumatoid arthritis varies from mild to very severe.65 Neer47 classified the pattern of rheumatoid involvement in the shoulder as dry, wet, or resorptive, with the possibility of low-grade, intermediate, or severe changes within each group. With the dry form, there is a tendency for joint space loss, periarticular sclerosis, bone cysts, and stiffness. In the wet form, there is abundant synovial disease with marginal erosions and protrusion of the humeral head into the glenoid. The characteristic feature of the resorptive form is bony resorption. Thus, commonly, the patients with rheumatoid arthritis or other inflammatory arthritides often develop severe medialization of the glenoid with central erosions (Fig. 27-3). The bone quality is often osteopenic to varying
degrees, further complicating the bony loss. Many rheumatoid patients may have rotator cuff disease and cuff loss, which may contribute to the pattern of arthritis. They may present with a pattern more like a cuff-tear arthropathy, in which there is more superior bone loss as the head articulates with an “acetabularized” coracoacromial arch, coracoid bone, superior glenoid, and acromioclavicular joint. All of these factors make the management of bony loss in the patient with long-standing rheumatoid arthritis especially challenging.
degrees, further complicating the bony loss. Many rheumatoid patients may have rotator cuff disease and cuff loss, which may contribute to the pattern of arthritis. They may present with a pattern more like a cuff-tear arthropathy, in which there is more superior bone loss as the head articulates with an “acetabularized” coracoacromial arch, coracoid bone, superior glenoid, and acromioclavicular joint. All of these factors make the management of bony loss in the patient with long-standing rheumatoid arthritis especially challenging.
Bone Loss in Revision Surgery
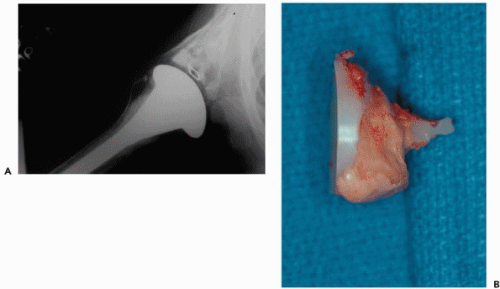
When undertaking a revision total shoulder arthroplasty, the surgeon will often encounter bony defects in either the humerus or glenoid. Bone lesions of the glenoid may simply be classified according to their composition (contained, uncontained, or combined) and location (peripheral or central). Contained defects involve the loss of cancellous bone within the glenoid vault, whereas noncontained defects involve some loss of cortical support usually along the posterior rim of the glenoid (i.e., posterior glenoid erosion). Glenoids with contained defects have historically been treated by filling the smaller defects with cement and larger
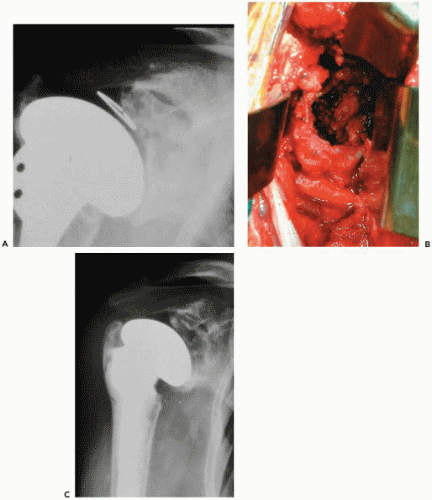
defects with bone graft. Cancellous bone grafting has been recommended for focal bone loss more than 3 mm in size.53 Overall, the contained defects are somewhat easier to address in the revision situation. Noncontained defects and huge cavitary lesions can be the most devastating to encounter in a revision. For a noncontained deficit, such as posterior wear, early attempts using an uneven cement mantle to correct glenoid version led to an increased rate of component breakage and loosening (Fig. 27-4).12,51,59 More recent efforts have focused on eccentric reaming in an attempt to correct mild glenoid erosion; however, severe glenoid deficiency may require grafting (which will be discussed in detail later in the chapter). Finally, when the glenoid deficiency cannot be corrected with bone grafting, especially when there is medialization of the glenoid, resurfacing of the glenoid may need to be abandoned (Fig. 27-5).
defects with bone graft. Cancellous bone grafting has been recommended for focal bone loss more than 3 mm in size.53 Overall, the contained defects are somewhat easier to address in the revision situation. Noncontained defects and huge cavitary lesions can be the most devastating to encounter in a revision. For a noncontained deficit, such as posterior wear, early attempts using an uneven cement mantle to correct glenoid version led to an increased rate of component breakage and loosening (Fig. 27-4).12,51,59 More recent efforts have focused on eccentric reaming in an attempt to correct mild glenoid erosion; however, severe glenoid deficiency may require grafting (which will be discussed in detail later in the chapter). Finally, when the glenoid deficiency cannot be corrected with bone grafting, especially when there is medialization of the glenoid, resurfacing of the glenoid may need to be abandoned (Fig. 27-5).
Humeral defects encountered in the revision situation are typically found in either the proximal metaphyseal region or distally in the cortical region. Minimal to moderate metaphyseal deficiencies can be discrete bony defects, or at times large losses of metaphyseal bone can be present. The diaphysis can have large and sometimes isolated defects. Defects present after resection for neoplasm are mostly large, segmental losses of bone.
Bone Loss Encountered in Fracture/Tumor Surgery
A traumatic injury to the shoulder can result in certain fracture patterns that can lead to bone loss in either the glenoid or humerus. Severe glenoid crush fractures can lead to a special pattern of bone loss, specific to the type of fracture. Severely comminuted proximal humerus fractures may have significant bone loss at presentation. Hemiarthroplasty for these situations has achieved widespread acceptance.14,46,48,50,52,63 Although there are many technical aspects to this treatment alternative, one of the most challenging is reestablishing the proper height of the prosthesis, especially when severe comminution or bone loss at the surgical neck exists. This problem is even more difficult in the revision setting, in which a prosthesis was placed too low, leading to poor function or instability.8,50,69 Neer and Kirby50 found this problem to be common after reconstruction for fractures in which there had been loss of humeral bone. Of 27 failed arthroplasties for fractures in their study, 18 had instability of the prosthesis and inadequate deltoid power because more than 2 cm of humeral length had been lost (58-book). If there is difficulty securing the tuberosities, either because of tuberosity bone loss or loss of bone at the shaft precluding adequate fixation, then tuberosity fixation should be supplemented with generous cancellous bone graft.
Tumors of the shoulder girdle can lead to significant glenoid or humeral loss after resection. The challenge of shoulder reconstruction after removal of a segmental portion of bone for neoplasm is immense. The proximal humerus is the second most common site of long bone primary tumors9; however, metastatic lesions of the shoulder girdle are common as well. After an appropriate amount of resection has been performed to maximize disease eradication, the generally accepted options for skeletal reconstruction of the proximal humerus include four techniques:
arthrodesis, all-metal prosthesis, osteoarticular allograft, or allograft-composite.
arthrodesis, all-metal prosthesis, osteoarticular allograft, or allograft-composite.
IMAGING
The diagnosis of bony deficiency of the arthritic shoulder is made with a proper radiographic evaluation. Imaging techniques, including plain radiographs, computed tomography (CT) scans, and possibly magnetic resonance imaging (MRI), truly remain the cornerstone of preoperative planning, whether for the primary arthroplasty or revision situation. Proper evaluation and subsequent anticipation of the magnitude of bony loss will help prepare the surgeon to deal with any situation that arises at the time of reconstruction.
Radiographs
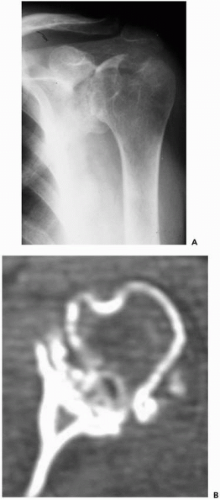
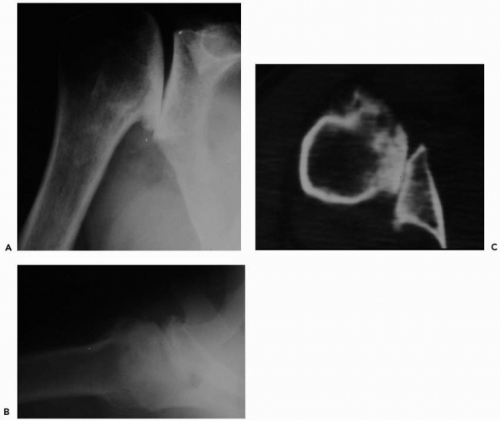
The radiographic series should consist of a true “scapular” anteroposterior (AP) view, a lateral “Y” scapular view, and an axillary view (Fig. 27-6, A and B). The axillary view is best for evaluating the amount of posterior wear, which is common in osteoarthritis or in patients who have undergone stabilization procedures. However, the axillary view can sometimes be inaccurate, and superimposition of the superior and inferior glenoid can make assessment of the glenoid vault difficult. If possible, serial radiographs including preoperative and postoperative x-rays (in the revision cases) should be assessed for radiolucent lines, osteolysis, prosthetic position, and prosthetic migration. If glenoid or humeral loosening is suspected, fluoroscopically guided radiographs may aid in demonstrating radiolucent lines at the bone-cement interface.11,35 Fluoroscopy also has been recommended as useful in evaluation of glenoid wear, as opposed to CT, which more commonly is used to assess the extent of glenoid damage.19,43,57
Computed Tomography Scan
Although a CT scan is not an absolute necessity in every case, the narrow-cut (3-mm) cross-section imaging can provide important information about the implant positioning, humeral and glenoid bony loss, glenoid version, and posterior glenoid erosion (Fig. 27-6C).20,25 Axillary radiographs can be inaccurate especially as to glenoid version, and CT is very useful in assessment of the available glenoid bone stock. It is important to fully examine the lower, middle, and upper glenoid cuts for a full understanding of the glenoid vault. The normal glenoid version has been shown by transverse CT studies to be approximately 6 degrees retroverted in relation to the angle between the glenoid fossa and the scapular blade.43 This information can be useful in the preoperative assessment of glenoid deficiency and bone stock available for reconstruction, especially when there is difficulty in attaining a good axillary view. Magnetic resonance imaging is rarely necessary in the evaluation of bony deficiencies for a primary or revision
surgery. However, if the status of the rotator cuff is in question, MRI can be used; however, it will provide less detail about the condition of the bone. Good MRIs can be obtained in the face of a prosthesis, and good information can be obtained when special techniques to reduce metal artifact are used.30
surgery. However, if the status of the rotator cuff is in question, MRI can be used; however, it will provide less detail about the condition of the bone. Good MRIs can be obtained in the face of a prosthesis, and good information can be obtained when special techniques to reduce metal artifact are used.30
GLENOID BONE LOSS: TECHNIQUES
Successful implantation of a glenoid component during a primary or revision total shoulder arthroplasty requires adequate exposure, appropriate soft-tissue balancing, careful glenoid preparation, and meticulous implant techniques. In the face of glenoid bone loss, an adequate assessment of the deficiency can only truly be performed if there is sufficient exposure of the glenoid. Although preoperative history and radiographic assessment are extremely important, the final evaluation of the extent of glenoid bony deficiency is achieved after direct inspection and palpation in the operating room. Of course, this will only be possible if the surgeon has performed the necessary releases and exposed the glenoid properly (Fig. 27-7).
Exposure and Releases
A standard deltopectoral approach is used extending proximally from the anterior edge of the clavicle just lateral to the coracoid and distal to the anterior deltoid insertion. Although it is technically possible to use a smaller incision, in this patient population scar length is usually not a concern and can limit the ease of exposure. Because resurfacing of the glenoid demands adequate exposure, especially when bony deficiency is present, an extensile deltopectoral approach is warranted. Any previous incisions are incorporated if possible.
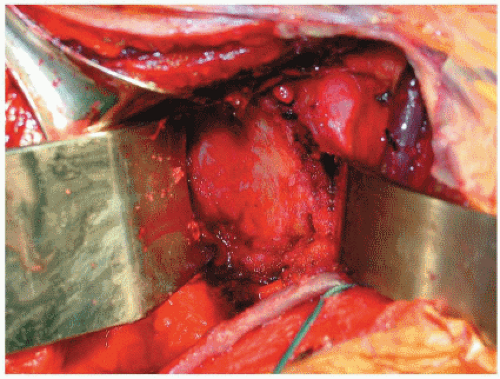 Figure 27-7 Exposure of the glenoid. The glenoid should be visualized en face, which requires extensive releases, especially in the revision situation. Although difficult, adequate evaluation of the extent of bony losses is only possible after full exposure. A Fukuda retractor is placed behind the posterior glenoid rim, and a spiked, curved retractor is used to expose the anterior glenoid margin.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|