Lumbar Laminectomy
Patient Selection
Lumbar stenosis is reduction in size of central, lateral recess, or foraminal lumbar canal
May present with radiculopathy or neurogenic claudication
Indications
Unsuccessful nonsurgical treatment of 3 to 6 months—No satisfactory relief, progressive neurologic deficit, impairment of activities of daily living
Nonsurgical treatment includes weight loss, smoking cessation, physical therapy, injections
Nonsurgical treatment particularly appropriate for patients with nontraditional symptoms and/or discordant history, imaging, physical examination findings
Laminectomy indicated after failure of nonsurgical treatment
Evaluate for spondylolisthesis or instability; both require arthrodesis in addition to decompression
Contraindications
Contraindication for laminectomy without arthrodesis is severe degenerative disk disease with low back pain
Elderly patients with multiple comorbidities
Preoperative Imaging
Plain radiographs
Weight-bearing AP, lateral
Flexion/extension views to assess for instability
CT—Better assessment of bony anatomy such as ossification of the ligamentum flavum
MRI—Helps to assess neural elements and soft tissues
CT/myelography—Helpful if MRI of poor quality, previous surgery with instrumentation, or instrumentation is planned
Procedure
Room Setup/Patient Positioning
Prone position
Jackson table or regular table with bolster under anterior superior iliac spine and chest
Also may position on Wilson frame; creates kyphosis, making decompression easier; may not be beneficial for arthrodesis
Also may use 90/90 position on Andrews frame
Abdomen hangs free to decompress epidural venous plexus
Prepare back in routine fashion
Perform timeout for all surgical team members
Localize levels with fluoroscopy
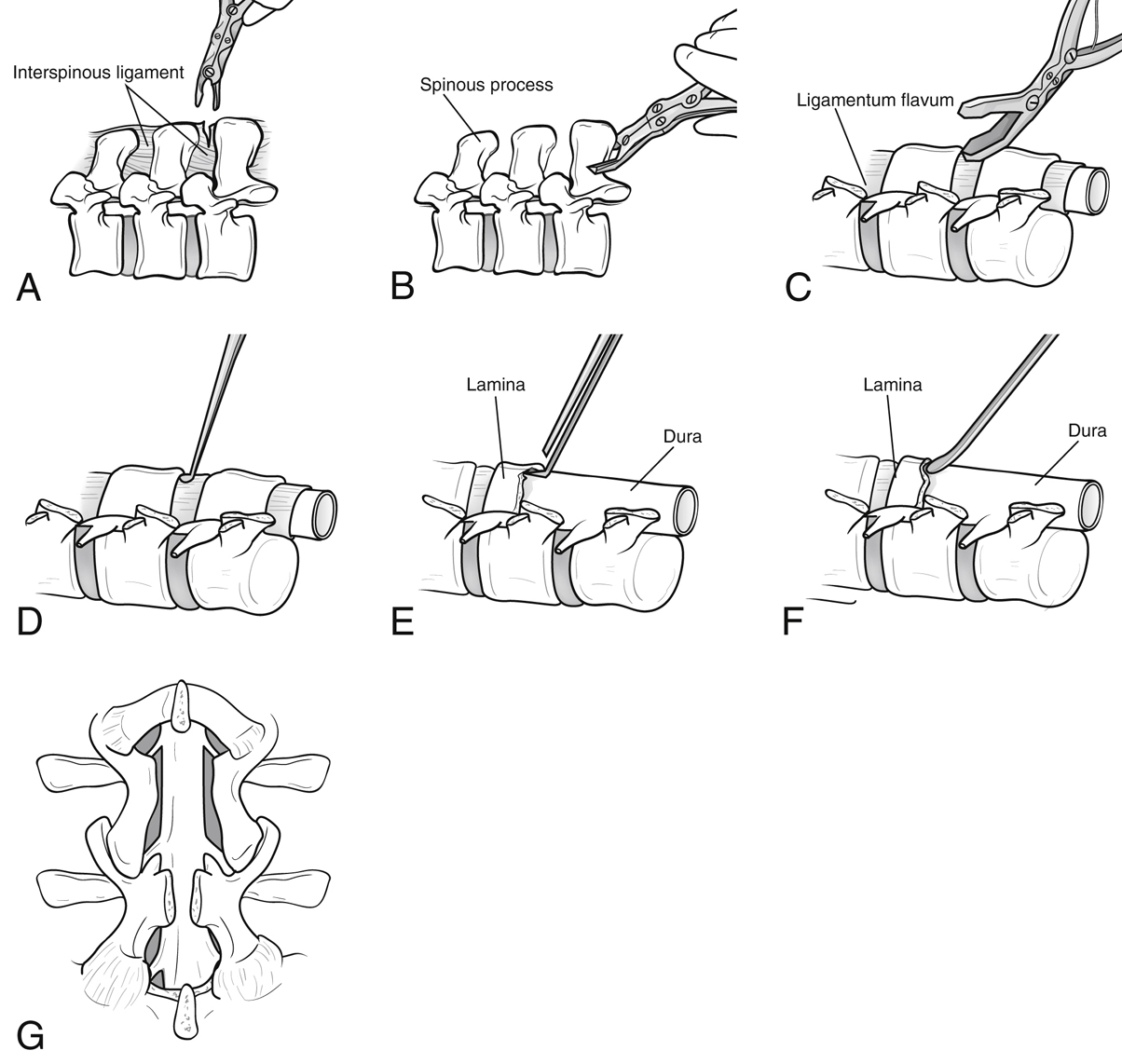
Surgical Technique
Make midline incision; use monopolar cautery to dissect to level of lumbodorsal fascia
Dissect fascia to facilitate reapproximation with watertight closure
Perform subperiosteal dissection to level of lamina
Expose facet joints carefully to lateral aspect without violating capsule; adequately expose pars interarticularis to avoid excessive thinning, which places it at risk for fracture
Confirm levels again using metallic marker of surgeon’s choice and lateral fluoroscopic image