Fig. 11.1
Minimal but adequate knee exposure is shown
The concept of MIS generally involves: (1) smaller incisions of approximately 10–13 cm; (2) patella dislocation without eversion (Fig. 11.2); (3) minimal dissection of the quadriceps tendon; (4) preservation of the suprapatellar pouch; (5) utilization of specifically designed MIS instrument trays of reduced size (Fig. 11.3); and (6) performing the operation through a mobile soft tissue window with the appropriate use of retractors [31–33].

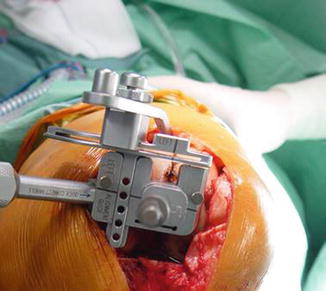

Fig. 11.2
Lateral displacement but not eversion of the patella is shown
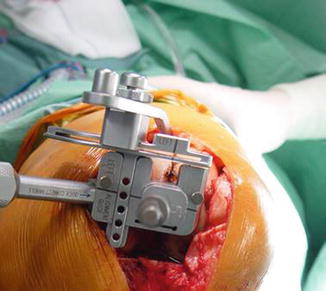
Fig. 11.3
Specially designed small instruments are necessary
Based on these principles, five surgical approaches have been described, which are: the mini medial parapatellar, quadriceps-sparing, mini-midvastus, mini-subvastus, and the direct lateral approach [34]. It is not the goal of this chapter to extensively describe the technical details of each approach but it should be noted that they are basically variations of ways of handling the quadriceps tendon (Fig. 11.4).
Fig. 11.4
A variety of popular MIS approaches is shown
The Various MIS Approaches
Some attempts have been made to compare effectiveness and safety among MIS approaches. Niki et al. [35] tested the lateral MIS approach in 26 valgus knees and found results comparable to medial MIS approaches in terms of clinical scores, postoperative pain, radiographic alignment and rates of complications. The fact, though, that a 1 cm snip of vastus lateralis had to be performed in five of their cases is indicative of the technical difficulties and the obstructed visibility of this approach. Lee et al. [36] report in their RCT that the mini midvastus and mini medial parapatellar (MMP) approaches gave comparable results in terms of pain, clinical scores and radiologic outcome in navigation assisted TKA’s. Acknowledging the technical difficulties of MIS techniques, these authors favour the MMP approach because it is easier to convert to the conventional approach when necessary. After reviewing a total of 23 level I or II studies, Costa et al. [37] conclude that the lateral MIS approach had the highest rates of complications. The mini-midvastus had the best clinical results at 1 and 3 months postoperatively and the mini-subvastus had the lowest rate of complications.
Lin et al. [38] compares the quadriceps sparing approach (QS) with the mini medial parapatellar in their RCT and found that QS-TKA had more radiological outliers and longer operating times compared with the MMP approach even after adequate learning curve and with appropriately selected patients.
Based on this evidence and our personal experience we believe that for those surgeons who wish to perform an MIS-TKR, either the mini-midvastus or the mini-subvastus approach can most reasonably be expected to offer the proposed advantages of MIS, i.e. better short term clinical results without complications. These approaches have consistently shown good results with minimal complication rates. They are technically easier to perform compared to the QS and mini lateral approaches and they offer better intraoperative visibility. They are also easily extended to conventional approaches should the circumstances require. The mini lateral approach is an option for valgus knees but the surgeon should have gained extensive personal experience with the MIS conceptualization of TKA before deciding to proceed with MIS techniques in valgus knees.
MIS and Conventional Techniques
To date there have been more than 50 RCT’s and approximately 16 systematic reviews and met-analyses investigating the difference between MIS and conventional approaches in TKA. From an overview of the literature we can see that up to now the majority of level I and II evidence reports short term results with follow up of 2–3 years. There is also significant heterogeneity between the studies because of the different MIS approaches, component choice or patient demographics.
Research during the past 10 years has focused on the investigation of the clinical efficiency of MIS techniques, the radiological alignment of the components and safety. Clinical efficiency was measured using clinical outcome scores, range of motion (ROM), the straight leg raise test (SLR), quadriceps strength, postoperative pain, and length of hospital stay. Radiological alignment was measured with alignment on the coronal plane and the rates of outliers. Safety was measured using blood loss, complication rates and revisions.
Clinical Scores
Costa et al. [37] reviewed 23 level I and II studies and found no significant difference in clinical scores between MIS and conventional techniques. In Li et al.’s [39] meta-analysis MIS-TKA has shown significantly improved results in objective and subjective outcome scores, VAS, ROM, knee flexion, flexion 90 day and straight leg rising day, all of which resulted in patients achieving faster recovery. In another study [40] results were analysed for measurements available at 6 weeks, 3 months and 6 months or more. The objective score at 3 months was just marginally significant in favour of the MIS group. In the same study the (VAS) was significantly improved in the MIS group.
Range of Motion
ROM is an important parameter of functional outcome. In control cohort studies, the MIS approach was found to be superior to the conventional approach in terms of ROM [41, 42]. Alcelic et al. [40] evaluated 507 MIS versus 513 conventional TKAs in a metanalysis. Knee flexion was significantly greater by 9.9° on average in the MIS group at 1 week postoperatively but not at 3 months.
Pain
Postoperative pain is an important parameter in terms of patient satisfaction and also greatly affects postoperative rehabilitation. Recently published meta-analyses report better results in VAS scores and postoperative pain [39, 40]. In our RCT [23] we report that during the first post-operative week pain was apparently greater in the minimally invasive group. In our opinion, pain management is a serious confounding factor in many published studies, and reduced pain levels should not be presented as a benefit of minimally-invasive TKA (Fig. 11.5).


Fig. 11.5
Immediate postoperative straight leg raising, due (in our opinion) to patient controlled epidural anaesthesia
Quadriceps Muscle Strength
The difficulty of consistently showing a definite clinical advantage of MIS techniques has led investigators to try to measure clinical outcome by other means. Bonutti et al. [43] used the contralateral knee as a control group and found that peak extensor muscle strength was significantly and consistently higher in the MIS group. Most patients preferred the knee treated with the MIS approach. Interestingly, these patients had different objective Knee Society Scores but similar Knee Function Scores. The authors conclude that this measure may not be sensitive enough to detect the improved outcomes of MIS techniques which are detectable with more specific measures, such as isokinetic muscle strength testing, ambulation and straight leg-raising time.
Costa et al. [37] concludes, in a systematic review, that the only significant difference observed was in the recovery of quadriceps muscle function (shorter in patients who had undergone a minimally invasive approach).
Alcelic et al. [40] also found a significant reduction in number of days to SLR in the MIS group.
Blood Loss
Radiographic Alignment
Despite initial reservations, the fear of implant malposition does not seem to be confirmed. Most of the meta-analyses [37, 39, 44] did not find inferior radiological results in terms of component orientation and outliers with MIS techniques. Bonutti et al. [45] reviewed their first 1,000 MIS TKAs and their most important radiologic finding were 3 impending component failures, 2 tibial and 1 femoral. They raise the concern of potential tibial component loosening related to decreased exposure and possibly poor cement pressurization. In another study by there were more cement voids and more retained cement debris in the minimally invasive cohort. In our study a high incidence of wrong implant placement was found and we argue that femoral component malrotation is not detected by conventional radiography [23].
Complications
Costa et al. [37], after reviewing a total of 23 level I or II studies, conclude that there were no differences in complication rates between patients with various minimally invasive approaches compared with a standard approach. The minimally invasive lateral approach had more complications than the other minimally invasive approaches. Alcelic et al. [40], in a systematic review and metanalysis, analyzed four RCTs and quasi RCTs with a total of 296 MIS TKAs for complications. They did not find an increased risk of wound healing problems but MIS techniques showed a significantly increased risk of developing intraoperative complications with a risk ratio (RR) of 7.6. The most common complication was quadriceps tendon laceration (31 cases) and anterior femoral notching (5 cases). Other reported complications were patellar tendon rupture or partial avulsion (four cases), laceration of the popliteus (two cases), palsy of the deep peroneal nerve (two cases), one medial epicondylar avulsion fracture, one femoral condylar fracture, one tibial plateau fracture, one supracondylar fracture and the inability to displace the patella or achieve adequate exposure in four cases in the MIS group requiring conversion to the standard approach. This finding, in our opinion, reflects the technical difficulties that surgeons encounter when performing MIS techniques.
On the contrary, Li et al. [39] discovered significant differences in superficial wound healing problems and a risk of increased skin necrosis with MIS techniques but not in superficial wound infection, deep infection, DVT, fractures, femoral notching, peroneal nerve palsy, stiffness requiring manipulation, polities tendon injury, or knee instability. However, we do not feel that superficial wound problems, which are usually easily treated, should be regarded as severe complications.
Operative Time
MIS techniques are associated with longer operative and tourniquet times, especially during the learning curve period [40], but there are studies indicating that these parameters reduce to levels comparable with conventional techniques as experience is accumulated by the surgical team [24].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







