Lower Extremity Nerve Entrapments
Evan Peck
Jay Smith
INTRODUCTION
Neurologic conditions account for 10-15% of all exercise-induced leg pain among runners (15,79,82,88). Causes include contusion, compression, stretching, and iatrogenic injury (3,5,6,78,79,80). The interdigital (interdigital or Morton neuroma), lateral plantar (LPN), medial plantar (MPN), tibial (TN), peroneal (common [CPN], deep [DPN], and/or superficial [SPN]), sural (SN), or saphenous nerves may be affected (79).
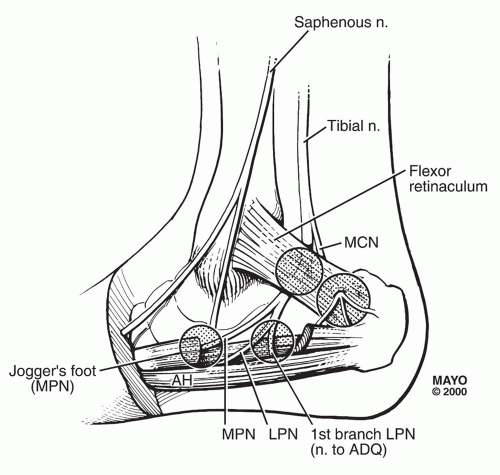
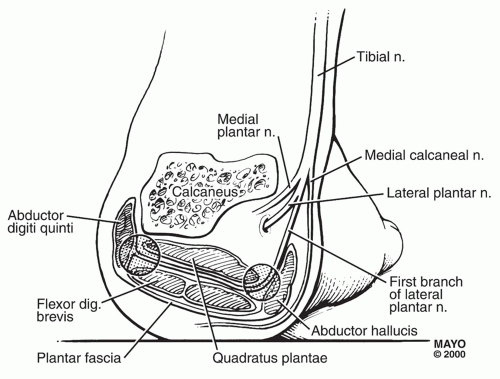
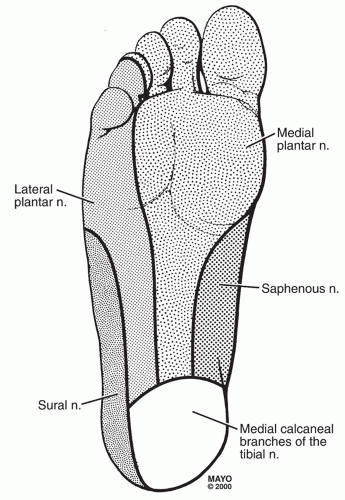
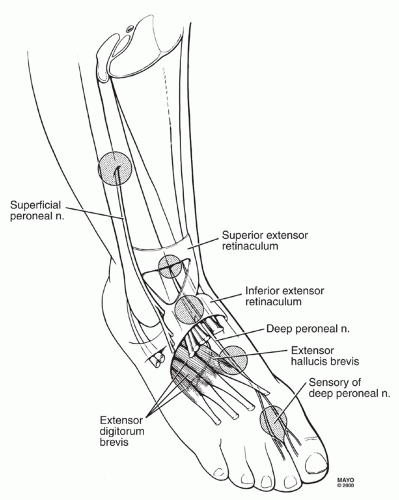
Figures 68.1, 68.2, 68.3, 68.4, 68.5, 68.6 and 68.7 show the relevant neuroanatomy, including as it pertains to entrapment sites.
Table 68.1 outlines the anatomic relationship among the lower limb nerves.
COMMON NERVE ENTRAPMENT SYNDROMES
Interdigital Neuroma (Morton Neuroma)
Anatomy, Pathophysiology, and Risk Factors
During push-off, forceful toe dorsiflexion compresses and stretches the interdigital nerve across the dorsal intermetatarsal ligament, resulting in demyelination, scarring, and hypertrophy (5).
Others suggest that Morton neuromas result from the pressure of the metatarsal heads and metatarsophalangeal (MTP) joints (41).
Risk factors: prolonged running, squatting, high-heeled or narrow toe-boxed shoes, or demi-pointe in ballet (98).
Hyperpronation dorsiflexes the third metatarsal relative to the fourth, exposing the nerve to injury during push-off (79).
Idiopathic MTP synovitis may cause local edema and interdigital nerve compression (78).
Symptoms and Signs
Tenderness in affected intermetatarsal space; neuropathic pain, typically between the third and fourth toes, increased with running, standing, walking, toe dorsiflexion, and squatting.
Provocative testing: pressure over plantar aspect of the web space between the metatarsal heads, or squeezing metatarsals together during palpation. The squeeze test may also result in a click (“Mulder click”) as the neuroma subluxates from between the metatarsals in a plantar direction (79).
Differential Diagnosis and Evaluation
Differential diagnosis includes proximal and systemic neurologic conditions, stress fractures, MTP joint synovitis or arthritis, and flexor tenosynovitis.
Diagnostic interdigital nerve block is confirmatory.
Diagnostic ultrasound (US) can be used for diagnosis or to guide therapeutic injection (34,36,70,83).
Magnetic resonance imaging (MRI) and US have comparable detection rates for evaluation of Morton neuroma (45).
Treatment
Activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), footwear modifications, physical therapy, and biomechanical interventions to reduce toe dorsiflexion, control hyperpronation, and maintain greater metatarsal separation.
Corticosteroids have been used with good results in some cases (52).
Sonographically guided alcohol ablation of the neuroma may be used (36). One study reported resolution of pain in 80.3% of cases at a mean follow-up of 36 months (50).
Surgery is generally indicated when diagnosis is firm and symptoms refractory. One study noted that 76% of cases were asymptomatic at a minimum of 2 years postoperatively after surgical resection (22). Minimally invasive techniques have also been described, with similarly favorable outcomes reported in one small study (100).
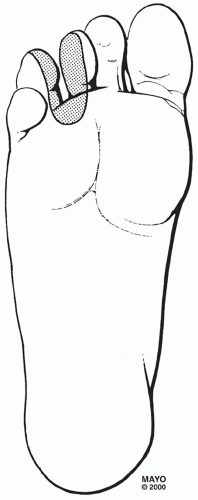
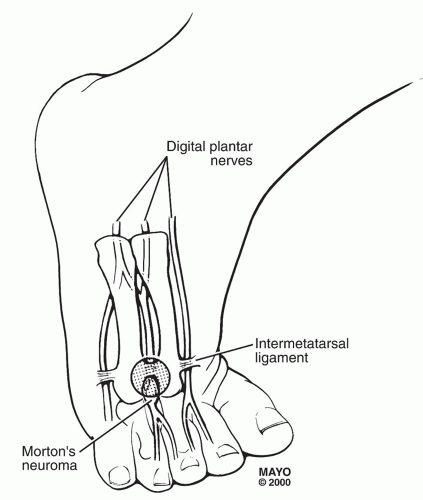 FIGURE 68.2: Interdigital neuroma in the third intermetatarsal space. By permission of Mayo Foundation for Medical Education and Research. All rights reserved. |
Tibial Nerve (TN): Tarsal Tunnel Syndrome (TTS)
Definition
TN entrapment most commonly occurs at the level of the tarsal tunnel (Fig. 68.3) (82). There is a slight (56%) female predilection (43). TN entrapment may also occur at the level of the medial gastrocnemius (high TTS), under the fibromuscular arch of the soleus, or as a result of popliteus muscle tear (5,6,19,24,67,78,79).
Anatomy, Pathophysiology, and Risk Factors
The TN originates from the L4 to S3 spinal segments and is the larger terminal branch of the sciatic nerve (52). The tarsal tunnel is a fibro-osseous space formed by the flexor retinaculum, medial calcaneus, posterior talus, distal tibia, and medial malleolus, and extends from the distal tibia to the navicular bone. Over 90% of the time, the TN will divide into the MPN and LPN within the tarsal tunnel (43). Within 1-2 cm below the medial malleolar-calcaneal line, the MPN and LPN enter separate fibro-osseous canals at the origin of the abductor hallucis muscle (AHM) (62,79). At this point, the LPN may be particularly vulnerable to injury (43).
Etiologies include trauma, compression by space-occupying lesions (e.g., venous varicosities, ganglion, neurilemmoma, tenosynovitis, os trigonum, bone fragments, tumors, or accessory muscles), systemic disease, and biomechanical factors (38,55,58,59,62,64,65,69,77,87,99). Hyperpronation increases AHM tension and may entrap the TN or plantar nerves (43). Eversion and inversion of the foot and ankle have been shown to decrease tarsal tunnel compartment volume (9). A specific cause is identified in only 60%-80% of cases (43).
Symptoms and Signs
Symptoms include cramping, burning, and tingling at the medial ankle, medial foot, and/or plantar foot. The medial heel is usually spared because of the proximal origin of the MCN (43). Symptoms increase with activity. Running on a banked surface promotes hyperpronation and may aggravate symptoms (52). Resting and night pain may occur in provocative positions, and shaking the foot or walking may provide relief, similar to carpal tunnel syndrome (78,79).
Examination includes inspection for malalignment, deformity, or muscular atrophy causing or resulting from TTS, such as forefoot pronation, claw toe, talipes calcaneus, or calcaneovalgus. Percussion testing is completed over the TN and all its terminal branches; a Valleix phenomenon (proximal radiation from the site of entrapment) may be elicited (21). Provocative maneuvers include sustained passive eversion or great toe dorsiflexion, and postexercise examination.
In severe cases, weakness of toe plantarflexion manifests by reduced push-off on the affected side (52).
Differential Diagnosis and Evaluation
Differential diagnosis includes polyneuropathy, proximal or distal neuropathy, deep posterior compartment syndrome, popliteal artery entrapment, vascular claudication, venous disease, tenosynovitis, ganglia, plantar fasciitis, tibiotalar or subtalar synovitis, accessory muscles, and osseous compression (76,93).
TN injury just distal to the SN contribution spares lateral calcaneal and foot sensation and gastrocnemius-soleus function. Injury distal to the midportion of the leg affects plantar
sensation and results in claw toe deformity caused by imbalance between the affected foot intrinsic muscles and the unaffected flexor digitorum longus (FDL) and extensor digitorum brevis (EDB) muscles (52).
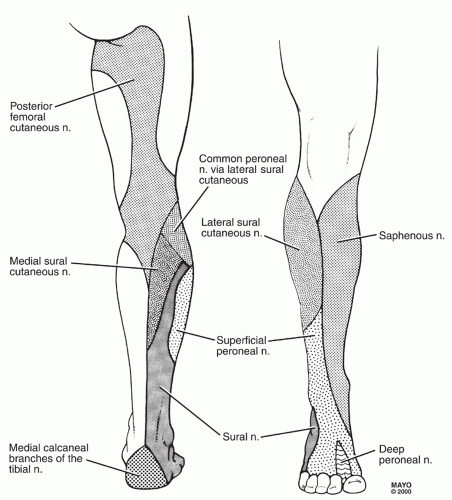
FIGURE 68.7: Cutaneous innervation of the thigh, leg, and dorsal surface of the foot. By permission of Mayo Foundation for Medical Education and Research. All rights reserved.
Table 68.1 Neuroanatomy of the Lower Limb
Sciatic nerve (L4-S3 spinal segments)
Tibial nerve (TN)
Medial sural cutaneous nerve (MSCN)
Medial calcaneal nerve (MCN)1
Medial plantar nerve (MPN)
Contribution to third interdigital nerve
Medial hallucal nerve
Lateral plantar nerve (LPN)
First branch of LPN (FB-LPN)2
Contribution to third interdigital nerve
Common peroneal nerve (CPN)
Lateral sural cutaneous nerve (LSCN)
Superficial peroneal nerve (SPN)
Deep peroneal nerve (DPN)
Femoral nerve (FN; L2-4 spinal segments)
Saphenous nerve
Lateral femoral cutaneous nerve (LFCN; L2-3 spinal segments)
Obturator nerve (ON; L2-4 spinal segments)
1 May arise from the LPN or from the bifurcation of the LPN and MPN.
2 May arise directly from the TN.
Night pain, proximal radiation, and lack of pain during the first steps in the morning help differentiate TTS from plantar fasciitis (39).
MRI is effective for examining the tarsal tunnel and reveals an inflammatory lesion or mass in up to 88% of patients with a firm clinical diagnosis of TTS (27). Diagnostic US can also effectively visualize structures within the tarsal tunnel and accurately identify compressive mass lesions and/or focal changes in TN cross-sectional area (2,59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree