Magnetic Resonance Imaging in the Lower Extremity
Courtney T. Tripp
John F. Feller
The opinions and assertions expressed herein are those of the authors and should not be construed as reflecting those of the Department of Defense.
HIP
Hip magnetic resonance imaging (MRI) protocols in the athlete should be performed to optimize assessment for both internal and external derangements of the hip. Ideally, MRI evaluation includes a combination of large field-of-view bilateral hip and pelvic structures that aid in evaluation of extra-articular abnormalities (i.e., musculotendinous injuries, osseous injuries, bursitis) and high-resolution small field-of-view unilateral imaging for intra-articular abnormalities (e.g., articular cartilage and acetabular labrum injuries, femoral acetabular impingement [FAI], and loose bodies) (5).
Although controversy exists regarding the most appropriate MRI assessment of intra-articular hip pathology, multiple studies have shown a high degree of accuracy with both noncontrast MRI and magnetic resonance (MR) arthrography for diagnosis of cartilage injuries of the hip (12,18,25). Newer novel MR mapping techniques for chondral assessment are also being developed (24).
Intra-articular abnormalities that commonly affect the young athletic population and can be evaluated with MRI include acetabular labral tears, chondral injuries, intra-articular loose bodies, and FAI.
Acetabular labral tears are well evaluated with MRI and diagnosed as a linear hyperintense signal contacting the labral surface either at the labral-acetabular junction or in the labrum itself (5).
Osteochondral injuries of the hip may be due to impaction injury, hip dislocation, or subclinical chondral shearing, and most commonly are present in the superomedial femoral head. Moderate to moderately high sensitivity for detection of chondral lesions of the hips has been reported. Cartilage sensitive sequences, especially high-resolution intermediate-weighted sequences, are necessary for optimal evaluation of chondral injuries (12,31). Intra-articular loose bodies can be identified on MRI and are especially conspicuous in the presence of a joint effusion or arthrographic solution.
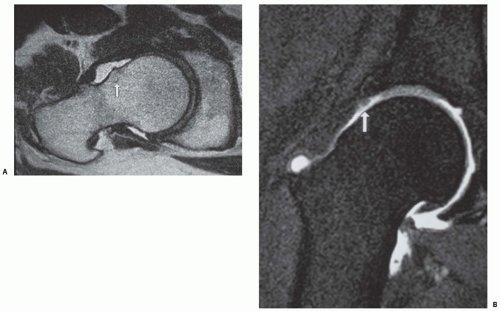
FAI is increasingly recognized as a potential cause of early-onset osteoarthritis of the hip. This impingement essentially is due to reduced joint clearance with repetitive abutment between the femur and acetabular rim during terminal hip movement. Findings on MRI that are suggestive of the clinical syndrome of FAI include labral tears, especially at the labral-chondral transition zone, and loss of articular cartilage. A nonspherical shape of the femoral head with decreased femoral head offset and anterosuperior chondral loss is characteristic of camshaft (Cam)-type FAI, whereas acetabular overcoverage and posteroinferior acetabular chondral loss characterize pincer-type FAI (Fig. 58.1) (14,23).
MRI is useful in imaging of the extra-articular regional musculotendinous structures demonstrating injuries such as traumatic muscular contusions or strains, tendinopathy, and tendon tears. Common to the athlete are musculotendinous strains of the hamstring and rectus femoris muscles, with abnormal high signal within the muscle and/or tendon on MRI. In adductor avulsion syndrome (“thigh splints”), there is periosteal hyperintensity near the insertion of the adductor muscles of the femur (3). Tendinosis, which is seen as thickening and or hyperintensity of the tendon, is commonly seen within the gluteus medius and minimus tendons near their greater trochanteric insertions.
The term athletic pubalgia (“sports hernia”) has been applied to various causes of lower abdominal wall and peripubic pain. A recent study by Zoga et al. (36) found a high correlation of clinical symptoms with MRI findings of rectus abdominis and adductor tendon insertional injuries at their pubic bone insertion.
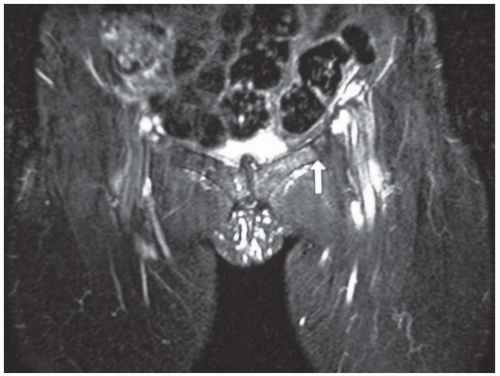
MRI evaluation of the osseous structures of the hip is excellent and is the imaging modality of choice for osseous stress injuries, avascular necrosis (AVN), and occult fractures. Osseous stress reaction and stress fractures common to the athletic population involve the femoral neck, the pubic bones, and the sacrum, all of which demonstrate marrow edema, and in the case of stress fracture, a low signal intensity line (Fig. 58.2).
AVN and subchondral insufficiency fractures of the femoral head both demonstrate femoral head edema in early stages.
Findings of AVN include a “double line sign” in nearly 80% of cases and may progress to include a subchondral fracture line and eventual articular collapse.
There are a few bursae in the region of the hip, notably the greater trochanteric, iliopsoas, and ischial bursa, which may become inflamed by repetitive microtrauma, demonstrating fluid signal hyperintensity of the bursa on MRI.
KNEE
MRI evaluation of the knee should include triplanar imaging with both high-resolution, intermediate-weighted, cartilage-sensitive sequences and water-sensitive (intermediate/T2 fat-suppressed, or STIR [short tau inversion recovery]) sequences for evaluation of marrow edema and pathology of the soft tissues.
In the athletic population, accurate evaluation of cartilage injury is crucial for directing treatment. MRI has been demonstrated to be an accurate method for evaluation of articular cartilage injuries. For this purpose, high-resolution cartilage-sensitive pulse sequences should be used in routine MRI of the knee. Generally, normal cartilage should be intermediate in signal intensity and of rather uniform thickness. With high-resolution cartilage-sensitive sequences, however, a normal gray scale stratification of the cartilage may be seen, which corresponds to normal cartilage zonal anatomy (31).
MRI accuracy for diagnosis of internal derangement of the knee is excellent, with high sensitivity and specificity (9,16). It is the most commonly evaluated joint by MRI (29). In a study of 200 patients who had MRI of the knee and subsequent arthroscopy, Vincken et al. (34) demonstrated high sensitivity and specificity of MRI for diagnosis of both medial and lateral meniscal tears, concluding that MRI is effective as a test for directing clinical treatment.
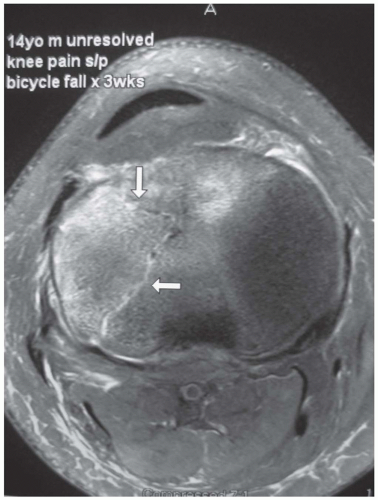
Figure 58.3: Axial fat suppression intermediate-weighted MRI demonstrating a subacute nondisplaced occult tibial plateau fracture (arrows), which was not suspected clinically.
MRI has a high sensitivity for diagnosing bone marrow edema, the causes of which are varied and include trauma, AVN, subchondral stress reaction or insufficiency fractures due to altered biomechanics, or arthritic changes (Fig. 58.3).
Many injury patterns are encountered in sports injuries to the knee, and certain bone marrow contusion patterns seen at MRI correlate with particular mechanisms of injury. Sanders et al. (29) described 5 such patterns that have a high correlation with specific soft tissue injuries of the knee. One particularly common contusion pattern is the “pivot shift injury,” in which the classic bone marrow edema pattern involves the posterolateral tibial plateau and the midportion of the lateral femoral condyle. The anterior cruciate ligament (ACL) is invariably torn with this mechanism of injury. Other soft tissue injuries to the knee that can be seen in this pattern include medial collateral ligament sprains, longitudinal tears through the peripheral aspect of the posterior menisci, and posterior capsular injuries (29).
The normal ligamentous and tendinous structures of the knee have uniformly low signal intensity on all MRI sequences. The cruciate ligaments are best seen on sagittal sequences, and the collateral ligaments are best seen on coronal sequences. However, correlation with orthogonal imaging planes is often valuable in corroborating pathology because, occasionally, volume averaging of signal with adjacent soft tissue structures may falsely suggest pathology (27).
The ACL is commonly injured in athletes. On MRI, the ACL is a thick dark band-like structure that parallels the roof of the intercondylar notch. Direct MR signs of ACL disruption include focal discontinuity of ligament fibers, abnormal slope of the ACL, and avulsion of the anterior tibial spine (Fig. 58.4).
Additional indirect MR signs of ACL disruption that can increase confidence of an ACL tear include a deep sulcus sign, a Segond fracture (capsular avulsion fracture of lateral tibial plateau), anterior translation of the tibia relative to the femur, hyperextension bone contusion injuries involving the anterior tibia and femur, and buckling of the posterior cruciate ligament (PCL) (28).
Full-thickness ACL tears are diagnosed by observation of complete discontinuity of the ligament fibers, as described previously. Partial-thickness ACL tears can be difficult to diagnose because there is only partial ligament fiber discontinuity. Confirmation of the diagnosis of partial ACL tear not only in the sagittal but also in the axial plane may be necessary (27). In the athletic population, ACL tears are typically repaired, because an unrepaired torn ACL may subsequently lead to chronic ACL deficiency. This condition is associated with a higher risk of medial meniscal degenerative tearing.
The ACL can be evaluated postoperatively with MRI and should parallel the roof of the intercondylar notch, without buckling, as seen in the sagittal plane. Tears of ACL grafts are diagnosed by observing focal discontinuity of graft fibers, not unlike that seen in a native ACL tear. Postoperatively, fast spin echo and inversion recovery sequences should be used rather than frequency selective fat suppression as the
water-sensitive sequence, because the latter is more susceptible to metallic particle-associated magnetic field inhomogeneities resulting in susceptibility artifact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree