Lateral Epicondylitis (Tennis Elbow) Arthroscopic Treatment
Alexander A. Fokin
Colin P. Murphy
Kevin P. Murphy
DEFINITION
Lateral epicondylitis (LE) is a common musculoskeletal disorder that is characterized by lateral epicondylar pain and tenderness over the origin of the extensor carpi radialis brevis (ECRB) slightly distal and anterior to lateral epicondyle with exacerbated pain at the resisted extension of the wrist.
The term epicondylitis is a misnomer due to the paucity of inflammatory changes implied by the suffix “-itis.”
Other known synonyms are traumatic enthesopathy of the ECRB, tendinopathy of ECRB, lateral epicondylalgia, lateral epicondylosis, tendinosis of ECRB, lawn tennis elbow, and so forth.
LE was first described in 1873 by F. Runge from Germany and was called a writer’s cramp attributed to a periostitis of lateral humeral epicondyle. The term tennis elbow was coined by H.P. Major in 1883 in relation to 1882 publication in the Lancet by H. Morris describing the condition as “the lawn tennis arm” resulting from frequent back stroke.35
INCIDENCE
LE has an average prevalence of 3% in the general population, ranging from 0.7% to 4.0% and peaking in patients aged between 45 and 54 years, with almost equal gender distribution.19,36 It is less common in black individuals. LE affects more often the dominant arm; bilateral or nondominant arm involvement is rare.
LE is a known work-related disorder with up to 14.5% prevalence in manual labor intensive industries such as foodprocessing industry or automobile manufacturing where repetitive “turn and screw” movements may be identified as a risk factor.23
The prevalence of LE among tennis players was reported at 1.3% to 14.1% with no gender difference. Risk factors such as heavy racquets, inappropriate grip size, high string tension, and so forth were suggested; however, the studies revealed that the use of string vibration dampers and grip size modifications did not have an effect on the development of the condition. It is more likely that LE is rather related to the improper technique that is more common in inexperienced players.1
ANATOMY
The main anatomic structures associated with LE are lateral epicondyle of the humerus and the tendon of ECRB.
Anatomic position of the ECRB tendon makes its undersurface vulnerable to contact and abrasion against the lateral edge of the capitellum during elbow motion, especially in extension and pronation.
ECRB originates mainly from the lateral epicondyle by the common extensor tendon and inserts distally into dorsal surface on the base of the third metacarpal bone, thus acting as a prime dorsiflexor of the hand.
The proximal portion of ECRB is covered by the extensor carpi radialis longus (ECRL) so that the latter must be elevated to visualize the former.
The origin of ECRB is entirely tendinous and diamond shaped, whereas the ECRL origin is muscular and has a triangular shape.
It is crucial to identify the full length of the pathologic tissue of ECRB to perform an adequate resection that includes approximately 13 to 15 mm of tendon. For easier identification of the ECRB origin from the extensor digitorum communis (EDC), it is recommended to follow orientation of the fibers from distal to proximal end of the forearm, and also, it could be easier distinguished from undersurface of the extensor.13
Among the other anatomic structures that possibly can be involved in the development of the condition are synovial fold (SF), capitellum, radial head, and joint capsule.
SF, also known as synovial plica or a synovial fringe, is a thickening of the synovium on the proximal edge of the annular ligament but distinct from the latter. SF prevents excessive movements in the radiohumeral joint.
Inflammation and thickening of SF (termed as SF syndrome) as the result of repetitive trauma can cause its impingement between the capitellum and radial head especially with elbow extension and forearm pronation. Subsequent focal synovitis may develop most often in the posterolateral quadrants of SF and is manifested by painful snapping in the elbow joint.12,37
PATHOGENESIS
The attachment of the tendons and ligaments to bones is termed as enthesis (meaning insertion in Greek).
Entheses are sites of high mechanical stress, and with aging, normal entheses are subject of wear and tear with consequent degenerative changes.
ECRB enthesis is fibrocartilaginous and helps to create a more gradual change in mechanical properties between soft and hard tissues. Enthesis ensures that any bending of the tendon/ligament fibers during joint movements is spread away from the bone—thus dissipating stress concentration.
Stress concentration at an insertion site involves not only enthesis itself but neighboring tissues as well. Many entheses have bursa and fat near the insertion site and in some cases deep fascia.
The concept of “functional synovio-entheseal complex” implies that one component (the enthesis) is prone to microinjury and the other (the synovium) to inflammation.
Enthesis is a relatively avascular structure with a limited capacity to accumulate fluid.7
Histopathology
Repetitive ECRB microtrauma initiates a degenerative process with ingrowth of weakened reparative tissue that results in angiofibroblastic hyperplasia known as angiofibroblastic tendinosis.
Degenerative, noninflammatory changes are characterized by the presence of disorganized collagen and immature fibroblasts and vascular granulation. Corticosteroid injections into tendons may also result in similar appearance.
Due to the described contact between the ECRB and the radiocapitellar joint, the matching cartilage lesions of the capitellum and radial head were reported in up to 65% and 81%, respectively, in surgical patients with LE.33
NATURAL HISTORY
The onset of LE is usually insidious, resulting from repetitive overuse microtrauma and rarely could it be secondary to an acute event.
LE progression can be categorized by three phases: (1) acute phase (up to 3 months), (2) subacute or intermediate phase (3 to 6 months), and (3) chronic phase (more than 6 months).
During acute phase, icing, rest, and activity modifications are recommended in conjunction with other conservative treatment modalities such as nonsteroidal anti-inflammatory drugs (NSAIDs).
In 90% to 95% of the cases, the timely administration of conservative treatment combined with a daytime bracing of the forearm (to reduce stress) placed over ECRB, distal to the lateral epicondyle, should alleviate acute LE symptoms.
With continuous repetitive trauma, fraying of the tendon and microtears can progress to macroscopic tears and even to rupture or avulsion.
If the lateral joint capsule is involved in chronic LE, it can avulse along with ECRB tendon that may result in the development of a lateral synovial cyst and lateral joint instability.
Chronic refractory LE could extend from ECRB and involve the anterior portion of EDC that may ultimately lead to weakening of wrist extension and supination.
In rare cases does severe chronic LE may require tendon transfer surgery for extensor function restoration.
Table 1 Arthroscopic Classification of Lateral Epicondylitis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
PATIENT HISTORY AND PHYSICAL FINDINGS
Comprehensive assessment of patient’s history is an important first step in diagnosis of LE that directs the following clinical evaluation and helps in choosing appropriate course of treatment sequence.
The review of patient’s history must reflect the onset, circumstances, and duration of pain and associated symptoms.
Hand dominance, particularities of sport activities, and occupational factors should be documented in detail.
All previously applied treatments and their effectiveness should be recorded and evaluated.
Patients who have had a good initial response to conservative treatment followed by reaggravation of symptoms may have resumed strenuous activities too soon and may respond to an additional trial of nonoperative management.
A prior surgical history of the involved elbow is extremely important for operative planning and can also contribute to the diagnosis. Furthermore, a previous ulnar nerve transposition could place the ulnar nerve at risk when establishing arthroscopic portals and may require an open approach.
When pain and tenderness during palpation is present in the area just distal to lateral epicondyle and it is exacerbated at the resisted extension of the wrist, then patient is diagnosed with LE.
Physical Examination
It is pertinent to perform a thorough physical examination of both the ipsilateral and contralateral upper extremity as well as of the cervical spine.
Palpation of the lateral epicondyle and common extensor area. The epicenter of pain and tenderness is located slightly anterior and distal (1 to 3 cm) to lateral epicondyle over the origin of the ECRB. Erythema, warmth, or swelling is absent.
Positive “Chair test.” Patient refuses or unable to lift a chair with a pronated hand due to elicited lateral elbow pain.
Positive Cozen test. Exacerbated pain at the lateral epicondyle at the resisted dorsiflexion of the wrist while the forearm is pronated and elbow is flexed at 90 degrees.
Positive Mill test. Pain in the area of lateral epicondyle at the resisted extension of the middle finger while elbow is flexed at 90 degrees and forearm is pronated with wrist flexed.
Grip strength and resisted supination. Grip strength is diminished in 78% of patients with LE. Resisted supination elicits pain in 51% of patients. Pain with turning a door knob is indicative of LE.
IMAGING AND OTHER DIAGNOSTIC STUDIES
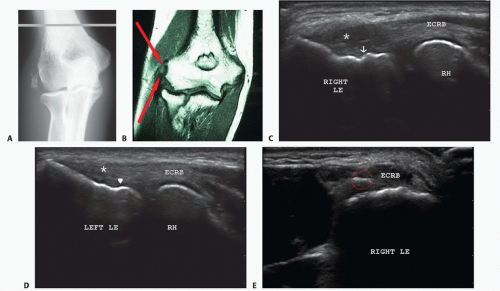
Radiographic evaluation is required to exclude coexisting pathology, especially in recalcitrant cases and is limited to anteroposterior (AP) view in full extension and lateral view at 90-degree flexion of the elbow.
Magnetic resonance imaging (MRI) has 90% to 100% sensitivity and 83% to 100% specificity for detecting epicondylitis.27
MRI reveals increased signal intensity on T1- and T2-weighted images and thickened extensor tendon (FIG 1B).
Coronal or axial T2-weighted images show fluid signal intensity in the areas of partial- or full-thickness tendon tears of ECRB. Adjacent soft tissue edema may be seen on T2-weighted sequences.
Magnetic resonance arthrography with gadolinium contrast agent may help in detection of intra-articular and periarticular lesions such as collateral ligament tears, capsular disruptions, loose bodies, and so forth. Intravenous gadolinium contrast administration helps to demonstrate bone perfusion and viability.16
Thickening of SF beyond 3 mm and abnormal signal intensity with irregular margins on MRI may be associated with SF syndrome.
Histologic and surgical findings correlate with MRI findings of tendon damage and degeneration.38
Ultrasound (US) is a noninvasive method for LE evaluation that also allows immediate dynamic measurements in flexion and extension.
US evaluation of LE has a reported sensitivity of 80% and specificity of 50%. US, however, has a high false-positive rate and is most useful in the evaluation of the extent of the tendon lesion in symptomatic patients.
Tendinosis is manifested as a tendon thickening and hypoechoic heterogeneous echo texture with loss of normal longitudinally oriented fibrillar pattern (FIG 1C,D). Tendon tears are seen as anechoic areas.
The degree of hyperemia on Doppler imaging reflects the extent of the increased vascularity, and depending on the stage of the process, it may indicate pathologic changes or can reflect the healing progression.
Surrounding fluid and calcification may also be seen (FIG 1E).
A convex boundary of the extensor tendons, an erosive lateral epicondylar cortex, internal calcifications, and tendon tears on a gray-scale US combined with color Doppler findings of neovascularity have a high diagnostic accuracy.22,30,38
Multiple steroid injections can affect the echo texture of the tendon.
Normal SF is identified by US as a hyperechoic triangular silhouette and pathologic SF exhibits thickening and irregular echogenicity.12
Other Evaluation Methods
Self-reported measures include a number of validated patientbased questionnaires.
Patient-Related Tennis Elbow Evaluation (PRTEE) questionnaire assesses both elbow function and pain and is considered as a standard and reliable outcome measure for LE.
Visual Analog Scale (VAS) is commonly used for pain intensity evaluation.
Disability of the Arm, Shoulder, and Hand (DASH) questionnaire quantifies pain and disability related to upper extremity.
Andrew-Carson Elbow Scores (ACES) and Mayo Elbow Performance Score (MEPS) are also used for evaluation of patients with LE before and after treatment.
Biomechanical assessment includes pain-free grip (PFG) strength and rate of force development measured with Jamar dynamometer. Maximal grip strength can be adversely affected in LE patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree