Limb Lengthening Using the Ilizarov Method or a Monoplanar Fixator
Roger F. Widmann
Emily R. Dodwell
Purushottam A. Gholve
Arkady Blyakher
DEFINITION
Limb lengthening is a surgical procedure performed to lengthen a bone.
In the Ilizarov method, lengthening is accomplished by gradual bone distraction through a low-energy, atraumatic corticotomy site. The bone fragments are controlled via stable bone fixation using half-pins and tensioned wires through bone that are rigidly fixed to an external ring fixator or arch.11
ANATOMY
Using the Ilizarov method, one can lengthen bones of both the upper and lower extremities, including bones of the hand and foot and the surrounding soft tissue.
The most commonly lengthened bones in the lower extremity include the tibia and fibula, the femur, and the metatarsals. In the upper extremity, the most commonly lengthened bones are the humerus, the radius and ulna, and the metacarpal bones.
Consideration is given to lengthening of the surrounding soft tissues, which include the muscle tendon unit, neurovascular bundle, and skin.11
During bone lengthening, the tension in the surrounding soft tissue may predispose the lengthened segment to deformity.13, 20 Frequently encountered deformities include the following:
Femur: varus and procurvatum
Tibia: valgus and procurvatum
Humerus: varus and procurvatum
Radius and ulna: has a tendency to collapse in the interosseous space, which may cause synostosis
Metatarsal and metacarpal: apex dorsal angulation
During large lengthenings, care is necessary to prevent subluxation or dislocation of the adjacent joint.20
Femoral lengthening, especially in the setting of congenital short femur, may result in hip or knee subluxation or dislocation secondary to associated deficient acetabular coverage at the hip and the high frequency of deficient cruciate ligaments at the knee.
Tibial lengthening may cause knee or ankle subluxation and progressive equinus deformity of the foot.
Metatarsal and metacarpal lengthening can cause metatarso- or metacarpophalangeal subluxation.
All of these issues are considered during any lengthening procedure.
PATHOGENESIS
The term distraction osteogenesis implies synthesis of new bone by slow, gradual (no more than 1 mm per 24 hours) controlled distraction of the bone fragments under conditions of rigid fixation.11
The new bone is formed mostly by intramembranous ossification and, to a lesser extent, through endochondral ossification.9, 11
To provide maximum construct stability and to minimize soft tissue trauma, it is important to maintain the two fragments well apposed to each other following the corticotomy.
Distraction is a good tool for influencing reparative regeneration of both the bone and the soft tissue (“stretching tension,” as described by Ilizarov). However, the new regenerate ossifies and remodels slowly.
Gradually removing distraction and applying mild compression increases the rate of remodeling. Therefore, the regenerate becomes more rigid against bending loads.
Functional load is a strong stimulus for the improvement of blood flow and allows organic remodeling of the regenerated osseous part. The extent of load depends on the stability of fragments and the amount of regenerate.
NATURAL HISTORY
The natural history of the limb length discrepancy (LLD) depends on the condition causing the LLD.22 A partial list of causes are as follows:
Congenital shortening: proximal focal femoral deficiency, coxa vara, congenital short femur, fibula and tibia hemimelia, hemiatrophy
Congenital lengthening: overgrowth syndromes such as hemihypertrophy, Beckwith-Weidemann syndrome, Klippel-Trenaunay-Weber syndrome, and Parke-Weber syndrome
Skeletal dysplasia or tumor: Multiple hereditary exostoses may result in limb shortening on the affected side as growth cartilage cells are diverted to the cartilage tumor.19 Radiation for malignancies adjacent to the physis may result in growth suppression or complete destruction of physeal cartilage cells, resulting in LLD or angular deformity.
Infection: Physeal destruction may result from physeal invasion from adjacent metaphyseal or epiphyseal bacterial osteomyelitis or direct physeal involvement in the case of intracapsular joint physes such as at the hip and shoulder.
Paralysis: Poliomyelitis and cerebral palsy as well as other nervous system afflictions in children typically result in shortening on the more affected side.
