Closed Lung Trauma
Jeffrey P. Feden, MD, Department of Emergency Medicine, Alpert Medical School of Brown University, 593 Eddy Street, Claverick 2, Providence, RI 02903, USA. E-mail address: jfeden@lifespan.org
Keywords
Thoracic trauma
Pneumothorax
Pneumomediastinum
Pulmonary contusion
Introduction
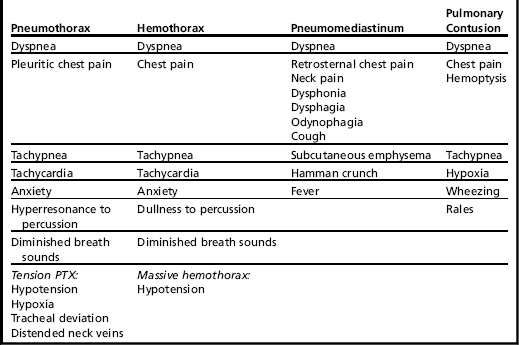
The chest wall is composed of bony, cartilaginous, and muscular structures that serve to protect the thoracic organs and other vital structures, such as the trachea and great vessels. Blunt trauma to the chest wall may cause injury to these underlying structures, and clinical presentations can range from subtle to immediately life threatening (Table 1). Traumatic lung injury can occur from direct force, barotrauma, or rapid deceleration of the organs against the inner chest wall. Such injuries include pneumothorax, hemothorax, and pulmonary contusion. Pneumomediastinum may also result from bronchoalveolar disruption. Because of the potential complications of these conditions, athletes with thoracic trauma demand careful evaluation.
The primary survey
Initial assessment of athletes with thoracic trauma follows the standard principles of Advanced Trauma Life Support, with immediate attention to A: Airway with cervical spine immobilization, B: Breathing and ventilation, and C: Circulation with hemorrhage control.1 The goal of this primary survey is to simultaneously identify and manage life-threatening injuries, such as airway obstruction, tension pneumothorax, massive hemothorax, open pneumothorax, flail chest with pulmonary contusion, and cardiac tamponade. Stabilization of the ABCs is mandatory before addressing less-threatening injuries and completing a more comprehensive evaluation. At the athletic venue, the decision to transport to an emergency department is based on the severity and mechanism of injury, in addition to the presence of respiratory compromise, hemodynamic instability, or clinical concern for potential decompensation.
Pneumothorax
Background
Pneumothorax (PTX) is defined simply as a collection of air within the pleural space. PTX can occur spontaneously or as a result of pleural injury with or without rib fracture after blunt trauma. Penetrating trauma, barotrauma, and iatrogenic causes of PTX are also well recognized. The negative intrathoracic pressure created during the inspiratory phase of respiration increases the tendency of air to leak into the pleural space, and air enters the pleural space until the pressure gradient is equalized.2 Traumatic PTX can result from laceration of the visceral pleura by a fractured rib or from an abrupt increase in airway pressures and bronchial or alveolar rupture (eg, barotrauma). Traumatic PTX is a rare complication of athletic participation but has been reported in contact and collision sports, such as ice hockey,3 football,3,4 rugby,5 and soccer.6 Barotrauma related to scuba diving7 and Valsalva maneuvers during weightlifting8 can also produce PTX. Tension PTX can develop in the setting of a 1-way valve effect, whereby air accumulates in the pleural space with each breath but cannot escape (Fig. 1). Pressure in the affected hemithorax rises and produces tension. This leads to worsening hypoxia, mediastinal shift, decreased cardiac output, and death if left untreated.
The largest series of sports-related PTX was published by Kizer and MacQuarrie9 and documents 20 cases over a 5-year period. All but 1 case were due to blunt chest trauma. Although 9 sports were involved, 11 cases were related to skiing or snowboarding. Other high-energy trauma, such as falls during equestrian sports, has also been associated with PTX.10 Regardless of the mechanism, complications of PTX can be life threatening and must be considered in symptomatic athletes with chest trauma.
Diagnosis and Management
Diagnosis of PTX is commonly made by history and physical examination. Dyspnea with pleuritic chest pain is the classic presentation of PTX. Other clinical manifestations include tachypnea, tachycardia, anxiety, and hyperresonance to percussion and diminished lung sounds on the affected side. Late findings, or findings associated with tension pneumothorax, might include altered mental status, hypoxia, hypotension, distended neck veins, and tracheal deviation away from the affected side.2 Infrequently, PTX may be asymptomatic.11 Clinical suspicion for any thoracic injury should be further evaluated with chest radiographs. Conventional chest radiography (CXR) has long been the initial screening test after trauma. CXR is widely available, noninvasive, and inexpensive and offers a wealth of information. The supine anteroposterior CXR often used in trauma has poor sensitivity, however, and is unreliable in making the diagnosis.2,12–14 With a small PTX, air accumulates in the anterobasal pleural space and may not be seen in the supine position.13 The deep sulcus sign, an exaggerated lateral costovertebral angle (Fig. 2), may be the only clue.15 Upright CXR in stable patients is the preferred technique, because it allows for better visualization of an apical air collection. If upright CXR is not possible, then bedside thoracic ultrasound has proved more sensitive than supine radiography for detection of PTX in blunt trauma patients.12
A growing body of literature supports multidetector CT for the diagnosis of thoracic injuries due to its superior sensitivity compared with CXR.13 With the growth of CT use in trauma, the entity known as occult PTX has emerged. Occult PTX, by definition, is identified only by CT scan and otherwise may go unrecognized.14,16 Much of the existing data, however, are based on motor vehicle and other major trauma, and its clinical relevance to the athletic population remains unclear. Regardless, observation is a reasonably safe strategy in the management of traumatic occult PTX.16,17
Initial management of PTX focuses on an assessment of the airway, breathing, and circulation. Supplemental 100% oxygen should be administered immediately.2 Respiratory distress and/or hemodynamic instability may be signs of tension PTX and must be addressed promptly because cardiovascular collapse and death can result. Treatment of tension PTX is accomplished by needle decompression, in which a 14G or 16G needle is inserted in the 2nd intercostal space in the midclavicular line to relieve pressure. Successful decompression is signaled by a rush of air and clinical improvement, and traditional placement of a large-bore chest tube to allow for lung re-expansion must follow.
Apart from tension pneumothorax, clinical management of PTX has evolved over the years and is based on the type and size of PTX in conjunction with the clinical presentation of the patient. The American College of Chest Physicians published consensus recommendations for the management of spontaneous PTX in 2001.18 Clinically stable patients with a small PTX (<3 cm apex-to-cupola distance; the cupola is the superior pleural dome) may be managed with observation alone and discharged from the emergency department after 3 to 6 hours if repeat CXR excludes progression. A follow-up CXR should be obtained again in no more than 2 days to ensure resolution. Aspiration or tube thoracostomy is unnecessary except in cases where the PTX enlarges. A large PTX (>3 cm apex-to-cupola distance) in clinically stable patients should be re-expanded by insertion of a small-bore percutaneous catheter or large-bore (16F–22F) chest tube, and these patients are typically admitted to the hospital. Clinical stability is defined as respiratory rate less than 24 breaths/min, heart rate between 60 and 120 beats/min, normal blood pressure, room air oxygen saturation greater than 90%, and the ability to speak in whole sentences between breaths. Unstable patients with a large PTX should be hospitalized with a chest catheter, the size of which depends on clinical stability. In contrast to primary spontaneous PTX, secondary spontaneous PTX occurs in the setting of underlying lung disease. A more conservative approach is taken in these patients, with recommendations for hospital observation and a lower threshold for insertion of a chest catheter.
Similar consensus guidelines for the management of traumatic PTX are lacking, but treatment generally parallels that of spontaneous PTX. There is some evidence that stable patients with a simple traumatic PTX can be safely managed without chest drain insertion.19 Otherwise, simple aspiration or chest tube thoracostomy is an effective strategy.2 Obeid and colleagues20 demonstrated the value of treating simple traumatic PTX with catheter aspiration in a small group of patients, although only 1 of these cases was due to blunt trauma. Other studies have similarly concluded that catheter aspiration is a successful, cost-effective alternative in patients with smaller pneumothoraces.21,22 Tube thoracostomy is necessary for large pneumothoraces or for failure of aspiration. The chest tube is removed after the absence of an air leak with the tube to water seal is documented by CXR.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree