Lateral Columnar Release for Extracapsular Elbow Contracture
Leonid I. Katolik
Mark S. Cohen
DEFINITION
Extrinsic elbow contracture refers to elbow stiffness secondary to fibrosis, thickening, and, occasionally, ossification of the elbow capsule and periarticular soft tissues.
In contrast to intrinsic contracture, the articular surface is either uninvolved or minimally involved, without the presence of intra-articular adhesions or articular cartilage destruction.
Although a distinction is made between extrinsic and intrinsic causes of contracture, these entities often overlap.
ANATOMY
The elbow is a compound uniaxial synovial joint comprising three highly congruous articulations.
The ulnohumeral joint is a ginglymus, or hinge, joint. The radiocapitellar and proximal radioulnar joints are gliding joints.
All three articulations exist within a single capsule and are further stabilized by the proximity of the articular surface and capsule to the intracapsular ligaments and overlying extracapsular musculature.
PATHOGENESIS
The propensity for elbow stiffness after even trivial elbow trauma is well recognized. After even seemingly trivial injuries, the capsule can undergo structural and biochemical alterations leading to thickening, decreased compliance, and loss of motion.
Causes of extrinsic elbow contracture include capsular contracture, damage to and fibrosis of the flexor-extensor muscular origins, collateral ligament scarring, heterotopic bone, and skin contracture.
Prolonged immobilization after trauma may be a separate risk factor for the development of stiffness.
NATURAL HISTORY
Little consensus exists regarding the natural history of capsular contracture. It is felt that appropriate recognition and treatment of acute elbow injuries, avoidance of prolonged immobilization, and early active range of motion may limit the severity of posttraumatic extrinsic contracture.
Patients typically do not tolerate elbow stiffness well because adjacent joints do not provide adequate compensatory motion.
Morrey10 showed that the performance of most activities of daily living requires a functional arc of motion from 30 to 130 degrees.
Vasen and colleagues11 have demonstrated that volunteers with uninjured elbows may adapt to a functional arc of motion from 70 to 120 degrees to perform 12 tasks of daily living.
Patients typically request treatment for elbow contracture when loss of extension approaches 40 degrees and flexion does not exceed 120 degrees.
Patients who do not improve with a concerted effort at nonoperative treatment often require surgical release.
Stiffness of the elbow typically is incited by soft tissue trauma, hemarthrosis, and the patient’s response to pain. Elbow trauma may cause tearing and contusion of the periarticular soft tissues. The patient typically holds the injured elbow in a flexed position to reduce pain. A fibrous tissue response then ensues within the hematoma and damaged muscular tissues. This fibrous tissue may ossify. In addition, overly aggressive therapy may further exacerbate these injuries, potentiating the cycle of pain, swelling, and limitation in motion that leads ultimately to frank contracture.
Collateral ligament injury may contribute to contracture. Primary fibrosis may develop within the collateral ligaments because of the initial injury. Alternatively, secondary fibrosis may result from immobilization and scar formation.
Significant injury to the anterior joint capsule and the overlying brachialis muscle may also result in capsular hypertrophy and fibrotic reaction contributing to ankylosis. This is particularly common in association with fracture-dislocations of the elbow.
PATIENT HISTORY AND PHYSICAL FINDINGS
The cause of contracture should generally be easily elucidated from the history. Particular notation should be made of concomitant injuries, including closed head injury or associated burn injury.
The duration and possible progression of symptoms should be noted.
The impact of the contracture on the patient’s upper extremity function and any limitations in activities of daily living should be noted.
Any previous treatment for contracture should be elucidated. This should include the appropriateness, duration, and results of prior physical therapy, splinting, intra-articular injections, and surgeries.
For patients with prior elbow surgery, the presence and type of any residual internal fixation devices should be noted. In addition, attention should be paid to any remote history of elbow infection.
Physical examination should include a general physical examination as well as a detailed examination of the involved extremity.
Attention must be paid to the examination of the skin and soft tissue envelope about the elbow, with notation made of prior incisions, skin grafts, flaps, or areas of wound breakdown.
Elbow motion should be measured with a goniometer and active and passive motion should be compared.
Notation should be made whether motion improves with the forearm in full pronation, which may suggest posterolateral rotatory instability.
Although rare, symptomatic incompetence of the ulnar collateral ligament may elucidated by examination.
Strength of the involved limb should be assessed, as a joint without adequate strength is unlikely to maintain motion after release.
Because many posttraumatic and inflammatory contractures about the elbow are associated with ulnar nerve symptoms, a careful neurologic examination should be performed. A positive Tinel test over the cubital tunnel as well as a positive elbow flexion test should increase the suspicion for concomitant ulnar nerve pathology.
IMAGING AND OTHER DIAGNOSTIC STUDIES
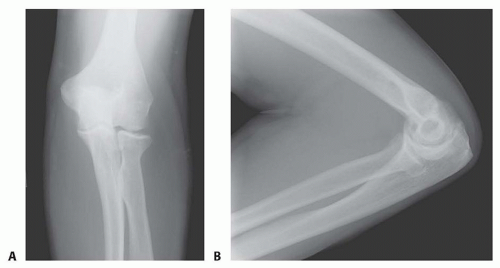
Anteroposterior (AP) and lateral radiographs are often all that is needed for preoperative planning (FIG 1).
Cross-sectional imaging with computed tomography is helpful in visualizing the articular surfaces, particularly after fracture.
We advocate the use of computed tomography for preoperative planning in cases of moderate to severe heterotopic ossification.
Extracapsular contracture is typically not painful through the remaining arc of motion and is not painful at rest. If pain is a significant component of the patient’s symptoms, serologic workup for infection, including a complete blood count, erythrocyte sedimentation rate, and C-reactive protein, is indicated.
DIFFERENTIAL DIAGNOSIS
Conversion disorder
Infection
Inflammatory arthropathy
Intracapsular contracture
NONOPERATIVE MANAGEMENT
Alternative measures to improve elbow stiffness include conservative modalities to decrease joint swelling and inflammation and relax or stretch contracted soft tissues. For protracted swelling, edema control sleeves, ice, elevation, active motion (including the forearm, wrist, and hand), and oral agents such as anti-inflammatory medication can be useful.
A short-term oral prednisone taper can be very effective in difficult cases. In addition, one can consider an intra-articular cortisone injection to decrease inflammation and joint synovitis.
Rarely, when patients exhibit guarding and involuntary co-contraction, biofeedback may be a helpful adjunct.
Dynamic splints, which apply a constant tension to the soft tissues, may be helpful.5
These braces improve range of motion through soft tissue creep. They tend to be more painful to wear and may cause unwanted inflammation.
Patient-adjusted static braces appear to be more effective. These braces use the principle of passive progressive stretch, allowing for stress relaxation of the soft tissues. They are applied for much shorter periods of time and are better tolerated by patients.
SURGICAL MANAGEMENT
To improve elbow flexion, one must release any soft tissue structures posteriorly that might be tethering the joint. These include the posterior joint capsule (including the posterior bundle of the ulnar collateral ligament) and the triceps muscle and tendon, which can become adherent to the humerus.1,6,8,9
Any bony or soft tissue impingement also must be removed anteriorly, including osteophytes off the coronoid process and any bony or soft tissue overgrowth in both the coronoid and radial fossae.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree