Lower Extremity Surgery in Children With Cerebral Palsy
Introduction
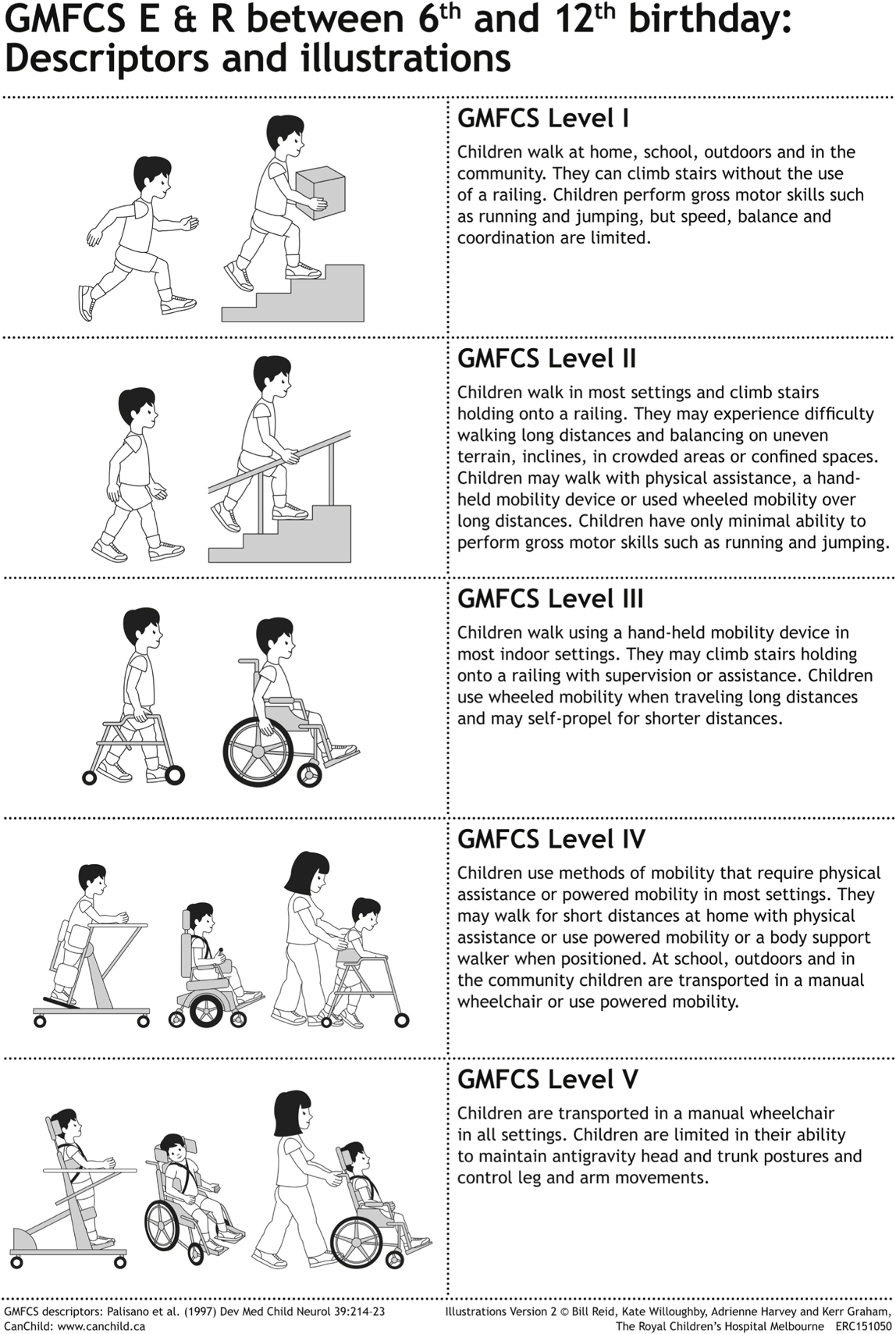
Figure 1Illustration of the Gross Motor Function Classification System (GMFCS) for cerebral palsy. Levels I through III (ambulatory). Levels IV and V (nonambulatory). E & R = expanded and revised.
(© Kerr Graham, Bill Reid, and Adrienne Harvey, The Royal Children’s Hospital, Melbourne, Australia. Data from Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B : Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol1997;39[4]:214-223 and data from CanChild Centre for Childhood Disability Research Institute for Applied Health Sciences, Ontario, Canada.)
Cerebral palsy (CP) is an abnormality of motor function resulting from insult to the brain during early development
Brain injury is considered static; musculoskeletal manifestations are progressive
Delay surgery until the patient is at least 6 years old; spasticity management is important adjunct
For multiple deformities, single-event multilevel surgery is recommended to prevent decompensation from unbalanced correction
Gross Motor Function Classification System (GMFCS) categorizes patients with CP based on function (Figure 1)
Functional Mobility Scale (FMS) rates ambulatory function at 5, 50, 500 m
Classification is important because surgery goals vary depending on whether the patient is ambulatory (GMFCS I through III) or nonambulatory (GMFCS IV and V)
Ambulatory Patients
TABLE 1
Typical Abnormalities and Potential Surgical Options in Ambulatory Patients With Cerebral Palsy
| Abnormality | Potential Surgical Treatments |
| Hip adduction contracture | Adductor tenotomy |
| Hip flexion contracture | Psoas release at pelvic brim |
| Knee flexion contracture | Distal hamstring lengthening |
| Distal femoral extension osteotomy with patellar tendon advancement | |
| Knee recurvatum | Ankle plantar flexor lengthening |
| Stiff-knee gait | Rectus femoris transfer |
| Equinus contracture | Ankle plantar flexor lengthening |
| Equinovarus deformity of the foot | Posterior tibialis lengthening, split posterior tibial tendon transfer, split anterior tibialis transfer, ankle plantar flexor lengthening |
| Pes planovalgus deformity | Peroneus brevis lengthening, calcaneal lengthening osteotomy (±cuneiform osteotomy), calcaneal sliding osteotomy (±cuboid and cuneiform osteotomy), subtalar arthrodesis, triple arthrodesis |
Surgeon must understand gait abnormalities to identify correct treatment and procedure
May be assessed via observational or instrumented gait analysis
Common abnormal gait patterns include scissoring gait, crouch gait, jump gait, stiff-knee gait, recurvatum gait
At the foot and ankle, patterns include pure equinus, equinovarus, pes planovalgus
Rotational abnormalities also may be present and need to be addressed; children with CP often cannot compensate for lever-arm dysfunction
Surgical options for ambulatory CP patients are listed in Table 1; before selecting one or more options, the surgeon must consider:
Gait abnormality
Soft-tissue, bony rotational issues causing dysfunction
Appropriate procedure to correct gait based on contractures/imbalances
Rotational components, which should be treated more aggressively in patients with CP than in typically developing children
Nonambulatory Patients
Hip subluxations, dislocations can cause sitting issues and can exacerbate scoliosis
Address this problem with combination of procedures, including proximal adductor, hamstring, psoas lengthenings; open reduction with capsulorrhaphy of hip (>50% subluxation); pericapsular pelvic osteotomy; femoral varus derotational osteotomy (VDRO)
Manage knee flexion contractures with hamstring lengthenings
Manage foot, ankle issues with surgeries similar to those used for ambulatory patients
Soft-Tissue Lengthening Procedures
Adductor Lengthening
Indications
Scissoring gait
Spastic hip subluxation/dislocation
Preoperative Imaging
Usually not required in isolation
When part of hip reconstruction, obtain AP, frog-leg lateral views of pelvis, bilateral hips; possibly CT with three-dimensional reconstructions
Surgical Technique
Supine position
Make transverse incision one fingerbreadth distal to groin crease
Incise fascia overlying adductor longus tendon in line with its fibers
Isolate adductor longus with right-angle clamp and cut as proximally as possible with electrocautery
Transect gracilis muscle similarly if limited abduction present with hip in extension
If still further abduction required, transect adductor brevis until 45° of abduction is achieved; identify and preserve the anterior branch of obturator nerve lying across this muscle
Close wound in layers
Complications
Hematoma formation
Inadvertent transection of obturator nerve branches
Postoperative Care and Rehabilitation
Place in Petrie casts with abduction bar for 4 weeks
Abduction brace may be worn instead; maintained at night for 6 months
Pearls
Do not extend the incision beyond the lateral border of the adductor longus tendon to avoid the femoral neurovascular bundle.
Distal Hamstring Lengthening
Indications
Crouch gait, jump gait, knee flexion contractures
Patient should have popliteal angle greater than 40° and posterior pelvic tilt;
Risk of worsening gait if performed in patients with anterior pelvic tilt
Surgical Technique
Prone position if performed as isolated procedure, with single midline incision
Supine position when performed with other surgeries via two-incision technique (medial and lateral)
Start incisions slightly anterior to hamstring tendons, 1 to 2 cm proximal to knee joint and extend proximally 5 to 7 cm
Medial Hamstrings
Dissection taken posterior to sartorius muscle to open fascia overlying gracilis
Section tendon of gracilis over muscle belly with electrocautery or knife
Identify semitendinosus tendon; section through fascia overlying muscle or perform Z-lengthening if more length needed
Semimembranosus muscle is deep, broad; can section its fascia once or twice as needed
Avoid injuring sciatic nerve by excessively stretching knee into extension
Lateral Hamstrings
Rarely indicated
Approach anterior to biceps to protect peroneal nerve
Transect tendon overlying biceps muscle belly
Complications
Sciatic nerve stretch or transection
Sciatic nerve palsy
Postoperative Care and Rehabilitation
Place in knee immobilizer for 4 weeks, and then begin stretching program
Carefully monitor sciatic nerve postoperatively
Lengthening of the Gastrocnemius-Soleus
Indications
Equinus contracture, jump gait, recurvatum gait
In the vast majority of children with diplegia, only the gastrocnemius is lengthened; in hemiplegia, both muscles are lengthened
Discourage Z-lengthenings of the Achilles tendon; risk of overlengthening, weakens muscles
Surgical Technique
Supine position
Make incision medially in middle third of calf
Identify sural nerve, lesser saphenous vein; isolate and protect them
Open fascia and lengthen tendon overlying muscles from medial to lateral under direct visualization, taking care to preserve muscle underneath
Perform gentle dorsiflexion after completing transection
Complications
Rupture of Achilles tendon
Sural nerve injury
Overlengthening
Postoperative Care and Rehabilitation
Short-leg walking cast with foot in neutral for 4 to 6 weeks
Transition to ankle-foot orthosis (AFO)
Pearls
Do not overlengthen.
The incision can be made medially or laterally, depending on the need to lengthen other tendons, such as the tibialis posterior and peroneus brevis, respectively.
Peroneus Brevis Lengthening
Indicated for pes planovalgus
Can perform with gastrocnemius-soleus lengthening through single lateral incision
Obtain weight-bearing foot radiographs as part of larger procedure
Surgical Technique
Supine position
Make posterolateral incision over distal third of fibula, approaching posteriorly to protect superficial peroneal nerve
Open sheath; identify peroneus longus tendon lateral to peroneus brevis tendon, which has muscle belly at this level
Protect peroneus longus; transect peroneus brevis tendon over belly, with distraction provided by inverting foot
Complications and Postoperative Care and Rehabilitation
Primary complication is superficial nerve injury
Rarely performed in isolation; postoperative care depends on larger procedure
Pearl
Can be performed concomitantly with gastrocnemius-soleus lengthening through lateral incision.
Posterior Tibial Tendon Lengthening
Indication and Surgical Technique
Indicated for equinovarus
Supine position with bump under hip
Make 3-cm incision medially at the junction of the middle and distal thirds of the leg
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


