Lumbar Discectomy
Bradley K. Weiner
Ronald Mitchell
DEFINITION
Clinically significant lumbar disc herniations are characterized by a focal distortion of the normal anatomic configuration of discal material resulting in compression and subsequent dysfunction of the lumbar nerve roots.
ANATOMY
The functional components of the intervertebral disc are the annulus fibrosus (fibrous concentric rings, type I collagen) enclosing the central nucleus pulposus (gelatinous, type II collagen, proteoglycans) and the vertebral endplates (hyaline cartilage).
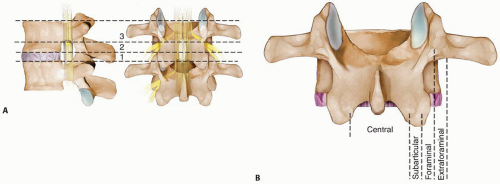
The anatomic unit of the lumbar spine is the vertebral body with its attached posterior elements and the disc below (FIG 1A).
The nerve roots travel within the common dural sac (the cauda equina) and then exit at each level. They are numbered according to the pedicle beneath which they pass.
The spinal canal is divided into zones from medial to lateral: central canal, subarticular zone, foraminal zone, and extraforaminal (far lateral) zone (FIG 1B).
Disc herniations are best classified based on the following ways:
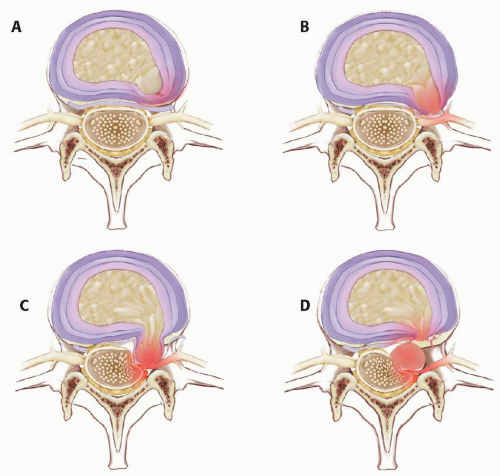
Based on the integrity of the annulus fibrosus and whether there is a connection of herniated discal material with the disc space (FIG 2)
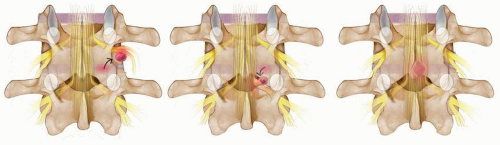
Based on the anatomic location of the herniated material relative to the disc space, the canal, and the compressed nerve root using the nomenclature mentioned earlier (FIG 3)
Accurate anatomic classification of disc herniations facilitates preoperative planning and can minimize the risk of surgical complications such as missed pathology and iatrogenic nerve root injury.
The importance of a complete knowledge of spinal anatomy and understanding of the particular patient’s pathoanatomy cannot be overstated.
PATHOGENESIS
In the normal disc, the nucleus pulposus imbibes and releases water to balance mechanical loads. The annulus fibrosus converts these loads to hoop stresses, thereby containing the nuclear material. The endplates allow diffusion of nutrition into, and waste products out of, the nucleus.
Together, they allow for the three basic spinal segmental functions: mobility, stability, and protection of the nearby neurologic structures.
With early or intermediate disc degeneration (natural aging with or without minor repetitive trauma), the endplates fail to allow adequate diffusion, the nucleus fails to replace degraded proteoglycans, and annular support weakens (failure of cross-linking, development of clefts). Biomechanical dysfunction occurs, with possible herniation of nuclear material.
Many disc herniations do not cause pain or neurologic symptoms. A combination of herniation, nerve root compression, and an inflammatory interface is required for nerve root dysfunction and associated radiculopathy and sciatica.
NATURAL HISTORY
Many studies have shown that with time and nonoperative treatment, over 90% of patients with a first-time lumbar disc herniation will get better without surgery. Accordingly, to propose surgery requires clear indications.
Absolute indications
Bladder or bowel involvement secondary to a massive disc herniation and cauda equina syndrome: immediate surgical intervention
Progressive (ie, worsening) neurologic deficit: the earlier, the better prognostically
Relative indications
Failure of conservative measures greater than 6 weeks to 3 months
Multiply recurrent sciatica
Significant neurologic deficit
In each case, the properly informed patient must clearly understand the current best evidence: Most patients get better quickly with nonoperative care. For those with significant symptoms that are not better within 6 weeks, short-term and long-term (8 years) outcomes are better in patients treated with discectomy as compared with continued nonoperative care.
HISTORY AND PHYSICAL FINDINGS
The most common complaint is pain with or without associated paresthesias or weakness in a specific monoradicular anatomic distribution.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Magnetic resonance imaging (MRI) is the imaging study of choice for the diagnosis and anatomic classification of lumbar disc herniations. It is highly sensitive and specific and provides, along with the clinical picture, adequate information for detailed preoperative planning.
Computed tomography (CT) myelography is invasive and less specific than MRI but provides excellent sensitivity when MRI is unavailable or contraindicated.
Plain radiographs may show disc space narrowing, early formation of osteophytes, or a “sciatic scoliosis.” Although providing no direct evidence of a herniated disc, they may be helpful to rule out unexpected destructive pathology (eg, infection, tumor, fracture) in patients who have failed to respond to nonoperative intervention or those with red flags. They also allow excellent delineation of bony anomalies that may prove vital to preoperative planning and intraoperative localization, such as transitional lumbosacral articulations or spina bifida occulta.
DIFFERENTIAL DIAGNOSIS
Intraspinal, extrinsic compression, or irritation at the level of the nerve root: spinal stenosis, osteomyelitis or discitis, neoplasm, epidural fibrosis (scar)
Intraspinal, extrinsic compression, or irritation proximal to the nerve root: conus and cauda lesions such as neurofibroma or ependymoma
Intraspinal, intrinsic nerve root dysfunction: neuropathy (diabetic, idiopathic, alcoholic, iatrogenic [chemotherapy]), herpes zoster, arachnoiditis, nerve root tumor
Extraspinal sources distal to the nerve root: pelvic or more distal neoplasms with associated sciatic or femoral nerve compression, sacroiliac disease (eg, infection, osteoarthritis), osteoarthritis of the hip, peripheral vascular disease
NONOPERATIVE MANAGEMENT
The evidence base is still a bit unclear, but the following are commonly recommended.
Rest: bed rest (no more than 2 or 3 days), activity or job modification, weight loss
Medication: analgesics (very short term for severe pain only), nonsteroidal anti-inflammatories, tapered doses of oral steroids
Exercise: physical therapy (McKenzie program)
Injections: epidural or selective root blocks (may provide some temporary relief while the natural history takes over)—no impact on long-term outcomes
Time: 6 weeks to 3 months (unless absolute indications for surgery exist as noted earlier)
SURGICAL MANAGEMENT
The evidence base is clear: Open discectomy and microdiscectomy are the operative techniques with the best-documented short-term and long-term outcomes and are the gold standards of surgery for lumbar disc herniations.
Preoperative Planning
This is vital and should aim to answer three questions:
What nerve root is involved (answered by history and physical examination)?
Where is the herniated material relative to the disc space, the canal, and the nerve root (answered by MRI)?
What approach will afford the best visualization and access to the herniated material while minimizing injury to tissues not directly involved in the pathologic process?
Positioning
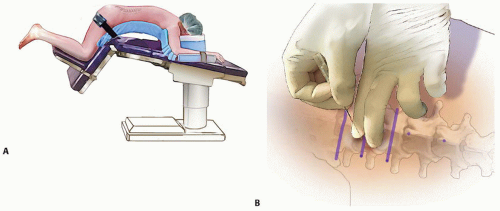
A “kneeling” position is generally used, with the patient stabilized on an Andrews frame, a Wilson frame, or the Jackson table (FIG 4A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree