Fig. 11.1
Tibia stress fracture. (Note: dreaded black line)

Fig. 11.2
Bone scan with focal uptake of tibia stress fracture

Fig. 11.3
Tibia stress fracture status post intramedullary nail at 6 months
Epidemiology
With a reported incidence of 0.5 %, tibial stress fractures can be found among a well-defined, broad demographic population [2]. More classically, distance runners and military recruits have sustained higher rates of stress injuries, particularly those involving the tibia [3–5]. However, these injuries are not specific to these cohorts as tibial stress fractures have been described in a variety of sports such as ballet, volleyball, rowing, basketball, and gymnastics [6].
Among military populations, tibial stress injuries typically occur in untrained service members undergoing repetitive, intense physical activity and/or training programs for combat readiness, such as in basic training or advanced specialized military courses. Several studies have demonstrated that 1–31 % [4, 7] of military recruits will incur a stress fracture, while up to 53 % may experience MTSS [8]. Cosman et al. demonstrated that the cumulative 4-year incidence of single-stress fractures among US Military Academy (USMA) cadets was 5.7 % for males and 19.1 % for females, with approximately 50 % of injuries occurring within the first 3 months of enrollment [9]. Among the broader US Armed Forces, Lee and colleagues [10] determined that the mean annual incidence rate of tibial stress fractures was 3.24 per 1000 person-years between 2004 and 2010. In the largest sample of US Army recruits, the incidence rate of tibial stress fractures was 19.3 and 79.9 cases per 1000 male and female recruits, respectively [5]. In addition to the medical burden of injury, the financial repercussions of stress fractures is not negligible, with the estimated cost approximately US$34,000 per US service member [11].
Many factors may contribute to the development of a tibial stress fracture. These are typically separated into intrinsic and extrinsic risk factors. However, more recently, the medical and public health community has been increasingly focused on the identification of modifiable risk factors as a means to improve injury prevention. Intrinsic factors for tibial stress fractures, including female sex, white race, older age, increased bone turnover, anatomic malalignment, and decreased tissue or bone vascularity have been identified and are largely non-modifiable. General physical fitness, muscle endurance, bone density, steroid or tobacco use, excessive alcohol consumption, and hormonal deficiencies are among the intrinsic factors that may be alternatively considered modifiable variables. Extrinsic factors include training regimen, dietary or nutritional profile, footwear, and training surface, and these factors may also be considered as targets for intervention and risk mitigation [12, 13].
Female sex is among the more notable risk factors associated with stress fractures, particularly within the military, in general, where they are at up to a 2- to 12-fold greater risk of stress injury than males [14–21]. While classically associated with the female athlete triad (i.e., eating disorders, functional hypothalamic amenorrhea, and osteoporosis), stress fractures can arise as a result of a multitude of factors. Known risk factors include underlying differences in bone geometry (e.g., smaller and more narrow tibia) and microarchitecture (e.g., decreased bone mineral density, greater trabecular volume), altered hormonal regulation, nutritional deficiencies, reduced muscle mass, and diminished physical fitness [20]. Given communal training within the military setting, lower levels of physical fitness among women lead to greater comparative physical effort, earlier fatigue, and altered gait or running mechanics, which could further exacerbate the risk of overuse injuries in the lower extremity [14, 22].
Training regimens, primarily dramatic increases in vigorous impact and running activity, contribute significantly to the development of tibial stress injuries. As a result, the study among military cadets and recruits during basic training is ideal and has helped develop the existent body of literature. In contradistinction to athletics where physical activity is more consistent throughout adolescence and adulthood, military enlistment is often preceded by a period of sedentary lifestyle or decreased general fitness, which may heighten secondary risk of stress fracture. Cosman and colleagues [9] demonstrated that cadets at USMA were at a twofold greater risk of stress injury when they had exercised less than 7 h per week in the year prior to matriculation. Furthermore, the rate, duration, and intensity of military training (e.g., marching, running) have been associated with rates of tibial stress fracture [10]. Consequently, redesigned training programs with decreased cumulative exposure, implementation of minimum sleep requirements, and greater emphasis on agility exercises and cross-training have been successful at mitigating the rates of tibial stress fracture without compromising unit readiness [10, 23, 24].
While there have been several attempts at preventative treatment, few measures have led to a decrease in rates of tibial stress injury. Adjusted training schedules and individualized risk stratification have been most successful in injury reduction [10, 25]. There is also limited evidence that suggests a relative risk reduction with the use of shock-absorbing insoles when compared with controls. However, the optimal insole design and shoe wear modifications are undetermined. Calcium and vitamin D supplementation have been widely promoted for the prevention of fragility fractures, and recent evidence certainly supports its use within a military population at risk for tibial stress fractures, particularly when deficiencies or other risk factors exist [26]. Conversely, pre-exercise stretching and medial arch supports for excessive pronation have not been found to demonstrate a protective effect from stress-related fracture [27].
Chronic Exertional Compartment Syndrome
Introduction
Chronic exertional compartment syndrome (CECS), or exercise-induced compartment syndrome, is a common source of lower extremity disability among active patients. First described by Mavor in 1956, CECS has historically referred to involvement of the leg, although cases affecting the shoulder, upper arm, forearm, hand, gluteus, thigh, and foot have also been described [28].
As with other overuse conditions of the lower extremity, the pathophysiology of CECS is only partially understood. During normal exercise, the muscle volume increases by up to 20 % or up to 20-fold greater than its resting size, with pressures exceeding 500 mmHg [29]. In response to increased metabolic demands, blood perfusion rises in turn with accumulation of interstitial fluid. However, when this is coupled with chronic fascial thickening, limited tissue compliance [30], diminished capillary density [31], and/or elevated baseline intracompartmental pressures, patients with CECS are unable to accommodate exercise-related changes and experience symptoms as a result of relative tissue ischemia and nerve compression [32]. In response to these changes, patients complain of pain and neurovascular symptoms, which often precipitate early cessation of athletic activity and military training. Alternatively, acute compartment syndrome represents a surgical emergency where tissue ischemia occurs following a traumatic injury or other underlying systemic process, and this should not be confused with CECS.
Epidemiology
CECS occurs most commonly in avid runners, military recruits, and competitive athletes involved in sports such as basketball, soccer, and football. The prevalence of CECS varies widely, with reported rates ranging from 10 to 60 % in selected cohorts [33–35]. In a recent evaluation of US military service members over a 6-year time period, the incidence rate of CECS was approximately 0.5 per 1000 person-years [36]. However, given the systematic underreporting coupled with inconsistent diagnostic criteria and specificity, the comprehensive burden of CECS is unknown within the military setting .
Traditionally, CECS has been described among young, active male athletes and military recruits, and the preponderance of cases occur among this demographic [36, 37]. However, limited research may suggest disparate epidemiological trends among patients with CECS, particularly among nontraditional cohorts recently exposed to the rigorous physical demands of the military. As military enlistments and athletic involvement have both continued to increase among females, there has been greater parity in at-risk exposure between males and females. Recent studies demonstrate increased risk among females including one study in US military service members [31, 36]. By contrast, multiple earlier studies suggest no difference in the incidence among men and women [30, 33, 37]. When evaluating by age, Waterman and colleagues [38] also showed a positive association between increased age and the incidence rate of CECS, with patients over 40 years demonstrating a nearly ninefold greater rate of CECS versus those under 20.
Non-commissioned service members, primarily those of junior rank and Army service, showed the highest rates of CECS. This likely reflects the unique physical demands of the junior enlisted service members, often serving in ground military forces with frequent exposure to organized physical fitness training, dismounted field activity, and prolonged marching with a combat load. Overtraining has been implicated, and junior service members may be less able to moderate these intense occupational demands to accommodate physical limitations arising from CECS [38, 39].
In addition to demographic variables, several modifiable factors may also serve as targets for intervention. Abnormal gait patterns and/or prolonged muscular contraction during aerobic exercise may exacerbate the underlying pathophysiology of CECS, by limiting peripheral vascular perfusion during muscle relaxation and increasing intracompartmental pressures. Additionally, repetitive eccentric exercise may diminish fascial compliance with continued exposure, as occurs with the anterior compartment during running [40]. As a result, newer literature has investigated the role of running technique, specifically a forefoot contact pattern, in reducing intracompartmental pressures and mitigating the symptoms related to CECS [41, 42]. In an evaluation of a 6-week forefoot training program for cadets with CECS at USMA, Diebal and colleagues [43] demonstrated significant reductions in anterior compartment pressures (78.4 +/− 32 vs. 32 +/− 11.5 mmHg) and vertical ground-reaction forces, while improving running distance, speed, exertional pain, and patient-reported outcome measures at up to a year after intervention. Furthermore, all patients avoided surgery and remained on active duty without physical activity restrictions. Creatine and anabolic steroid use can also lead to increased intramuscular fluid volume and hypertrophy, thus diminishing potential space for normal volume expansion and increasing intracompartmental pressures with exercise activity .
While certain anatomic features mentioned previously have been associated with the development of CECS, the role of fascial defects of the leg remains uncertain. Between 10 and 60 % of patients presenting for treatment of CECS also had clinically evident fascial defects [39], compared with less than 5 % among asymptomatic individuals [28]. While only 1–2 cm2 in size, this fascial defect may serve as a site for adjacent superficial peroneal nerve entrapment when localized to the anterolateral intermuscular septum. With continued exercise, muscle and neurovascular herniation may occur, leading to further, localized inflammation and/or micro-ischemia. Further studies are required to better elucidate the underlying contribution of these fascial defects, as well as the underpinnings of disrupted arteriolar homeostasis thought to be central to the development of CECS [28].
Ankle
Ankle Sprain
Introduction
The so-called ankle sprains can often collectively represent a spectrum of traumatic soft tissue injuries about the ankle and hindfoot, but the diagnosis classically denotes ligamentous instability about the tibiotalar joint with varying degrees of severity [44]. Traditionally, ankle instability comprises three discreet categories of injury, including lateral, medial, and syndesmotic ankle sprain. However, combined ligamentous involvement and other associated injuries, particularly those involving the chondral surface of the talar dome and peroneal tendons, are common. Sprains involving the lateral ligament complex, including the anterior talofibular ligament, calcaneofibular ligament, and posterior talofibular ligament, account for at least 85 % of all ankle sprains [45] (Figs. 11.4 and 11.5). Conversely, syndesmotic, or “high ankle sprains,” and medial ankle sprains are diagnosed in only approximately 10–15 % of patients with ankle sprains, and the epidemiological literature is fairly limited [46]. The focus of the current review will further elaborate largely on lateral ankle instability.
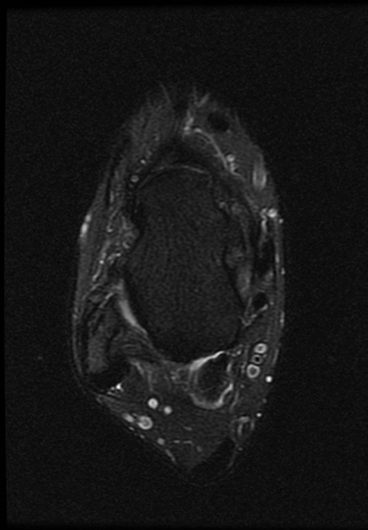
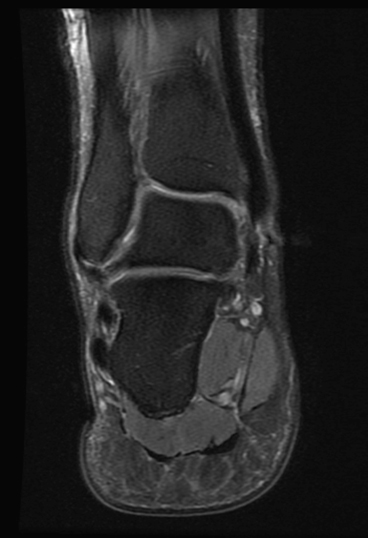
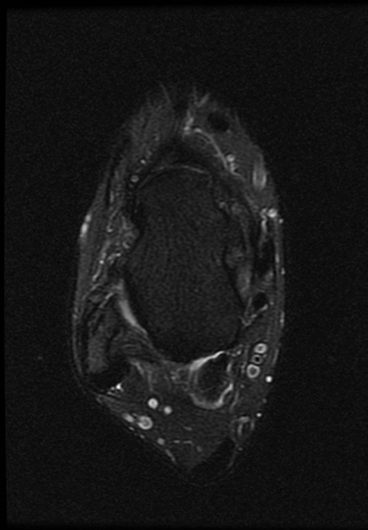
Fig. 11.4
Axial T2 MRI—anterior talofibular ligament (ATFL) disruption
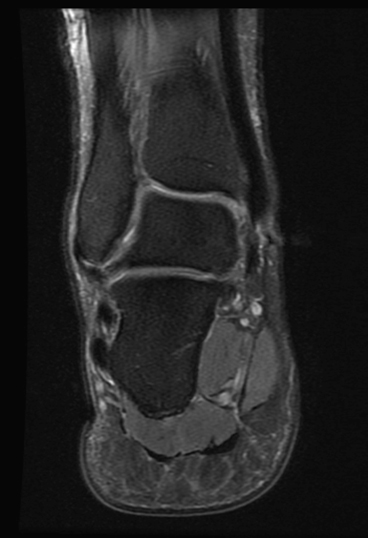
Fig. 11.5
Coronal T2 MRI—CFL disruption
Epidemiology
In active , athletic populations, ankle sprains account for up to 30 % of single-sport injuries. Nearly 1.2 million ankle-sprain-related health-care visits occur per year, with an estimated cost of up to US$3.8 million for both treatment and rehabilitation [47, 48]. The incidence rates of ankle sprain may vary , with between 2 and 7 individuals per 1000 in the general population injured per year [49–51]. However, the risk of ankle sprain is an order of magnitude greater in military cohorts, with reported incidence rates ranging from 35 to 58.4 per 1000 person-years in previous studies [46]. Among military personnel, paratroopers are at a particularly elevated risk. Lillywhite [52] identified that between 0.6 and 1.2 % of Royal Army paratroopers sustained ankle injuries per year, with increases up to 7.9 % on mass descents. Further studies have shown that ankle sprain accounts for 9–33 % of parachute-related injuries and have an incidence rate between 1 and 4.5 per 1000 jumps [53, 54].
To better understand and anticipate the epidemiology of this injury, several authors have sought to identify modifiable risk factors associated with lateral ankle sprain [46, 55–57] (Table 11.1). Non-modifiable risk factors can be useful in identifying high-risk populations for injury prevention, while modifiable risk factors such as body mass index (BMI), proprioception or postural stability, and the absence of external restraints to inversion (e.g., prophylactic bracing) can be the targets for intervention [57]. Within the context of this framework, several risk factors for ankle sprain will be discussed.
Non-modifiable risk factors | Modifiable risk factors |
|---|---|
Sex | Weight |
Age | |
Height | Bracing/taping |
Race | Footwear |
Foot/ankle anatomy | Neuromuscular control |
Extremity alignment | Postural stability |
Previous ankle sprain | Muscle strength |
Generalized joint laxity | Exposure to sport |
Player position | |
Playing surface | |
Skill level |
Non-modifiable Risk Factors
Gender
With the increasing popularity and involvement of female athletes in sports, gender-related studies of musculoskeletal injury have become important in determining potential health disparities. The underpinnings of these gender-based discrepancies are likely multifactorial, with several postulated associations including inherent hormonal differences, lower extremity anatomy, limb alignment, ligamentous laxity, neuromuscular control, and the extent and type of athletic exposure [57, 58].
Gender studies on ankle sprain incidence, however, have yielded mixed results. A study of military cadets showed incidence rates (IR) of ankle sprain as 96.4 and 52.7 per 1000 person-years for women and men, respectively (incidence rate ratio (IRR) of 1.83 (95 % confidence interval (CI) 1.52–2.20)), while no differences were detected between the male and female intercollegiate athletes [51]. In a separate study of collegiate athletes, Beynnon et al. showed IRs of 1.6 and 2.2 per 1000 person-days for men and women, respectively, although the difference was not statistically significant [59]. Hosea et al. subsequently found that while female athletes had a 25 % greater risk of sustaining a grade I ankle sprain compared with their male counterparts in both high school and intercollegiate basketball, there was no significant difference in the risk for the more severe ankle sprains [60].
Further studies in the general population of the USA show no overall differences by gender, although male individuals between the ages of 15 and 24 and female individuals over the age of 30 had higher rates of ankle sprain than their opposite sex counterparts [51]. A population-based study of active duty military personnel revealed that female service members experienced an incidence rate that was 21 % higher than that of male service members [46]. Based on the available literature, gender appears to be associated with risk of ankle sprain, although additional factors such as exposure to and level of at-risk activity may directly influence this complex relationship.
Age
Younger age, particularly when associated with increased exposure to at-risk activity, is also associated with the risk of ankle sprain. Studies of the general population of the USA [46] and Denmark [50] yielded a mean and median patient age of 26.2 and 24.4, respectively. A recent population-based study within an active duty military population reported the highest incidence rates for ankle sprain in the group of those under 20 years old for both male and female subjects, and rates generally declined with increasing age [57]. These studies suggest that peak incidence rates for ankle sprain occur during the second decade of life, with male and female peak incidence rates occurring between the ages of 15 and 19 and 10 and 14, respectively [49, 51].
The mechanism of injury for ankle sprain also varies by age, with a greater preponderance of injuries occurring during recreational or competitive sports in young, active populations [46]. Patients under 25 years of age were more likely to sustain ankle sprains while engaging in athletics and physical activity, while patients over 50 were more likely to incur ankle sprain in their own homes or during activities of daily living [50].
Previous Ankle Sprain
Ankle sprain produces damage to ligaments that maintain the stability of the ankle joint, thereby creating potential functional limitations. Some of this damage, such as that resulting in proprioceptive or neuromuscular impairment, is modifiable through exercise. However, the initial inflammatory response following injury can also lead to scar tissue formation, which is more likely than normal tissues to fail due to a 60 % reduction in energy-absorbing capacity [61].
Functional instability and increased risk of reinjury may still occur after primary ankle sprain in athletes and military recruits undergoing basic training even if the primary sprain is on the less severe end of the injury spectrum [62–65]. A recent study on track and field athletes and rates of reinjury within 24 months demonstrated that athletes with a grade I or II lateral ankle sprain were at higher risk of reinjury (14 and 29 %, respectively) than high-grade acute lateral ankle sprains (5.6 %) [65]. However, this may also be related to inadequate rehabilitation of less severe injuries and earlier perceived healing despite persistent proprioceptive impairment, which ultimately increases further risk of recurrence .
Modifiable Risk Factors
Weight and BMI
With increasing weight and BMI , an increasing mass moment of inertia acts about the ankle, potentially increasing the risk of ankle sprain. In a study on high school football players, Tyler et al. [66] showed that the incidence of ankle sprain was significantly increased in patients with BMI categorized as above normal or overweight when compared to players with a normal BMI. Waterman et al. [46] reported similar findings in military cadets with ankle sprains who had higher mean weight and BMI than their uninjured counterparts. Interestingly, in the same study, no statistically significant differences in height, weight, or BMI were observed between the injured and uninjured female cadets, but this may have been due to the limited female representation within the studied cohort .
Despite the evidence that weight and BMI are associated with an increased risk of ankle sprain, other studies have failed to demonstrate that these anthropometric measures are independent risk factors for ankle sprain [59, 67]. Certain athletic cohorts or player positions with elevated BMI may be at a greater predisposition for ankle sprain; further research is required to discern these subtle differences.
Neuromuscular Control/Postural Stability
Proprioception and broader neuromuscular control were first proposed as a risk factor for ankle sprain by Freeman et al. [68] in 1965. Subsequent studies have extensively and rigorously evaluated proprioceptive deficits after primary ankle sprain and described their resultant effects on strength, postural balance, and ankle stability, particularly in athletic populations [69–71]. Furthermore, McGuine et al. [72] demonstrated that high school basketball athletes who subsequently sustained ankle sprains had significantly greater measures of pre-injury postural sway when measured with stabilometry than their uninjured counterparts, indicating an underlying neuromuscular predisposition. Other studies have reported similar results with clinical assessments of postural stability [73].
However, while gross morphologic changes and disrupted afferent nervous networks have been noted with ankle sprain and resultant postural instability, its causal link with chronic ankle instability is less clear [74–76]. Muscular fatigue or diminished baseline strength may potentiate neuromuscular impairment and contribute to subsequent ankle instability [77].
Sport
Certain athletic activities increase the likelihood of ankle sprain, particularly those that involve frequent running, cutting, and jumping movements. Analysis of the National Electronic Injury Surveillance System (NEISS) for all ankle sprain injuries presenting to emergency departments over a 5-year time period revealed that 49.3 % of ankle sprains were caused by participation in sports; basketball (41.1 %), football (9.3 %), and soccer (7.9 %) accounted for more than half of all ankle sprains during athletic activity [51].
A more expansive systematic review of ankle sprain epidemiology revealed that incidence rates varied depending on the unit of measurement [78]. When evaluating for incidence per 1000 person-hours, rugby had the highest incidence (4.20), followed by soccer (2.52). Conversely, when considering incidence more accurately in terms of athletic exposure, lacrosse had the highest incidence rate (2.56) of sprains per 1000 person-exposures, followed by basketball (1.90). Similarly, Waterman et al. [46] found that basketball (men’s, 1.67; women’s, 1.14), men’s rugby (1.53), and men’s lacrosse (1.34) were among the highest incidences per 1000 person-years among intercollegiate athletes.
Level of Competition
As a broad category, level of competition has also been identified as a potential risk factor for ankle sprain. Traditionally, level of competition has been synonymously used to describe both intensity of competition (i.e., practice vs. game) and level of skill (e.g., recreational, intercollegiate, and professional). However, both of these components represent distinct variables that should be separately considered and evaluated.
When considering intensity of competition, there is a positive relation between higher level of play and increased risk of ankle sprain, with approximately 55–66 % of injuries occurring during games when compared to training sessions [79–82]. This is likely attributable to the increased risk-taking activity and pace of play .
There is less of a consensus on the impact of skill level on the incidence of ankle sprain. Our previous work has revealed that ankle sprain incidence in intercollegiate athletes was seven times that of intramural athletes in terms of injuries per 1000 person-years [46]. However, when more specifically controlling for the extent of athlete exposures, no significant differences between intramural and intercollegiate athletes were noted. Other prior studies evaluating skill level are conflicting; one report notes an increased risk in higher-level intercollegiate athletes [60]. Conversely, two additional studies have revealed an increased risk of sports injuries in lower-skill soccer athletes than their higher-skill cohorts [83, 84].
Preventative Measures
Reasonable measures may be implemented to mitigate modifiable risk factors and reduce the risk of ankle sprain. Several interventions have demonstrated success in achieving these goals without significant effects on quality of life or athletic performance. By increasing passive restraints to ankle inversion and enhancing postural stability, prophylactic bracing in high-risk athletes and selected military personnel can be effective in reducing the risk of primary and recurrent ankle sprain by up to 50 % [27, 67, 89]. In one prospective randomized trial, Sitler et al. [67] showed a threefold increased risk for ankle sprain among unbraced basketball players when compared to braced athletes over a 2-year time period at the USMA. Among paratroopers, a recent systematic review revealed that an external parachute ankle brace reduced all ankle injuries, including ankle sprain, by approximately half while saving between US$0.6 and 3.4 million in direct and indirect costs [54].
Furthermore, neuromuscular training programs have also shown merit in reducing the risk of ankle sprain. In a meta-analysis, McKeon et al. [76] confirmed that prophylactic and targeted balance control training resulted in a 20–60 % relative risk reduction for sustaining lateral ankle sprain, particularly in those individuals with prior history of ankle sprain. With more consistent screening of high-risk athletes and better-instrumented measures for diagnosis, prophylactic interventions may gain more widespread popularity and effectively reduce the incidence of ankle sprain .
Osteochondral Lesions of the Talus
Introduction
Osteochondral lesions of the talus (OLTs) encompass a broad spectrum of terms previously used to describe injury to the articular talar dome, including osteochondritis dissecans, transchondral talus fractures, and osteochondral talar fractures (Figs. 11.6–11.8). An OLT can occur in association with a severe, acute ankle sprain, and the majority of patients will note an acute injury or remote history of trauma. Alternatively, an OLT can also arise from chronic ankle instability due to the repeated shear stress or edge loading of the articular surface. An estimated 50 % of all acute ankle injuries have articular cartilage injury of the talus, while up to 73 % of ankle fractures are associated with chondral lesions [90, 91]. Early descriptions identify a strong association between lateral lesions of the talus and traumatic injury. Berndt and Harty [92] proposed that compression injury happens to a dorsiflexed and inverted ankle, while medial lesions can arise from inversion and external rotation onto a plantarflexed joint. However, the pathogenesis of medial OLTs is less clear and may also be associated with chronic instability, other mechanisms of injury, or atraumatic etiologies [93]. Other proposed causes include degenerative ankle arthropathy, heritable predispositions, underlying metabolic or endocrine disorders, systemic vasculopathy, joint malalignment, and excessive alcohol use [94, 95]. Due to their extensive cartilage surface, tenuous vascular supply, and limited capacity for repair, OLTs lead to chronic pain, swelling, and mechanical symptoms, while the lesion may become unstable, enlarge, or ultimately progress to osteoarthritis if left untreated [93]. Additionally, ankle synovitis, osteophyte formation, loose bodies, and peroneal tenosynovitis or tears may be present in up to 93 % of patients with chronic OLTs [96].


Fig. 11.6
Coronal CT—osteochondral lesion of the talus
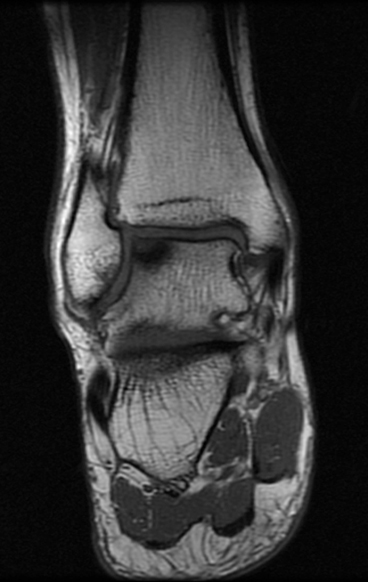
Fig. 11.7
Coronal T1 MRI—osteochondral lesion of the talus
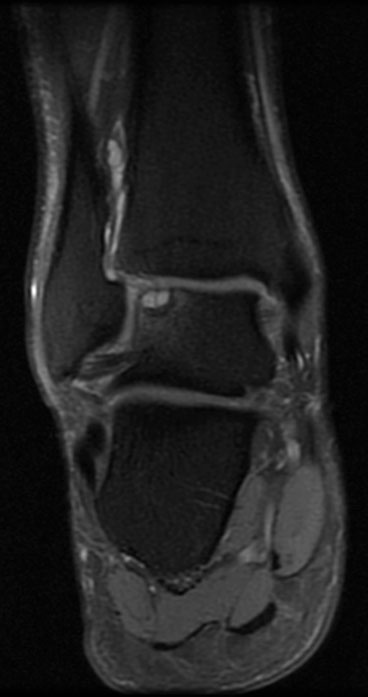
Fig. 11.8
Coronal T2 MRI—osteochondral lesion of the talus
Epidemiology
OLTs comprise approximately only 0.1 % of all fractures of the talus and up to 0.09 % of all fractures. Approximately 6.5 % of all ankle sprains had OLTs when evaluated arthroscopically, while between 23 and 95 % of patients undergoing lateral ankle stabilization for chronic instability demonstrated chondral lesions of the talus with increased risk among athletic populations [96–99]. In a study of OLTs among the US military over a 10-year period, Orr et al. [94] reported that the unadjusted incidence rate was 27 per 100,000 person-years, with increased risk among individuals of female sex, white race, enlisted military rank, Army or Marine Corps service, and increasing chronological age. The authors suggest that cumulative exposure to intense occupational demands, particularly among the enlisted ranks and ground forces during a time of war, may explain the temporal and age-related trends observed in their study. Prior studies have also emphasized the increased risk of OLTs in the second to fourth decade of life, spurned by a combination of peak physical activity and age-related diminution of the biomechanical properties of articular cartilage [94, 100, 101].
As with ankle sprains, the treatment and preventative strategies for OLTs should be targeted at mitigating further ankle instability. Physical therapy, bracing, and symptomatic management with nonsteroidal, anti-inflammatory medication may limit OLT propagation or osteochondral fragment displacement, where surgical considerations for chondral restoration are more immediately appropriate (Figs. 11.9 and 11.10). However, nonoperative management has limited success, with reported rates of acceptable outcomes ranging from 45 to 59 % [102, 103].
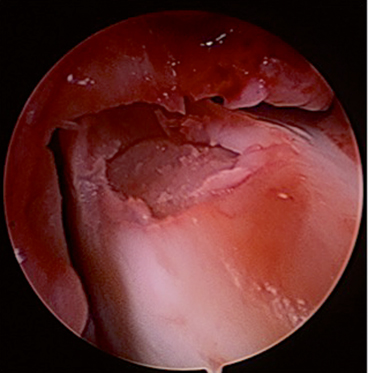
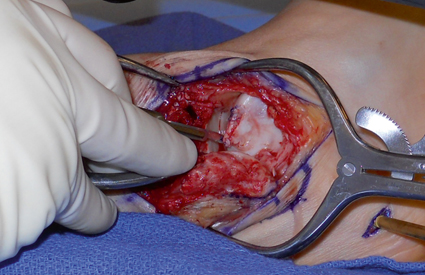
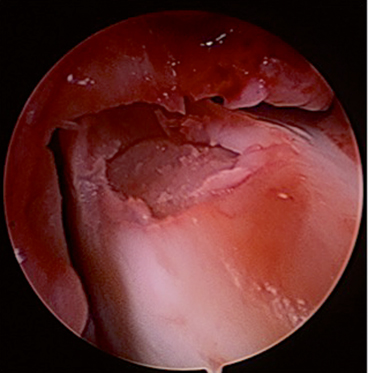
Fig. 11.9
Intraoperative arthroscopic image of lateral osteochondral lesion of the talus
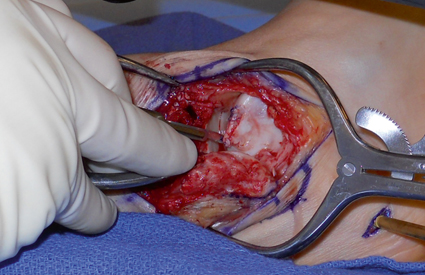
Fig. 11.10
Intraoperative open image of lateral osteochondral lesion of talus
Peroneal Tendon Pathology
Peroneal tendon pathology is associated with ankle instability or other acute ankle injury and should be suspected in any patient with chronic lateral ankle pain. Normally restrained by the superior peroneal retinaculum in the retromalleolar sulcus, the peroneus longus and brevis primarily act to plantarflex the great toe and evert the foot, respectively. In addition to these functions, the peroneal tendons also act as dynamic lateral stabilizer of the ankle, particularly during the midstance phase of gait [104]. However, the peroneal tendons can become unstable with forced dorsiflexion and eversion upon an inverted ankle, leading to tendon subluxation, longitudinal tears, and other post-traumatic tendinopathy. A low-lying peroneus brevis muscle belly, an anomalous peroneus quartus, hypertrophied peroneal tubercle, or specific anatomic variants of the retromalleolar sulcus (i.e., absent or convex morphology, calcaneal tunnel) can predispose patients to mechanical symptoms or instability, and assessment of hindfoot alignment should also be performed to rule out varus deformity as a contributing factor [105–108]. Other underlying comorbidities, including diabetes mellitus, hyperparathyroidism, rheumatoid arthritis, and psoriasis, may also contribute to peroneus longus tears, although the majority of these injuries occur during athletic injuries or other acute trauma [104] (Fig. 11.11).
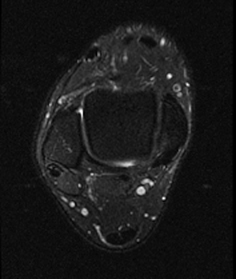
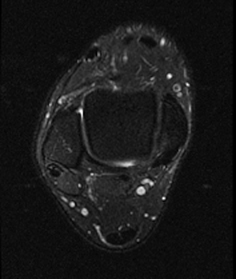
Fig. 11.11
Axial T2 MRI—peroneus brevis tear
Unfortunately, preventative strategies for peroneal tendon injuries are limited. Careful clinical screening and treatments focusing on the prevention of further ankle instability are the hallmarks of treatment for peroneal tendon pathology, particularly with a previous history of ankle sprain or specific underlying disease (Figs. 11.12 and 11.13).
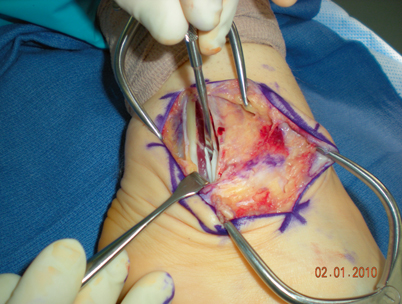
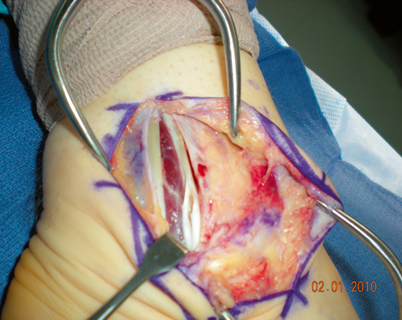
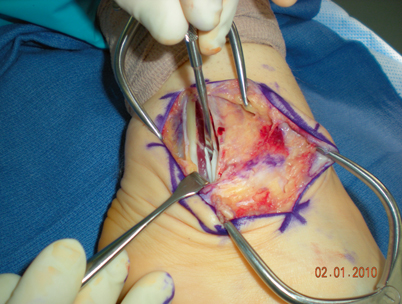
Fig. 11.12
Lateral ankle intraoperative image—longitudinal peroneus brevis tear
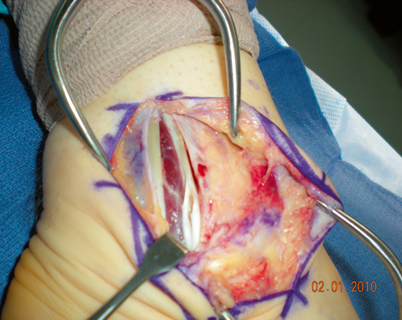
Fig. 11.13
Lateral ankle intraoperative image—longitudinal peroneus brevis tear
Foot
Achilles Disorders
The gastrocnemius–soleus complex serves as a powerful plantarflexor of the ankle and provides a pivotal link to the normal gait cycle through the Achilles tendon. Given its critical importance and peak forces up to 12.5 times body weight, the Achilles tendon is often subject to several inflammatory, degenerative, and traumatic conditions, particularly with age and cumulative activity [109].
With age and repetitive loading, the microscopic architecture of the Achilles tendon undergoes characteristic changes (Fig. 11.14). The collagen fibril diameter and density decrease while becoming increasingly disorganized and disoriented. Additionally, intrasubstance degeneration occurs with microtears, focal necrosis, calcification, and a relative absence of neovascularization indicative of tendinosis at the calcaneal attachment (insertional) or more proximally (non-insertional). Alternatively, tendonitis implies an underlying inflammation and is frequently a misnomer for tendinosis on histopathological analysis. Paratenonitis is an inflammatory entity that arises from mechanical irritation and manifests as edema, increased vascular response, and perivascular infiltration of inflammatory cells. Lastly, Achilles ruptures typically occur in the watershed area of limited vascularization and often vis-à-vis preexisting tendinosis .


Fig. 11.14
Palpable Achilles tendon defect
Epidemiology
Achilles injuries are prevalent among active cohorts, particularly with running and competitive athletes, and by extension, military service members. Conservative estimates place the incidence rate of Achilles ruptures as 7 injuries per 100,000 in the general population, with increases up to 12 per 100,000 when isolating competitive athletes [110]. Although not infrequent, the epidemiology of Achilles ruptures is not completely borne out given the difficulty in quantifying a population at risk. However, certain risk factors have been articulated, including advancing age [111], male gender [112], athletic participation, involvement in selected sports (e.g., basketball) [113, 114], marked changes in training or physical activity [115], preexisting tendinopathy, steroid [116, 117] and fluoroquinolone use [118, 119], and underlying baseline comorbidities. Raikin et al. [113] conducted a descriptive epidemiological study of 406 Achilles tendon ruptures presenting to a tertiary referral setting in the USA. The patient population was middle-aged (mean, 46.4 years), male (83 %), and involved in sporting activity (68 %); basketball (48 %) and tennis (13 %) were the most commonly involved sports in related ruptures. The incidence rate among military service members is approximately 0.24 % [120]. Participation in basketball has resulted in the predominance of acute Achilles ruptures, particularly among African-Americans. In their study over a 3-year time period, Davis and colleagues [114] identified that individuals of the black race were at nearly a twofold higher risk (1.82; 95 % CI, 1.58, 2.10) of Achilles rupture than non-black patients .
Overuse Achilles injuries, including paratenonitis and symptomatic tendinopathy, are more prevalent. Both can occur with recreational or competitive athletics, although there appears to be a stronger association with endurance running. In a retrospective study of Achilles injuries, approximately 53 % of athletes were active runners at the time of injury, while an additional 27 % were involved in running sports. Of all injuries, 66 % of individuals had paratenonitis and 23 % had insertional tendinopathy. Achilles paratenonitis and symptomatic tendinopathy occur largely as a result of training errors or changes in distance, intensity, terrain, technique, or fitness. Whereas some risk factors such as misalignment, limb length inequality, and muscle imbalance or weakness are non-modifiable, other risk factors may be targets for intervention, including heel running, training surfaces, environmental conditions (e.g., wet, slippery, or uneven surfaces), footwear, and equipment [121].
Numerous approaches to conservative treatment have been postulated, although few other than an Achilles stretching and strengthening regimen have demonstrated consistent success. This preserves the mobility and function of the normal ankle and Achilles tendon, while decreasing strain. Mafi et al. [122] and Silbernagel et al. [123] demonstrated significant improvements with an eccentric, load-bearing training protocol, particularly with non-insertional tendinopathy. However, other authors have demonstrated moderate success with a limited-dorsiflexion, eccentric program in patients with insertional Achilles tendinosis as well [124].
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







