Fig. 16.1
Satisfactory clinical and radiological outcome of a cemented Genesis II TKA at 16 years follow up
Cementless fixation was developed in order to achieve a more physiological bond between implants and bone and to improve longevity of the interface, especially in young patients. It has been available for more than three decades (Figs. 16.2 and 16.3) [3, 8–12]. However, due to less than optimal outcomes with the old generation of prostheses, cementless fixation in TKA has never gained popularity [3, 11, 12]. Osteolyis is still seen and RSA studies have shown early migration of the tibial plate, which is a long term determinant of implant failure [13–15]. A critical review of initial studies has shown that early cementless implants were used in young patients with higher demands and level of activity. Aseptic loosening, more common in the young, varied between 5 and 30 % at 5 years follow up and it was associated mainly to tibial tray failure [16–20].

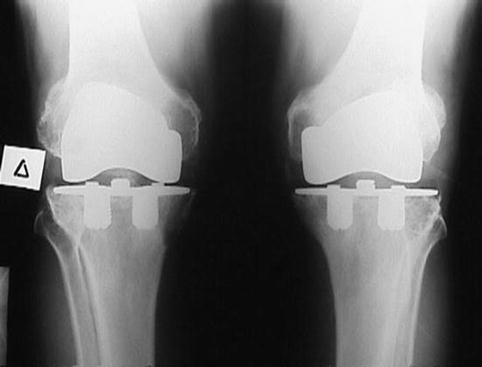

Fig. 16.2
Satisfactory clinical and radiological outcome of an cementless design at 17 years follow up
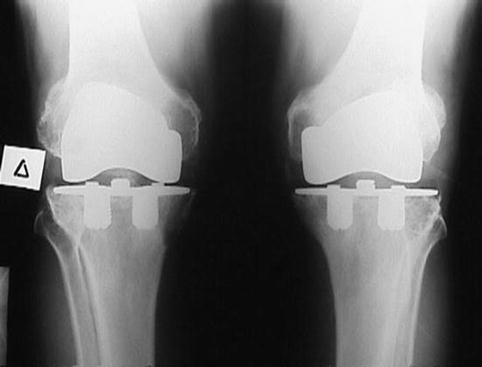
Fig. 16.3
Satisfactory clinical and radiological outcome of an early HA coated design (Goeland, Landos) at 24 years follow up
As the indication and numbers of TKA continue to increase [12], younger and more active patients are undergoing the procedure and since new technologies for cementless fixation are available [11], we present, in this chapter, a review of old and new cementless TKA clinical outcomes and we critically evaluate future perspectives.
Old Designs
Old designs were developed based on the assumption that a more physiological bond between the implant and the bone can result in improved survival from the problem of aseptic loosening, due to the ability of the interface to respond to stresses in a physiological way [11, 21]. However, the long term durability of cemented fixation has come into question in young and active patients because cement has shown poor resistance to shear and tensile forces which may result in deformation and degradation over time [3, 11, 12, 22].
A critical evaluation of old studies with cementless implants reveals that inferior outcomes were produced due to screw track osteolysis, poor old polyethylenes, metal backed patella component failures, and poor tibial tray designs implanted inappropriately in cancellous bone instead on the cortical tibial rim [3, 11, 12, 23]. It also became apparent that cementless fixation is more sensitive to component tibial tray malalignment due to abnormal concentration of loads [11, 24, 25]. Failure of ingrowth, tibial tray radioluncencies and inferior survival curves (below 90 % at 10 years) were found in several studies (Miller Galante I, PFC designs etc.) [26–29]. Other newer designs (Natural Knee, Ortholoc, LCS etc.) showed survival rates over 90 % at 10 years [30–35]. In five prospective randomised studies which evaluated cemented and cementless old designs (PFC, Interax and NexGen) no statistically significant differences were found in clinical outcome between the two versions of the components with a follow up ranging from 10 to 17 years [1, 5, 36–38]. A meta-analysis by Gandhi et al. [39] evaluated the survivorship of cemented and cementless TKA in 11 studies (5 RCTs and 10 observational). It was found that the odds ratio for failure of the implant due to aseptic loosening and the cumulative success rates were in favour of cemented fixation. However, when the five randomised studies were isolated and evaluated, no differences in survivorship were detected between cemented and cementless implants. The authors conclude that the higher failure rate of the cementless implants in the observational studies was due to the younger age and increased activity levels of the patient population of these studies. In a more recent systematic review and meta-analysis by Mont et al. [23] 37 studies were evaluated comparing cemented to cementless TKA. It was found that cementless implants had comparable survivorship to cemented. The mean survival rate was 95.6 % and 95.3 % for cementless and cemented TKA respectively at 10 years. At 20 year follow up survival rates for cementless and cemented TKA decreased to 71 % and 76 % respectively. In more recent publications, with newer designs of implant, satisfactory outcomes have been reported in mid and long terms for cementless implants [10, 40–43]. Due to the fact that in old and new observational studies nearly all the failures for aseptic loosening were related to the tibial tray component several surgeons have suggested the use of hybrid fixation in TKA with satisfactory mid and long term results [44].
In a Cochrane database report evaluating cemented, cementless or hybrid fixation options in TKA for osteoarthritis and other non-traumatic diseases, there was a smaller displacement (assessed by radiostereographic analysis) of tibial components with cemented fixation in relation to cementless fixation in studies of patients with osteoarthritis and rheumatoid arthritis who underwent primary TKA with a follow-up of 2 years; however, cemented fixation presented a greater risk of future aseptic loosening than cementless fixation [45].
Hydroxyapaptite (HA) Coated Cementless Designs
Bioactive coatings have been used in order to enhance bone ingrowth on cementless component surfaces [46–48]. It has been suggested that HA transforms fibrous tissue to bone in loaded implant–bone interfaces [49]. Radiostereometric analysis has shown that cementless components sustain greater micromotion and early migration compared to cemented components which can lead to early migration [11, 15, 50, 51, 54]. Studies of similar design have shown equal early stability of the interface between HA coated cementless and cemented implants [50, 51, 53, 54]. In a systematic review study by Voigt and Moiser [52], early implant stability was evaluated by radiostereographic analysis in three groups of patients (HA coated, porous coated and cemented). It was found that the HA coated implants without screw fixation were less likely to be unstable at 2 years compared to the porous coated and cemented implants. In observational studies with old and new HA coated implants, survival rates above 90 % have been reported between 10 and 20 years follow up [3, 11, 20, 23, 55–57]. In a prospective randomised trial, at 5 years follow up, there was no difference between cementless tibial fixation with HA and cemented tibial fixation in terms of self-reported pain, function, health-related quality of life, postoperative complications, or radiographic scores [58].
New Technologies
Recently, cementless TKA have made a comeback with newer designs, improved materials and manufacturing techniques [3, 11, 12, 23, 30, 31, 59–61]. It has been strongly suggested that the longevity of fixation depends on: joint alignment (surgical technique and instrumentation), bone quality, patient factors (age, level activity, weight), implant features (stems, pegs) and implant surface characteristics (coating, material). Additionally, factors affecting bone ingrowth or ongrowth for implant coatings are related to the structure of the material, porosity of the structure and type and size of the porous. A series of new structures have been developed, tested in animals and applied to humans: tantalum trabecular metal technology (Zimmer) [61], Tritanium dimensionised matrix (Stryker), Regenerex (Biomet), and Titanium foam (Microport-Wright Medical) (Fig. 16.4). Table 16.1 summarises the basic characteristics of these structures. Trabecular metal technology tibial tray implants were the first to be used in humans. Satisfactory clinical and radiological results have been reported from different centers with a follow up ranging from 5 to 10 years [62–64]. Fernandez-Fairen et al. [65], in a prospective randomised trial, found comparable outcomes of tantalum cementless and cemented tibial implants at 5 years follow up.


Fig. 16.4
Satisfactory clinical and radiological outcome of a titanium foam cementless advance medial pivot design at 6 years follow up
Table 16.1
Structural and material characteristics of cementless TKA surfaces in use
Coating type | CsTi | Trabecular metal | Sintered beads | Fiber mesh | Ti foam | Spongiosa metal II |
Company | Zimmer | Implex/Zimmer | WMT, Stryker, Depuy, S&N | Zimmer | WMT | ESKA |
Porosity | 52–58 % | 80 % | 30–40 % | 50 % | 65 and 75 % | 60 % |
Cell sizea | 480–560 μm | ~500–550 μmb | N/A | N/A | ~650 and 680 μmb | 800–1,500 μm |
Inter-connecting pore sizec | ~230 μmb | N/A | N/A | ~280 and 300 umb | ||
Material | Ti | Ta | Ti, CoCr | Ti | Ti (CoCr) | Ti |
Substrate | Ti, CoCr | Polymer, stand-alone, Ti | Ti, CoCr | Ti | Ti (CoCr) | Ti |
Bioactive surface | N/A | N/A | Offered w. HA coating | N/A | TBD | N/A |
Clinical history | 15+ years | <5 years | 20+ years | 15+ years | N/A | 20 years |
Various Issues
Historically, the use of posterior stabilising designs in cementless TKA has been controversial. In theory the cam/post configuration of these implants could apply unpredictable stresses to the tibial tray-bone cementless interface [66]. These reservations have been called into question in a recent publication [67]. Obesity in combination with young age are not negative predictive factors for implant survival in cementless TKA [68, 69]. Neither is rheumatoid arthritis is a negative factor for cementless TKA with patients enjoying satisfactory outcomes in mid and long term [70]. Both cemented and cementless TKAs present with areas of periprosthetic bone loss with the cementless fixation principle not preventing its appearance [71, 72]. Cementless TKA is not contraindicated in osteoarthritic knees with severe valgus or varus deformity [73]. Recent extensive research has been published evaluating tibial tray loading under different conditions in cementless TKA [74–81]. The methodology of older papers has been criticised, initial screw fixation has been withdrawn from the system, it has been suggested that peg fixation is preferable for tantalum trabecular metal tibial trays and that HA coated implants show a preferable initial mechanical environment.
Conclusion
Old cementless TKA designs produced unsatisfactory mid and long term outcomes for various reasons. The clinical outcomes of newer designs are comparable to those of cemented designs. The application of new materials and technologies in TKA designs shows promising early results [3, 11, 12, 23, 39, 82]. The cost-effectiveness of the use of such technology either in young or in all patients remains unclear since cementless TKA costs three times more than cemented TKA in most countries [58].
References
1.
Kim YH, Park JW, Lim HM, Park ES. Cementless and cemented total knee arthroplasty in patients younger than fifty years. Which is better? Int Orthop. 2014;38:297–303.PubMedCentralPubMedCrossRef
2.
Bauer TW, Schills J. The pathology of total joint arthroplasty. I: mechanisms of implant fixation. Skelet Radiol. 1999;28:423–32.CrossRef
3.
Lombardi Jr AV, Berasi CC, Berend KR. Evolution of tibial fixation in total knee arthroplasty. J Arthroplasty. 2007;22(4S1):25–9.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







