Fig. 3.1
The polycentric total knee arthroplasty is shown
The first metal backed tibial component with modular polyethylene inserts was designed and implanted by Nas Eftekhar at the New York Orthopaedic Hospital in 1969 [5]. It was suggested that metal backing and accurate articular geometry would permit the use of thinner polyethylene inserts. Implants were fixed with cement, but it was the use of long intramedullary stems which would secure fixation. This knee design (Eftekhar Mark I) would evolve into a condylar total knee design (Eftekhar Mark II) (Fig. 3.2). Early in the 1970s, Coventry (Mayo Clinic), Riley (Johns Hopkins), Finerman (UCLA), Turner (Harvard) and Upshaw (Corpus Christi) introduced the first geometric knee arthroplasty (Geomedic or Geometric I Knee) [6]. This design was based on Bob Averill’s idea of creating a conforming device which allowed preservation of both cruciate ligaments. The femoral components were made of chromium and cobalt and joined together with a narrow metal bar, while the polyethylene tibial insert had three small pegs to improve fixation. The patella was not replaced and both cruciates were preserved (Fig. 3.3). It was designed in order to reduce stresses using a conforming geometry of the femoral and tibial components, but this implant also eventually failed due to rapid and excessive loosening.
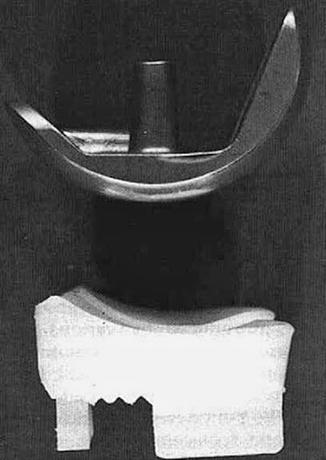
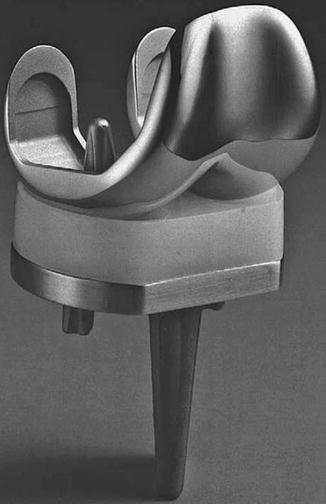
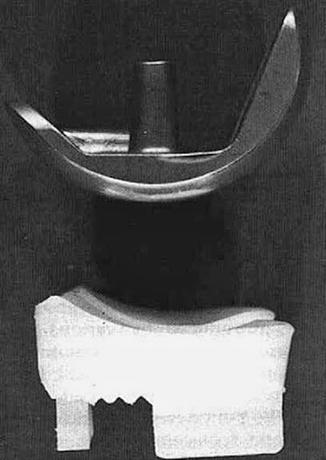
Fig. 3.2
The geometric total knee arthroplasty is shown
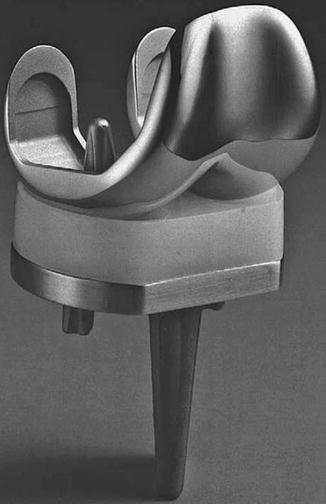
Fig. 3.3
The Eftekhar Mark II total knee arthroplasty is shown
The next step in the evolution of this implant was the Geometric II knee. In 1975, Zimmer presented two similar geometric knees. In the first, a tibial peg was added in order to improve fixation (Geotibial knee) and in the second, a femoral flange was used in order to improve patellar tracking (Geopatellar knee). Both designs had an increased sagittal radius of curvature of the tibial polyethylene liner in order to increase constraint. Further designs emerged from these implants – the Multi-Radius, Miller Galante, Miller Galante II, and Nexgen knees. In the same year, Howmedica presented a similar but more anatomical design, the Anametric knee, which would evolve into the porous-coated anatomical knee (PCA) and eventually the Duracon knee.
During the same period, several hinged prostheses were developed, like the Sheehan prosthesis, the Attenborough prosthesis and the most popular Guepar total knee replacement (Fig. 3.4). Despite the initial enthusiasm, however, these prostheses failed because of a high rate of patellofemoral complications, breakage of the implant, early wear and loss of fixation. Nowadays, hinged and rotating hinge arthroplasties are only used in revision and tumour cases.


Fig. 3.4
The Guepar hinge total knee arthroplasty is shown
Outcomes of First Knee Replacements and Evidence-Based Data
The literature is relatively poor regarding the outcomes of first generation knee arthroplasties. An early publication describing a polycentric knee design Scolnick et al. [7] presented satisfactory outcomes of a unicompartmental polycentric knee arthroplasty, but follow-up was only 1 year and it is difficult to draw reliable conclusions. However, the authors supported the use of unicompartmental geometric implants and defined the indications for their use (one compartment osteoarthritis, osteoarthritis unsuitable for valgus upper tibial osteotomy, osteoarthritis after condylar fracture and necrosis and failed prior high tibia osteotomy). Similar results were presented by Jones et al. [8] (a series with unicompartmental polycentric and geometric designs). Follow up was longer (2.6 years), but again too short to be reliable. The main causes of failure in this series were loosening of the tibial implant and unexplained pain. The proposed indications for use were the same as Scolnick et al. and the authors suggest that adequate knee movement and increased levels of independence and activity could be achieved with these implants. Gunston himself presented the results of 89 polycentric knee arthroplasties with 2–7 years follow up [9]. The majority of patients had an improvement in function and mobility, but loosening rates of the prosthetic components were also high (10 %). Bryan and Petersen [10] reported a prognostic assessment of polycentric knees with a 5–7 years follow up. Outcomes were better in the patients with rheumatoid rather than degenerative arthritis and failures occurred due to infection, loosening of the tibial component, dislocation, instability and progression of patellofemoral arthritis. The authors emphasized the need for improving surgical techniques and using more durable and non constrained implants. Probably one of the biggest series with polycentric knee replacements and the longest follow-up was that published by Lewallen et al. [11]. Although the study was retrospective, important conclusions could be made regarding outcomes and complications. The failure rate in this series proved to be high (34 %), with the main causes being instability, loosening, infection and patellofemoral joint pain. According to this study, proper axial alignment was a critical factor in the reduction of complication rates.
Tietjens and Cullen [12] presented the preliminary results of the geometric TKA in 1975. Results were encouraging, but the population sample was small and the follow up short. Three years later, Riley and Hungerford [13] reported the results of 54 geometric knees with a longer follow up (24–64 months). All patients had rheumatoid arthritis and the improvement of pain symptoms and mobility was significant. Patellar pain, flexion contracture and tibial loosening were the causes of the three cases of revision. Finerman et al. [14] reported their early experience with the Geometric II knee. They called it the anametric knee because it was designed to mimic the anatomy of the normal knee. Improvements in pain symptoms and function were attributed to the addition of further sizes and tibial fixation options. An interesting comparative study by Wilson et al. [15] showed no differences in midterm outcomes and revision rates between the Walldius and geometric knee prostheses. Attention to surgical procedures and reduction of technical errors were emphasized by the authors in order to avoid complications. Lowe and McNeur [16] reported a comparative study of Geometric TKA used in two groups of patients with different diagnoses. Patients with rheumatoid and those with degenerative arthritis had similar levels of satisfaction, although more rheumatoid arthritis patients considered their results disappointing. The revision rate was 5 % and the main causes were instability or loosening. In contrast, Hunter et al. [17] supported the use of geometric designs in patients with rheumatoid arthritis demonstrating its benefits in pain relief, good function and low risk of patellofemoral problems. He also recognized that these immunocompromised patients were at risk of developing late infection. Imbert and Caltran [18] analysed the results of 63 first generation Geometric arthroplasties with a follow up of more than 5 years. They reported an increased rate of complications, mainly loosening and infection. Coventry and Rand [19] also showed similar complication (12 %) and revision rates (20 %) with the use of this implant. All their patients had osteoarthritis and one third of them experienced implant loosening. The 10 year survival of the prosthesis was 69 % with revision or moderate to severe pain as an end point. Eftekhar [5] presented the midterm results of his knee design (4–9 years follow up) in 1983. Although one third of the patients showed evidence of a non progressive radiolucent lines around the tibial component, functional outcome was very satisfactory. Only 2 out of 112 patients had a revision for loosening and deep infection was the major complication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






