Lengthening of Gastrocnemius Fascia
James J. McCarthy
David A. Spiegel
DEFINITION
Lengthening of gastrocnemius fascia is commonly performed for conditions in which the patient positions their foot in equinus either while standing or walking.
Equinus represents a loss of dorsiflexion and may be due to true shortening of the musculotendinous unit (myostatic contracture) and/or increased muscle tone or spasticity (dynamic contracture).
The most common condition in which this procedure is performed is cerebral palsy; however, other conditions include idiopathic toe walking, traumatic conditions, complications of surgical procedures such as tibial lengthening, and a variety of neuromuscular disorders.
Some disorders, such as Charcot-Marie-Tooth disease, may appear to have equinus, but the true deformity is plantar flexion of the midfoot on the hindfoot (midfoot cavus). Other disorders may have equinus that is less obvious due to a break in the midfoot and apparent dorsiflexion. The plantar flexion will be evident with correction of the midfoot.
Ankle equinus and midfoot cavus may also be observed in selected conditions.
ANATOMY
The medial and lateral heads of the gastrocnemius muscles, the soleus, and the plantaris muscles form the triceps surae. Although all are part of the same muscle group, their structure and function differ.
The larger medial head of the gastrocnemius arises from the popliteal surface of the femur just above the medial femoral condyle, and the lateral head originates from the superolateral surface of the lateral femoral condyle.
The medial and lateral muscle bellies insert into a midline tendinous raphe that widens into the aponeurosis of the gastrocnemius at or just above the midcalf.
This tendon unites with the soleus forms the conjoined tendon which inserts into the calcaneus by way of the tendo Achilles. A study of 40 cadavers indicated that there are five morphologic patterns identified at the “conjoint junction” or the place where the gastrocnemius tendon unites with the aponeurosis of the soleus. These include transverse (25%), oblique passing distally and medially (45%), oblique passing distally and laterally (5%), arcuate as an inverted U (17.5%), and a U-shape (7.5%).5
As far as the location of the conjoint junction, Elson et al5 found that on the medial side, the gastrocnemius tendon could be located between 36% and 46% of the distance between the upper border of the calcaneus and the fibular head on the medial side, 45% to 58% in the midline, and 48% to 51% on the lateral side.
Pinney et al12 found that the gastrocnemius tendon was an average of 18 mm distal (20 to 57 mm) to the surface landmark of the distal aspect of the gastrocnemius muscle belly.
The gastrocnemius spans the ankle and knee joint and therefore can plantarflex the ankle and/or flex the knee. It typically has fast twitch type II muscle fibers, allowing for short, powerful bursts of activity, important in activities such as running and jumping.
The soleus lies deep (anterior) to the gastrocnemius muscle. It originates on the proximal tibia, fibula, and interosseous membrane, and its fascia blends with the tendon of the gastrocnemius to form the conjoined Achilles tendon or triceps surae. Contraction results in ankle plantarflexion. It is made up of primarily slow twitch type I muscle fibers. The soleus acts eccentrically to decelerate advancement of the tibia over the foot during the second rocker in stance phase and then concentrically during the push-off phase of gait.
The plantaris arises just above the lateral head of the gastrocnemius and inserts into the calcaneus; it is largely vestigial and should be released at the time of surgery.
PATHOGENESIS
Equinus positioning of the foot can occur due to the following:
Increased tone or spasticity of the triceps surae muscles
Shortening of some or all of the muscles
Joint contracture
Bony deformity
It is critical to differentiate the cause of the equinus because the treatment options differ in each circumstance.
The initiating etiology of this disorder varies. Spasticity, weakness, and subsequent shortening of the muscle group can occur, secondary to neuromuscular disorders such as cerebral palsy. Relative shortening of the triceps surae, as occurs when the tibia is lengthened, or fixed positioning of the foot in equinus, such as prolonged casting in plantar flexion, can all result in equinus of the ankle. Bony changes at the ankle due to trauma or congenital disorders may also result in equinus.
NATURAL HISTORY
The natural history varies according to each disease process and prior treatment history.
Equinus tends to progress in patients with cerebral palsy. The deformity begins as a dynamic loss of motion due to spasticity and then progresses to myostatic contracture. The contracted muscles may tether growth, resulting in skeletal deformities.
Equinus is also likely to progress in the majority of neuromuscular disorders.
Some disorders, such as idiopathic toe walking, often improve as the patient matures into adulthood.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients may complain of tripping/falling due to inability to easily clear the limb during swing phase and/or pain over the metatarsal heads or forefoot from increased stress distribution over the forefoot.
Range of motion of the ankle should be assessed with the hindfoot inverted to lock the subtalar joint, avoiding spurious dorsiflexion through the transverse tarsal joints.
The Silfverskiöld test assesses the degree of passive ankle dorsiflexion with the knee flexed and extended. If dorsiflexion is restricted with the knee flexed, then there is contracture of the soleus. Loss of dorsiflexion when the knee is in extension indicates a contracture of the gastrocnemius.
Observational or instrumented gait analysis is important to correlate the physical finding with functional deficits during ambulation. The patient should be evaluated when walking and/or running.
Small limitations in dorsiflexion range may have little functional deficit.
Silfverskiöld test: The ankle should be able to be dorsiflexed 10 degrees.
Observational gait analysis: rockers
First (heel): initial contact to loading response
Second (ankle): midstance foot flat
Third (forefoot): terminal stance
IMAGING AND OTHER DIAGNOSTIC STUDIES
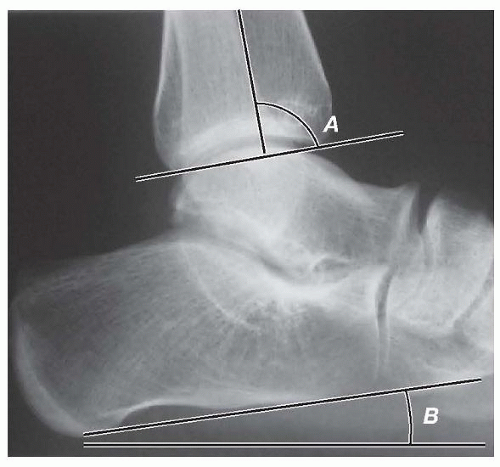
Although not routinely required, standing lateral radiographs of the foot may help to evaluate equinus, especially when there may be a component of midfoot cavus (FIG 1).
The angle between horizontal and a line drawn across the plantar aspect of the os calcis (calcaneal pitch) should be 15 degrees (0 and 30 degrees).
The angle between the line drawn through the tibia and along the distal articular surface of the tibia parallel to the measure 80 degrees (distal articular surface is dorsiflexed).
The contribution of the midfoot may be assessed by measuring the talo-first metatarsal angle (Meary angle).
DIFFERENTIAL DIAGNOSIS
Cerebral palsy, Duchenne muscular dystrophy, and other neuromuscular disorders
Idiopathic toe walking
Congenital limb deficiencies
Bony deformity (posttraumatic, malalignment, asymmetric growth arrest)
Postimmobilization
Posterior tibial lengthening
NONOPERATIVE MANAGEMENT
Physical therapy and stretching is the most common form of treatment for mild deformities and used in an attempt to maintain range when gained by other methods. The knee must be extended and the hindfoot placed in an inverted position when stretching the ankle.
Bracing and/or nighttime splinting can be used in combination with other techniques. It is primarily used to maintain gains or prevent worsening deformity.
Botulinum toxin (BTX) causes a reversible neuromuscular blockade by blocking acetylcholine release at the neuromuscular junction and can be considered as an adjunct to physical therapy and/or casting especially in patients with spasticity. The effect lasts about 3 to 8 months.1
Serial casting10, 13 can also be used, in which short-leg casts are typically placed. They are changed weekly or biweekly, each time with increasingly greater dorsiflexion.
Usually, three or four casts are used until satisfactory range is obtained.
Recurrence is common, and if not carefully performed, skin breakdown can occur.
SURGICAL MANAGEMENT