Lunotriquetral Dissociation
18.1 Introduction
Historically, the etiology and treatment of carpal instability located on the radial side of the wrist has received the greatest attention. Although Linscheid et al in their landmark paper had already described ulnar-sided instability in the 1970s, lunotriquetral (LT) disruption as a specific carpal injury was described by Reagan et al only in 1984.1 Lunotriquetral dissociation is a common form of carpal instability on the ulnar side of the wrist, but the general awareness of this problem is often poor, which explains why currently the diagnosis of lunotriquetral injuries is still delayed or missed. It may occur not only as an acute isolated lesion but also as part of a more complex injury. On the other hand, as a more chronic lesion, it may be associated with degenerative tears of the triangular fibrocartilage complex (TFCC) or be secondary to ulnocarpal abutment syndrome. The clinical appearance may range from a dynamic type of instability to a static and fixed carpal instability. Often it is confused with other ulnar-sided wrist problems, such as midcarpal instability, incomplete lunotriquetral coalition, lesions of the TFCC , isolated triquetrohamate instability, pisotriquetral problems, extensor carpi ulnaris instability or tendinitis, or distal radioulnar joint subluxation.
18.2 Anatomy
Because the three bones of the proximal carpal row have no tendinous insertions and therefore no dynamic constraints, normal kinematics and joint stability are dependent on the joint surface configuration as well as on intrinsic and extrinsic ligaments.
The triquetrum is regarded as the keystone in the coordination of motions occurring at four articulations.
The LT joint forms the articulation between the ulnar surface of the lunate and the radial surface of the triquetrum. These articulations between the lunate and triquetrum are flat and semilunar.
The convex proximal surfaces of the lunate and triquetrum articulate with the hybrid radiocarpal/ulnocarpal articulation: the lunate fossa of the distal radius and the triangular disk of the TFCC. Usually, no more than 50% of the lunate articulates with the triangular disk.
The relevant midcarpal articulation is between the distal articular surfaces of the lunate and triquetrum and the proximal surfaces of the capitate and hamate. A sagittal ridge can divide the lunate articular surface into radial and ulnar fossae. If this is the case, the proximal surface of the hamate articulates with the lunate. The incidence of this type II lunate varies considerably (27–63% of adults). In a type I lunate, there is no articulation with the hamate and the distal surface of the lunate is concave in both coronal and sagittal planes. The triquetrohamate articulation has a helicoid or screw-shaped configuration. The plane of the joint is not parallel to the articular surface of the distal hamate with the fourth and fifth metacarpals but is situated at a substantial angle (reported as high as 90°).
Finally, there is a joint surface between the triquetrum and the pisiform.
The triquetrum is also an important stabilizer against major torques generated during hand function. Because each of the four joints around the triquetrum requires ligaments to ensure stability, it is not surprising that almost all nonarticular surfaces of the bone are covered by a complex arrangement of ligament attachments (▶ Fig. 18.1).
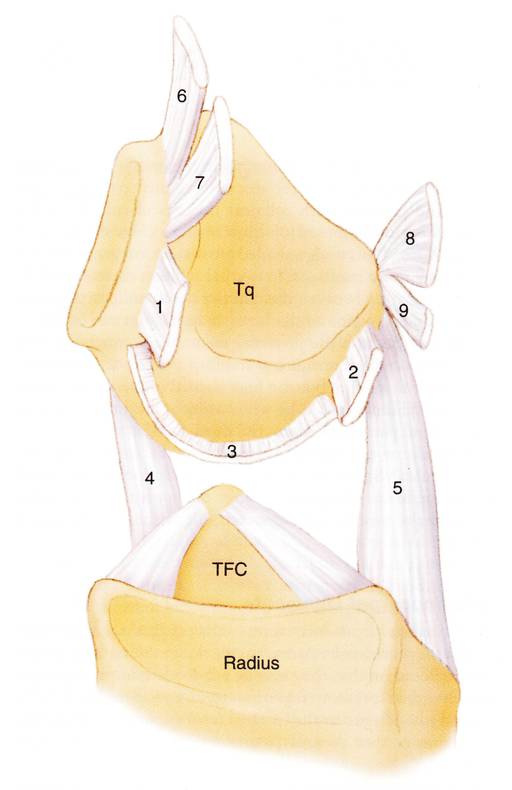
Fig. 18.1 Drawing representing the ligaments attached to the triquetrum (Tq) as seen from the radial side, the lunate having been removed. The LT joint is linked directly by three structures: palmar LT ligament (1), dorsal LT ligament (2), and proximal LT membrane (3). The ulna is connected with the triquetrum by means of the palmar ulnotriquetral ligament (4). The radiotriquetral ligament (5) is wide and fan-shaped and is key in the prevention of carpal collapse. The midcarpal joint is constrained palmarly by two fascicles: the triquetrum-hamate ligament (6) and the triquetrum-capitate ligament (7), both of which are important midcarpal stabilizers. The triquetrum is connected dorsally with the trapezium and trapezoid by means of the dorsal intercarpal ligament (8) and with the scaphoid by means of the dorsal scaphotriquetral ligament (9). TFC, triangular fibrocartilage.(Reprinted from Fractures and Injuries of the Distal and Carpus: The Cutting Edge, Slutsky, D, ed., Chapter 40: Kinematics of the Lunotriquetral Joint, Ritt, MJPF, pp 401–406, 2009 with permission from Elsevier.)
The intrinsic lunotriquetral ligament is C-shaped and is composed of three separate subregions: true ligaments dorsally and palmarly with collinear fascicles of collagen and a proximal region composed of fibrocartilage. In normal subjects there should be no communication between the midcarpal and radiocarpal joints but the proximal region of the LT joint can be perforated by age. Because this proximal region contributes very little to the overall lunotriquetral stability, a defect at this level is not a sign of instability, but can be a normal physiological, albeit age-related, finding, caused by wear.
There are several extrinsic ligaments constraining the LT joint.2 Functionally, these may be subdivided into two major groups: radioulnocarpal ligaments and midcarpal ligaments. Most of these extrinsic ligaments across the radioulnocarpal joint are obliquely oriented relative to the longitudinal forearm axis and based on this, they may be again subdivided into ligaments that control supination and ligaments that control pronation. There is no dorsal or ulnar ligament between the triquetrum and hamate. Because the midcarpal joint is not a true hinge articulation, there are no vertically oriented ligaments. Their absence is functionally substituted by the extensor carpi ulnaris tendon, which is a thick sheath that may act as a dynamic joint stabilizer.
18.3 Material and Constraint Properties
Results of material property testing of the LT ligament showed that the palmar region of the ligament is not only thicker but indeed stronger than the dorsal portion of the ligament (average yield strengths: 301 N and 121 N, respectively). The palmar region was found to constrain primarily translation, whereas the dorsal region provides the majority of rotational constraint. The fibrocartilaginous proximal region failed at 64 N and was the least important constraint in all directions.3 The morphology and material and constraint properties of the LT ligament are the exact opposite of what is found in the scapholunate ligament. Dorsally, the scaphotriquetral (dorsal intercarpal) and radiotriquetral ligaments are important secondary stabilizers of the articulation and can influence the carpal kinematics significantly. Recently, immunohistochemical analysis of wrist ligament innervation showed that sensorily important ligaments were primarily related to the triquetrum, while mechanically important ligaments were primarily located in the radial, force-bearing column of the wrist. The triquetrum and its ligamentous attachments are regarded as key elements in the generation of the proprioceptive information necessary for adequate neuromuscular wrist stabilization.4
18.4 Pathomechanics
The consequences of LT ligament disruptions have been studied extensively in the laboratory. The first study of the role of the LT ligament on carpal kinematics was reported by Reagan et al,1 who also were the first to publish a clinical series of these ligament injuries. They showed that severe lunotriquetral sprains often exhibited a static VISI (volar intercalated segmental instability) deformity and abnormal motion of the carpus. Their clinical series of LT ligament disruptions also showed a more than 30° change in the LT angle compared with normal and an increased proximal migration of the triquetrum on ulnar-deviated posteroanterior radiographs. In 1990, Viegas et al showed that even in partial disruptions of the LT ligament there is increased motion between the elements of the LT joint, a finding later confirmed by others.5 All intercarpal joints have altered kinematics after complete LT ligament sectioning, but the changes are especially marked at the LT joint.6 From multiple biomechanical studies is was concluded that the palmar LT ligament is the major stabilizer of the LT joint during wrist extension and that the rest of the LT ligament provides stability during ulnar deviation. These experiments do not take into account the effect of cyclic loading (where gradual attenuation of the remaining constraining ligaments can change carpal malalignment dramatically) nor the effects of healing and remodeling in living systems. Nevertheless, from most of these cadaver studies, results of which seem to be in accordance with the observations made in clinical practice, one can conclude that injury to the proximal and dorsal parts of the LT ligaments does not cause significant alteration in carpal mechanics; division of the palmar or dorsal part of the LT ligament can cause substantial kinematic dysfunction, sufficient to induce synovitis. Subsequently, a dynamic VISI deformity can arise after cyclic loading and only when the secondary LT joint stabilizers (dorsal radiotriquetral and scaphotriquetral ligaments) are divided does a highly dysfunctional static VISI deformity arise.
There is a general agreement that injuries to the LT ligament are part of a spectrum of progressive ligament disruption. This is associated with perilunate dislocation either in the classic direction or, as is more often the case, in the reverse direction. This concept of a “reversed Mayfield perilunate dislocation model” was discussed by Viegas et al in a biomechanical study.5 The pattern of injury progresses from the ulnar to the radial side in a staged fashion. In 2005 Shahane et al found clinical evidence that this reversed perilunate pattern in most instances is probably the cause for an isolated lunotriquetral injury: in only 7 out of 46 patients with posttraumatic LT instability, did they find evidence of an abnormality on the radial side of the wrist.7
In this situation, isolated injuries to the LT ligaments appear as the consequence of a fall backward on the outstretched hand, with the arm being externally rotated and the wrist positioned in radial deviation and extension. In this way, the impact concentrates on the pisiform. The triquetrum, already in extended position, is translated dorsally but the lunate does not follow: it is effectively constrained by the radius and the long radiolunate ligament. Furthermore, it is likely that this mechanism, with concomitant midcarpal pronation, is able to tighten the ulnocarpal ligamentous complex to a point where isolated failure of the lunotriquetral fibers may occur, whereas the radiocarpal ligaments are spared. Substantial shear stress on the LT ligament causes progressive stretching and, ultimately, tearing of (parts of) the ligament and damage to other lunotriquetral stabilizing ligaments. Complete rupture of the strong palmar portion of the LT ligament rarely occurs unless there is additional violent pronation of the distal row, by which the palmar triquetrohamatocapitate ligament adds the extra destabilizing force that is required for this strong part of the ligament to fail. Frequently encountered associated regional injuries are a peripheral tear of the TFCC (actually the first phase in the experiments by Viegas et al) and a distal avulsion of the ulnotriquetral ligament. It is reported that this combination of injuries is not unusual, and it is easy to miss any one of its components. Avulsion fracture of the palmar rim of the triquetrum should be interpreted as a subtle sign of a more extended lunotriquetral injury and would correlate well with this concept.
In other circumstances, the progression of injury seems to follow a more direct perilunate destabilization process, as described in the well-known paper by Mayfield et al, cited elsewhere. This classic pattern of progressive perilunate instability begins with palmar-to-dorsal disruption of the scapholunate interosseous ligament. In these instances, injury to the LT ligament occurs in stage III, after rupture of the scapholunate ligaments (stage I) and the lunocapitate dislocation (stage II). Lunotriquetral dissociation is an integral part of a progressive perilunate dislocation, but it is difficult to imagine as an isolated finding according to this classic progression pattern. Perhaps isolated lunotriquetral instability represents a residual problem from a previous perilunate injury in which the scapholunate problem heals spontaneously or with intervention.
Acute LT ligament injury is less frequently seen with distal radius fracture than one of the TFCC or scapholunate ligament injuries. Still, partial or complete LT ligament disruption is reported to be associated with intra-articular fractures in a considerable number of cases, ranging from 7% to 24%. Because additional disruption of the palmar arcuate ligament and/or the dorsal radiocarpal ligaments is necessary to produce a VISI condition, this pattern is seldom seen acutely in distal radius fractures.
Finally, ulnar-positive variance can lead to a tear of the triangular fibrocartilaginous complex and ultimately injury or degeneration to mainly the proximal portion of the LT ligament by a wear mechanism. Chronic repetitive stress on the wrist can also predispose to this instability, as was shown by Schroer et al in a group of paraplegic patients.8 Also, patients without history of trauma, inflammatory arthritis, or ulnocarpal abutment also may have degenerative lunotriquetral lesions because this region is prone to age-related degeneration. In all these situations the LT joint is not dissociated and no progressive derotational changes will develop. As was demonstrated in biomechanical studies, however, there is increased mobility of the joint, which can lead to a dynamic instability and local synovitis. Again, only when the dorsal radiotriquetral ligament and the LT ligament are torn does a VISI deformity with a palmar-flexed lunate result.
18.5 Clinical Forms
As a logical consequence from the pathomechanics, as mentioned in Section ▶ 18.4, the clinical picture of lunotriquetral dissociation may vary greatly. It can be an acute or a chronic injury, with almost no apparent abnormalities or on the other hand frank carpal collapse. The problem can be located only on the ulnar side of the wrist or it can be part of a more extensive perilunate instability. Garcia-Elias provided a very elegant subdivision into five more common clinical forms of lunotriquetral injuries. This subdivision is particularly helpful in deciding which treatment is appropriate in the individual cases.9
18.5.1 Acute Lunotriquetral Injury without Carpal Collapse
This is a dynamic instability that is usually only diagnosed by arthroscopy. The degree of lunotriquetral damage can vary but may include a complete rupture of the LT ligament. There is no malalignment of the wrist because the secondary stabilizers of the lunotriquetral joint (extrinsic ligaments) are still intact. The pain that patients experience is a result of increased motion between the two bones—thus, shear stress and local synovitis.
18.5.2 Chronic Lunotriquetral Injury without Carpal Collapse
This entity constitutes the same situation as in Section ▶ 18.5.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