Trauma: direct injury to growth plate, posttraumatic bone loss or shortening, and overgrowth following femoral fracture
Miscellaneous: slipped capital femoral epiphysis, Legg-Calvé-Perthes disease
Upper extremity discrepancy or shortening usually does not cause major functional problems but may result in significant cosmetic deformities.
Predicted lower extremity discrepancy of 2 to 5 cm may be dealt with by long-leg epiphysiodesis in children or by leg lengthening using the Ilizarov technique. LLD greater than 5 cm usually is amenable to leg lengthening.22
Untreated LLD of more than 3 cm may result in pelvic obliquity, visual gait disturbance, short-legged gait, or structural/nonstructural scoliosis.22
LLD greater than 5.5% of the long leg has been shown to decrease the efficiency of gait, as determined from kinetic data.
PATIENT HISTORY AND PHYSICAL FINDINGS
The underlying cause of a leg length discrepancy can typically be elucidated by careful history and physical examination.
The common symptoms at presentation are limp, compensatory gait mechanics, pelvic obliquity, and nonstructural scoliosis.
Physical findings depend on the etiologic factors.22
In hemihypertrophy (both syndromic and nonsyndromic), the affected extremity may be larger in both length and girth. In classic hemihypertrophy, upper extremity hypertrophy as well as hemifacial asymmetry may be present. Vascular overgrowth syndromes may be associated with cutaneous or deep hemangiomas, which may alter surgical approaches to attempted limb equalization.
Clinically, LLD is best measured by the block test, in which the shorter leg is placed on increasingly larger measured blocks until the posterior iliac crest is level. Discrepancies as small as 2 cm are accurately detected by this method, and detection of discrepancies is largely unaffected by patient size or body mass.25 Direct measurement of leg length from anterior superior iliac spine to the tip of medial or lateral malleolus is significantly less accurate.
True leg length is measured from the anterior superior iliac spine to the tip of the medial malleolus. It is important to place the legs in identical positions to measure true leg length.
If the patient has a 20-degree abduction deformity of right hip, the left hip is placed in 20 degrees of abduction to measure true length.22
Apparent leg length is measured with the patient supine with the legs parallel to each other. The landmarks are the umbilicus to the tip of medial malleolus. Pelvic obliquity and fixed deformities of the hip and knee affect the reading. This method is also significantly less accurate than block measurement.
Range of motion is noted for all joints, primarily the hip, knee, ankle, and subtalar joints. The ankle joint range of motion is measured with the knee in extension and flexion.22
IMAGING AND OTHER DIAGNOSTIC STUDIES
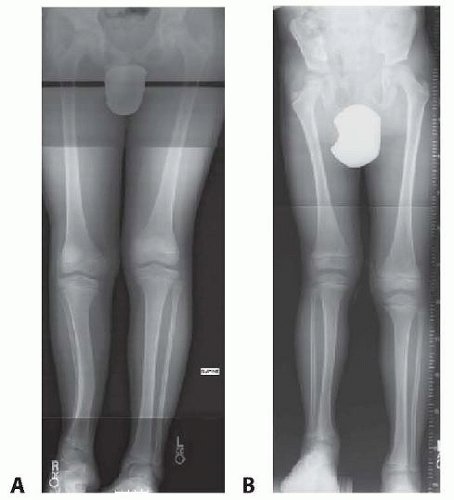
Plain radiographs have traditionally been used to document the objective measurement of LLD (FIG 1).
Full-length (hip to ankle) anteroposterior (AP) radiographs are obtained in standing position with both patellae facing directly anteriorly. The appropriate-sized block is placed beneath the shorter leg to level the pelvis. A long x-ray cassette (51 inches) is used with the x-ray beam center focused on the knee from a distance of 10 feet. A radiolucent ruler often is used to assist in calculation of limb discrepancies.
A lateral hip to ankle view can be included to further assess length, as contractures in the sagittal plane may result in inaccuracies on AP measurements. This view can also assess for angular deformities in the coronal plane.
Computed tomography (CT) scanogram has been the gold standard for low-dose, accurate imaging of leg length discrepancy.
CT scanogram is as precise in measuring LLD as the slit scanogram and it has the added benefit of more easily measuring LLD in the setting of joint contractures. Slit scanogram is of historical interest only and is no longer typically used for measuring LLD.
EOS7 is a low-dose, high-resolution radiologic imaging system, which captures both simultaneous posteroanterior (PA) and lateral radiographs and full body radiographs.12, 26
Recently, EOS biplanar imaging systems have been shown to be equally accurate/reliable with the added benefit of imaging the patient in a standing position such that leg length and alignment can be obtained from a single low-dose image. Radiation exposure is also lower with EOS.6
Skeletal age can be determined by a left hand/wrist radiograph in combination with the Greulich and Pyle method.8
The Hospital for Special Surgery (HSS) shorthand method. This method was derived from Greulich and Pyle and uses a single radiographic criteria used for each age, allowing for rapid bone age determination.10
The LLD at maturity can be predicted in a variety of ways:
The arithmetic method15
The growth remaining method1
The Moseley straight-line method17
The Paley multiplier technique21
Applications/programs that incorporate the Paley multiplication factors are readily available on phones/computers for clinical use. These allow calculation of length discrepancy at maturity for both congenital and acquired deformities.
Parental and sibling height may be useful in interpreting predicted height in the previously mentioned methods.
In LLD secondary to physeal growth arrest, graphical or arithmetic methods are helpful in determining appropriate timing of epiphysiodesis.
DIFFERENTIAL DIAGNOSIS
True shortening (eg, femoral or tibial)
Apparent shortening due to dislocated hip
Apparent shortening from contractures
Angular deformity causing apparent shortening
Overgrowth syndrome with both increased length and limb girth: hemihypertrophy
Congenital limb deficiency (beware knee joint instability)
NONOPERATIVE MANAGEMENT
No treatment is required for a predicted LLD less than 2 to 2.5 cm at maturity.
A shoe lift can be used as treatment for leg length discrepancies at maturity less than 2 cm.
Often, a lift is used in children until an appropriate skeletal age is reached to perform an equalization procedure.
A prosthesis may be necessary if deformities are so severe that adequate length or ambulatory ability cannot be achieved by operative methods.
SURGICAL MANAGEMENT
Preoperative Planning
Ilizarov Method
Accurate radiographic measurement of current discrepancy and calculation of projected LLD at maturity
Determination of which bony segment is affected
Assessment of compensatory mechanics used for walking: equinus gait, circumduction, vaulting, or combination
Assessment of contractures: for example, extra- or intraarticular, bony
Assessment of associated deformities: for example, angulation, translation, and rotation
Long-leg standing radiographs in both planes help determine malalignment.
Stability or laxity of joints (hip, knee, ankle) is determined clinically and radiographically.
Skin condition: for example, open defect, scar tissue
Planning for corticotomy level, for lengthening as well as for correction of associated deformity with appropriate room for wire or half-pin fixation
Determine optimum frame configuration, with or without inclusion of the adjacent joint.
Details on ring size, half-pin, or K-wire placement
Single-stage lengthening of 10% to 15% of bone length is associated with fewer complications.
Technical considerations
The Ilizarov frame may be constructed before surgery. The design of the frame and the number of rings and arches depend on the amount of lengthening planned.
Separate threaded connecting rods are used between each ring block and the next. A rod spanning two or more rings allows less flexibility if adjustments are needed.
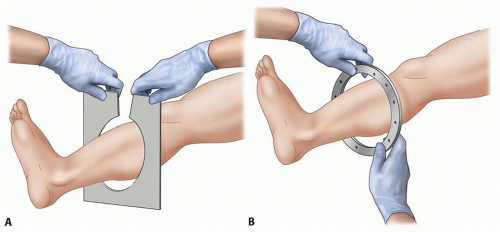
Adequate skin clearance of at least 2 to 3 cm must be maintained circumferentially under the ring. Small rings are more rigid than large rings, but smaller rings may hinder skin care and may cause soft tissue compression if there is postoperative swelling.
A template or an actual ring can be used to select the appropriate ring size (FIG 2).
Due to the changing diameter of each limb segment, different ring sizes may be required for a single limb segment (eg, the diameter of the proximal arch for the femur typically is larger than the distal ring).
Monoplanar Fixation
True measures of current discrepancy and calculation of projected LLD
Compensation mechanisms used during walking: equinus gait, circumduction, vaulting
Assessment of contractures: extra- or intra-articular
Associated deformity: angulation, translation, and rotation
Stability or laxity of joints: for example, hip, knee, ankle
Skin condition: for example, open defect, scar tissue
Long-leg films showing hip, knee, and ankle for lower extremity and similar long films for the upper extremity
Planning for corticotomy level, osteotomy level if needed for correction of associated deformity, and planning for points of fixation
Choose appropriate size for arch, rods, rail, half-pin, and/or K-wires.
Choose the appropriate size of the fixator (pediatric or adult).
Positioning
Lower extremity: supine position on any radiolucent table (eg, Jackson table)
Upper extremity: supine position with arm over a radiolucent table
Intraoperative fluoroscopy (for both the AP and lateral images)
For the Ilizarov method
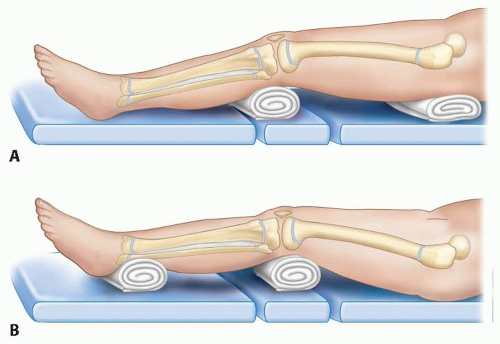
Place rolled sheets (as bumps) beneath the ipsilateral buttock and proximal tibia, leaving the femur free (FIG 3A). Similarly, for the tibia, a rolled sheet is placed beneath distal femur and ankle to create space for the tibial frame (FIG 3B).
Place a sandbag beneath the ipsilateral shoulder/scapula and rolled sheets (as bump) beneath the humerus and radius ulna to create a space for the frame.
For monoplanar fixator use, place rolled sheet (as bumps) beneath the femur and tibia to create working space for application of the frame.
TECHNIQUES
▪ Tibial Lengthening Using the Ilizarov Method
Wire Insertion
The wire insertion site is determined by local anatomy and the use of cross-sectional anatomic atlases to protect and avoid damage to blood vessels, nerves, and tendons.
In small children, 1.5-mm fixation wires are used; in adolescents and adults, 1.8-mm fixation wires are used. The wires usually are tensioned to 100 kg in children and to 130 kg in adults.
The wire is introduced from the side nearest the neurovascular bundle. This helps prevent inadvertent injury to the neurovascular structures.
Initially, the wire is gently pushed through the soft tissue until it hits bone cortex. The center of the bone is located, and the wire is drilled through the cortex. It is important not to bend the wire while drilling.
The wire is prevented from bending by a short lever arm on the wire that holds the wire with a wet sponge or by use of a protective soft tissue sleeve (TECH FIG 1).
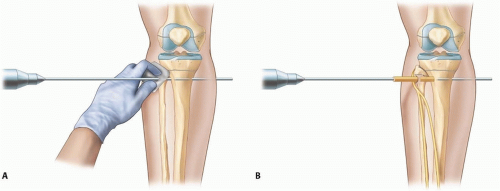
TECH FIG 1 • Bending of wire during insertion is prevented by holding the wire with a wet sponge (A) or with a protective soft tissue sleeve (B).
After piercing the far cortex, the lowest possible drill speed is used to further insert the wire. After exiting the far skin, the wire is inserted further by tapping with a mallet.
The wire is fixed to the ring without bending the wire. Bent wires will move the bony fragments on tensioning.
Any tension or puckering of the skin at wire insertion or exit is corrected by releasing the surrounding skin or fascia with the help of a no. 15 blade on a scalpel.
Half-Pin Insertion
Hydroxyapatite-coated half-pins are recommended because they achieve better fixation and are associated with lower rates of infection and loosening.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree