Nonoperative Management of Adult Flatfoot Deformities
Roger Marzano, CPO, Cpedrmarzano@yankebionics.com, Yanke Bionics Clinics, Inc, 303 West Exchange Street, Akron, OH 44302, USA
Managing those with adult flatfoot deformities can be quite challenging, and the methods and devices used are wide-ranging based on the experience of the managing physician and the experience of the provider of the orthotic devices. A thorough biomechanical assessment is paramount to provide the most successful treatment due to the wide range of pathologic abnormalities and pathomechanics that lead to this painful disorder. Taking away pain while improving function for any patient is a rewarding aspect of clinical foot care, and the information covered in this article should arm the practitioner, or surgeon, with viable alternatives to surgical management.
Pathomechanics and biomechanical assessment
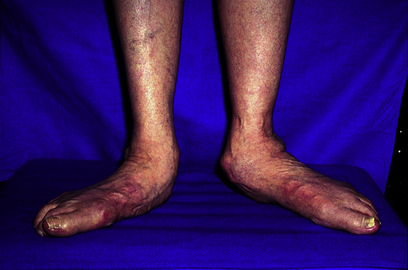
The most common alignment deficiencies seen in those with adult flatfoot deformity are forefoot varus, hypermobility of the first ray, and a congenitally or iatrogenically shortened first ray, which often presents with transfer metatarsalgia. Other alignment deviations commonly seen in this patient population are excessive calcaneal valgus with resultant subfibular impingement, peritalar subluxation, and equinus contractures noted in most (Fig. 1). In late stage II and stage III tibialis posterior tendon dysfunction patients, one may see stress fractures of the distal fibula and lateral column symptoms due to the compressive forces to the lateral articular structures of the hindfoot. Other concomitant pathologic abnormalities commonly managed with these patients are hallux limitus or rigidus, tibialis posterior tendinosis or rupture, tarsal coalition, accessory navicular, midfoot osteoarthrosis, Charcot osteoarthropathy, and even some failed or nonunions of single, double, or triple arthrodeses. Patients who have had previous ankle arthrodeses or malaligned arthrodeses will often, over time, develop a secondary flatfoot deformity due to the subtalar and midtarsal articulations becoming mobile in dorsiflexion to compensate for the loss of talocrural mobility created by the ankle fusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree