INTRODUCTION
The rehabilitative care of adults with acquired amputation of the lower extremity as a result of trauma or dysvascular disease is a challenging area of specialization within the field of physical medicine and rehabilitation. Management relies on careful evaluation of the patient, obtained through the history and physical examination, and presupposes a good understanding of the constantly evolving componentry for prosthetic fitting and rehabilitation.
EPIDEMIOLOGY
More than 100,000 major amputations occur each year in the United States. This number is steadily growing as a result of the increasing incidence of diabetes mellitus and dysvascular disease, and the steadily increasing number of individuals older than 65 years. Dysvascular disease accounts for 82% of all amputations, with 97% of these in the lower limb. Trauma accounts for 16% of amputations, with only 32% of these involving the lower limb. Cancer and infection together account for roughly 1% of amputations, with 75% of these involving the lower limb. The remaining 1% of amputations are the result of congenital deficiency or deformity.
There are more than 1.6 million amputee survivors in the United States, and this number is also steadily increasing. One third of these patients are survivors of dysvascular disease; the other two thirds represent traumatic amputation. The long-term survival of the former group is dramatically lower than that of patients with trauma-related amputation.
The perioperative survival rate following lower limb amputation due to vascular disease is 94% for patients with amputation below the knee and 83% for patients with amputation above the knee. The 5-year survival rate for patients with amputation below the knee is 48%, and only 22% for patients with amputation above the knee. The long-term survival rate for patients with traumatic amputation is near normal. The rate of revision surgery for the vascular population is 18–25%, with nearly 10% converting from below-the-knee to above-the-knee amputation. Amputation of the remaining limb is also a significant concern. The risk of having amputation of the remaining limb is greater than 50% at 5 years. The rate of revision surgery for the traumatic population is approximately 14%, with a wound infection rate of 34%. Consequently, although many more amputations due to diabetes and dysvascular disease are performed annually compared with amputations from trauma, the long-term survival of the trauma patient is much better and much longer. The “50–50” rule remains unchanged for the dysvascular population: approximately 50% of vascular amputees die within 5 years of the first amputation, and of the survivors, 50% will lose a portion of the remaining lower limb.
The epidemiology of prosthetic fitting is more difficult to determine. Medicare data indicate that approximately 70,000 new prosthetic devices are fitted each year for new and existing lower limb amputees. This means that roughly 50–70% of new amputees are fitted with a prosthesis each year. The annual cost of prosthetic fit and fabrication exceeds $1 billion per year.
EVALUATION OF THE PATIENT
The opportunity to evaluate the patient before amputation is of great value as it allows for a more comfortable physical examination and offers an excellent opportunity to educate the patient about what to expect immediately after amputation and in the long term. Exercising critical muscle groups in preparation for amputation will make the postoperative physical therapy program much easier for the patient to understand and accomplish, and may shorten the rehabilitation phase. Unfortunately, most patients are evaluated after amputation surgery when pain and immobility make the evaluation more difficult for both the physician and the patient.
Once the history and physical examination have been completed, the medical information obtained should be consolidated and conveyed to the remaining team members to assist in the appropriate multidisciplinary management of the patient. Introduction of the team concept is the responsibility of the physician. Explaining the roles of the physical therapist, occupational therapist, prosthetist, psychologist, pedorthist, and case manager facilitates their interaction with the patient and improves patient adherence with the treatment program.
A thorough history allows the physician to understand the cause of the amputation and the patient’s experience to date. Both the duration of injury or disability prior to amputation and the exact cause of amputation are important elements to be reviewed. The timeframe of disability helps predict the length of recovery and rehabilitation. Documenting repeated surgical procedures or complications (eg, bypass surgery, skin grafts, muscle flaps, and debridement) provides information important to the hospital course. Diagnostic testing, such as arterial, cardiac, pulmonary, and renal studies, provides relevant details about the patient’s underlying medical condition. Review of the past medical history helps the physician to understand the patient’s potential for rehabilitation and ambulation with a prosthesis. Patients with vascular disease commonly have multiple medical problems, including cardiac disease, diabetes mellitus, peripheral neuropathy, vision impairment, and renal failure. It is also important to review the pain history with the patient. Any pain prior to amputation should be assessed, in addition to postoperative surgical pain. Patients with acquired amputation commonly have phantom sensation of the limb but may also have phantom pain of the limb that interferes with their ability to participate in therapy, self-care, or sleep. The treatment for each of these types of pain should also be reviewed carefully.
Review of the social history should include assessment of the social support system at home and the direct involvement of that support system since surgery. Careful review of the patient’s previous level of activity and personal responsibilities should be conducted. Specific questions addressing the patient’s exact level of ambulation just before amputation are critical as they help predict the patient’s functional ambulation with a prosthesis. Examples include, “When was the last time you walked on two feet?” or “Could you walk one block outside?” The patient’s work history should be reviewed for potential return to work. Interest in hobbies and other activities at home should be elicited. The patient’s concerns regarding ability to return to these activities should be addressed early in the rehabilitation phase. Psychological status, including any specific concerns about cognitive status or prospective concern about depression related to the amputation, should also be addressed. The patient’s previous experience with prosthetic devices or conceptions about such devices should be elicited in this early phase to avoid any misunderstanding about the actual function or cosmesis of prosthetic devices. Finally, the history should include issues related to family responsibilities (eg, being a caretaker for younger children) or relationships (eg, the patient’s spouse or significant other). Often the presence or lack of a strong social support system is the factor determining whether a patient is able to return to the home environment and resume many of his or her previous activities.
Physical examination of the patient following amputation should include routine components involving overall hygiene and body habitus; head, eyes, ear, nose, and throat (HEENT); and cardiopulmonary, neurologic, and cognitive examinations. Careful attention should be given to the musculoskeletal and sensory examinations as these will have a direct impact on prosthetic fitting and rehabilitation.
The uninvolved limbs should be examined first, before moving to the involved limb, so the patient will understand the type of examination. Evaluation of the involved limb should clearly define the appropriate level of amputation, including bone length and soft tissue coverage. Skin integrity should be described carefully and a photograph taken, if possible. Overall limb shape, including measurements of the limb, should be noted. Healing at the surgical site or any remaining wounds should be carefully documented. Areas of skin grafting, scarring, or soft tissue adherence should be documented. Tenderness to palpation throughout the residual limb should be assessed as this will determine tolerance to prosthetic fit. Sensation throughout the soft tissue and skin should be recorded.
Manual muscle testing should include all four limbs, but critical areas of strength testing are the hip extensors and hip abductors, knee flexors and extensors, and ankle dorsiflexion–plantar flexion bilaterally, as appropriate. Strength of the upper limbs should also be tested, in anticipation of the need for upper limb strength to use an assistive device both before and after prosthetic fitting. The critical muscles in the upper limb include those involved in grip, elbow extensors, and shoulder depressors. Hand dexterity should be assessed, as peripheral neuropathy may impair sensation and fine motor skills in the hands.
Range of motion for hip extension, knee extension, and ankle dorsiflexion should be assessed because flexion contractures are common following amputation surgery and periods of immobilization. Careful examination of the remaining foot should include assessment of sensation, skin integrity, bony architecture, and vascular status. The remaining foot in the patient with dysvascular disease and major amputation is at high risk for compromised circulation and skin breakdown.
CLASSIFICATION & LEVELS OF LOWER LIMB AMPUTATION
A clear description and understanding of the level of amputation is necessary to understand the prosthetic restoration of the lost limb and the rehabilitation program that will accompany it. The biomechanical changes that occur at each level of limb loss influence the energy cost of ambulation and cardiac demand. The tolerance to prosthetic fit and long-term functional outcome are clearly determined by multiple factors, but most importantly by the level of amputation, soft tissue coverage, proximal muscle strength, and overall medical condition.
Loss of single or multiple toes often has little functional consequence for patients. From a biomechanical perspective, the architecture of the foot is well preserved and much of the weight-bearing surface remains. Use of a protective foot orthotic with a toe filler should be considered to prevent further complications to the remainder of the foot. However, amputation of a toe due to dysvascular disease clearly is a sign that the patient is at high risk for a higher level of amputation, and efforts should be made to monitor and preserve circulation to the remainder of the foot. Protection of both feet with appropriate footwear should be a lifetime management plan.
Transmetatarsal amputation (TMA) is the most common level of amputation when disease or injury compromises the foot proximal to the metatarsal-phalangeal joint. TMA is performed through the midshaft of the metatarsals, using the plantar flap to cover the end of the metatarsal bones (Figure 26–1). Ideally, sensate tissue from the plantar surface will help protect the amputation site during future ambulation. The preservation of dorsiflexion, plantar flexion, inversion, and eversion leaves a very stable and mobile foot for indoor and outdoor ambulation. Prosthetic fitting with a TMA prosthesis includes a combination of foot orthotic and forefoot filler inside an appropriate orthopedic-type shoe. A rigid plate under the prosthesis or a rigid sole on the shoe helps deflect any significant pressure at push-off to the end of the shoe rather than the end of the amputation site.
Other levels of partial foot amputation are less common and sometimes considered less desirable because they compromise the weight-bearing column of the skeleton or the balance of dorsiflexor and plantar flexor muscles. The Lisfranc level of amputation includes loss of all metatarsals and toes, while leaving some tarsals in place (Figure 26–2). This level of amputation compromises the arch of the foot and some of the insertion sites of the dorsiflexors, promoting a plantar-flexed position of the remainder of the foot. This deformity is even more exaggerated with the Chopart level of amputation, in which all tarsals and metatarsals are lost to amputation (Figure 26–3). The prosthetic fitting for these other levels of partial foot amputation requires some type of rigid boot or gauntlet to capture the remaining foot and restore the arch. Unopposed plantar flexion inevitably results in plantar-flexion contracture and weight bearing onto the distal calcaneus, with resultant skin breakdown. To prevent this problem, the Chopart-level prosthesis may incorporate offloading and immobilization of the remainder of the foot, using a bivalve prosthetic shell that transfers the load to the calf or to the patellar tendon area and immobilizes the calcaneus.
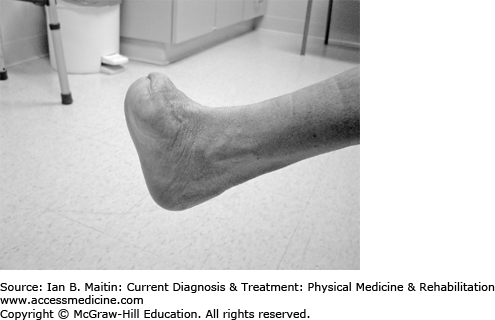
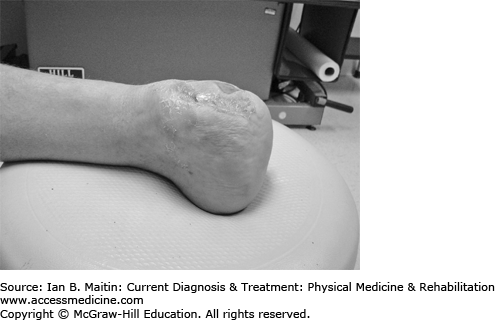
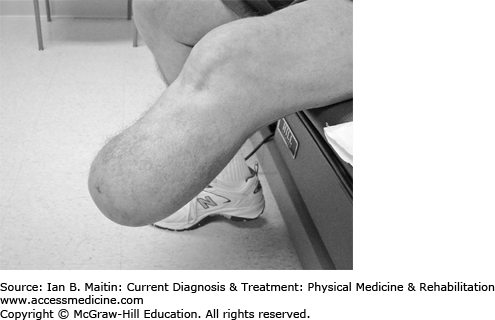
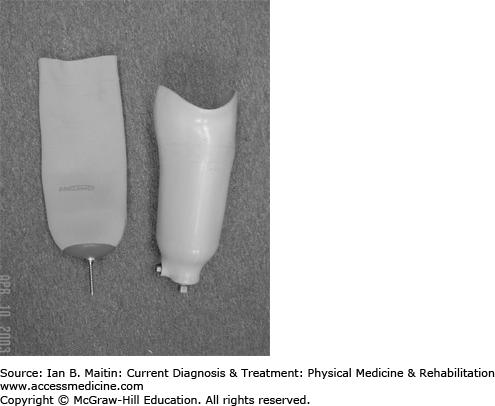
The most common ankle disarticulation procedure is Syme’s amputation. This procedure includes true disarticulation of the ankle and then removal of the medial and lateral malleolus to create a level weight-bearing surface on the tibial articular cartilage. The heel pad must remain intact because it is placed on the end of the tibia to obtain an end-bearing structure (Figure 26–4). The benefit of Syme’s amputation is that it permits partial end bearing and retains the full length of the tibia for excellent leverage and control of the prosthesis. The major disadvantage is the bulk of the distal end, which may lead to a cosmetically unappealing prosthetic socket design. There are also limitations in prosthetic foot availability due to the limited space and height available. The socket design commonly includes a removable medial or posterior window to allow the more bulbous distal end to reach the bottom of the socket (Figure 26–5). Once the window is closed, it captures the narrow portion of the distal tibia creating a self-suspending socket design. Commonly, 50% of weight is placed distally on the tibia and 50% is at the patellar tendon and the medial tibial flair. Migration of the heel pad off the end of the tibia is a common complication and may prevent end bearing.
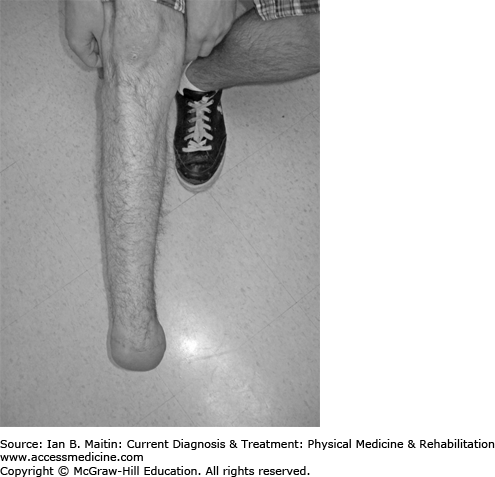
The appropriate bone length in transtibial amputation depends on the quality of the soft tissue, extent of underlying disease, and length of the gastrocnemius–soleus muscle mass. The ideal length can be determined by identifying the musculotendinous junction of the gastrocnemius–soleus muscle and resecting the bone 2–3 cm proximal to this point. This approach should allow sufficient muscle for flap coverage of the distal tibia and fibula, which commonly occurs in the middle or proximal third of the tibia, but rarely in the distal third (Figure 26–6). The minimum length necessary for transtibial amputation is determined by the insertion of the patellar tendon and hamstring tendons. Compromising flexor or extensor mechanisms at the knee will leave a flail segment that may be impossible to fit with a prosthesis. Reconstructive techniques to maintain amputation below the level of the knee should be considered when appropriate. These may include soft tissue reconstruction using rotation flaps or free island muscle flaps to cover bony structures. Skin grafting is also fairly well tolerated at this level of amputation. Preservation of the amputation level below the knee at almost any cost should be considered, since the functional outcome is nearly always better compared with above-the-knee amputation.
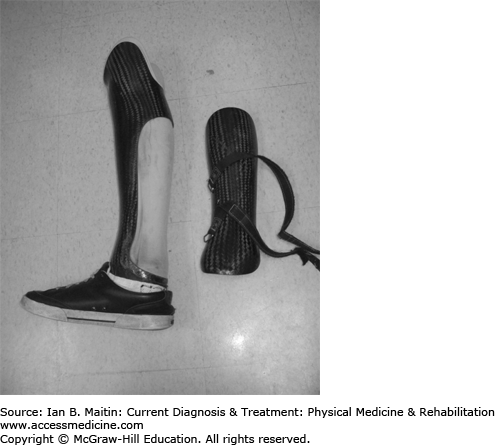
The socket design for transtibial amputation commonly includes total contact with more pressure at the patellar tendon, medial tibial flair, and gastrocnemius muscle. Some newer socket designs also capture the anterior tibial plateau and femoral condyles for additional weight-bearing surfaces. Pressure relief should be provided at the distal tibia and fibula, the fibula head, and the medial and lateral knee joint. The socket walls commonly rise higher on the medial and lateral sides to provide additional stability but are lower at the posterior wall to maximize knee flexion for sitting. The posterior brim of the socket should match the height of the patellar tendon–bearing (PTB) bar anteriorly. There is always a soft interface and rigid outer frame in the transtibial socket. The interface is commonly a soft foam material for a temporary prosthesis, and a gel material for the permanent prosthesis. Initial use of the soft foam material allows for adjustments to be made with pads to accommodate for volume loss as the limb shrinks and atrophies. Once the patient’s limb shape has stabilized, the use of a gel liner with or without pin suspension provides a stable cushion interface for higher-level activity (Figure 26–7). The outer rigid socket may utilize a carbon fiber laminate or a thermoplastic design. The suspension options include a supracondylar wedge, elastic sleeve, suction system, thigh corset, and elevated vacuum system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree