Chapter 22 Lactose Malabsorption Testing
 Introduction
Introduction
Lactose malabsorption results from the inability to properly digest lactose, the disaccharide found in mammalian milk. Lactase is an enzyme in the brush border (microvilli) of the small intestine responsible for cleaving lactose into absorbable monosaccharides. Lactase enzyme deficiency leads to lactose malabsorption as the gut is unable to absorb the larger diasaccharide. When symptoms such as diarrhea, bloating, flatulence, or abdominal discomfort result from this malabsorption, a diagnosis of lactose intolerance is given. Lactose intolerance affects an estimated 25% of Americans and 75% of adults worldwide.1 As shown in Table 22-1, the condition occurs in people of all ethnic backgrounds, with a near 100% prevalence observed in Asians. Within the United States, prevalence parallels country of origin, with the highest rates in African Americans, Hispanic Americans, Asian Americans, and Native Americans.2
TABLE 22-1 Prevalence of Lactose Intolerance by Ethnic Group
| GROUP | PREVALENCE (%) |
|---|---|
| African blacks | 97-100 |
| Asians | 90-100 |
| North American blacks | 70-75 |
| Mexicans | 70-80 |
| Persons of Mediterranean descent | 60-90 |
| Persons of Jewish descent | 60-80 |
| North American whites | 7-15 |
| Northern Europeans | 1-5 |
The generalized nature of abdominal symptoms of lactose intolerance can obscure proper diagnosis,3 resulting in symptom management through medical intervention. However, when properly diagnosed, lactose intolerance may be treated with patient education, lactase supplementation, and dietary modifications,4 eliminating the need for medical interventions. In patients experiencing symptoms, a nutritional history and objective measures of lactose malabsorption can lead to the diagnosis of lactose intolerance. Objective measures for lactose malaborption include stool pH testing, lactose tolerance testing, and hydrogen/methane breath testing. In addition, genomic tests are also available to assess the presence or absence of polymorphisms linked to lactase enzyme deficiency.
Controversy surrounds the subject of lactose intolerance stemming from the dramatic decrease in dairy consumption that can result from its diagnosis. Numerous studies showed a correlation between decreased dairy consumption and a rise in calcium-dependent conditions, such as osteoporosis, heart disease, and colon cancer.5–10 Studies also indicated that food-based calcium was a better source of this nutrient than supplements. Because dairy foods are the richest and best-absorbed dietary sources of calcium, careful diagnosis should be made before these foods are eliminated from the patient’s diet. Dietary limitation of calcium rich foods should only be done in the context of objectively proven lactose intolerance. Many patients with lactose malabsorption are able to consume moderate amounts of lactose without symptoms, so both the diagnosis and treatment should be pursued under professional guidance.11
 Pathophysiology
Pathophysiology
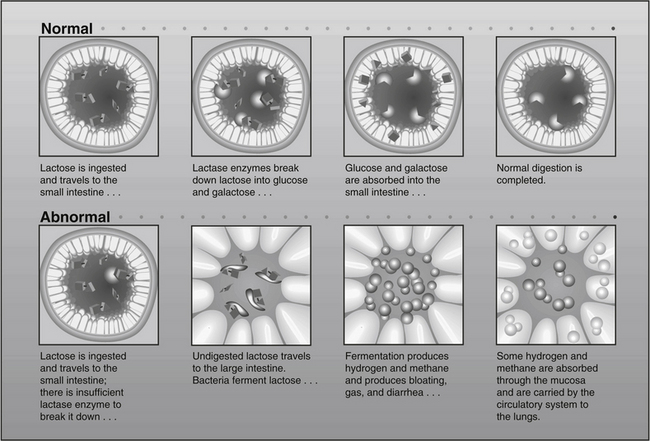
Lactose is a disaccharide that can be hydrolyzed by the lactase enzyme lactase-phlorizin hydrolase (LPH) into glucose and galactose, which are actively absorbed in the small intestine (Figure 22-1). When LPH activity is decreased in the brush border (microvilli) of the distal duodenum and proximal jejunum, then lactose malabsorption results. The presence of lactose malabsorption does not always result in lactose intolerance. Only when the amount of lactose ingested exceeds digestive capacity does lactose persist in the lumen, ultimately reaching the colon, where it may lead to osmotic retention of fluid and bacterial fermentation, thus causing the symptoms characteristic of lactose intolerance (see Figure 22-1).12 Therefore, symptoms of lactose intolerance often require several contributing factors in addition to LPH deficiency, including (1) relatively high lactose load, (2) gut dysmotility13 (3) rapid small bowel transit, (4) heightened visceral sensitivity,14 and/or (5) altered bowel flora.15
 Adult-Type (Primary) Lactose Deficiency
Adult-Type (Primary) Lactose Deficiency
The majority of the world’s population has a normal decrease in LPH synthesis after weaning. This common autosomal recessive genotype confers the phenotype of primary lactase deficiency (lactase nonpersistence). Genetically, nucleotide sequences in the distal enhancer region of the LCT gene (chromosome 2), which encodes LPH, appear responsible for this developmentally programmed loss of transcription.16
It is theorized that maintaining the ability to digest lactose into adulthood (lactase persistence) is the result of a relatively new evolutionary genetic mutation that occurred after the domestication of farm animals.17 Preservation of lactase synthesis has been associated with several distinct single nucleotide polymorphisms (SNPs) on the distal enhancer region of the LCT gene (–13910C>T, –13915T>G, –14010G>C). Although the presence of any these SNPs suggests lactase persistence, their absence does not equate to lactase nonpersistence, because there appear to be other SNPs that have not yet been determined.18
 Acquired (Secondary) Lactase Deficiency
Acquired (Secondary) Lactase Deficiency
Because LPH is located in the brush border (microvilli) of gut mucosal cells, LPH deficiency may be secondary to diseases that damage these cells. Lactose intolerance has been observed as a secondary feature in celiac disease,19 tropical sprue, acute gastroenteritis, chemotherapy-induced mucositis,20 cystic fibrosis, alcoholism,21 pelvic radiation therapy,22 and Crohn’s disease.23 In secondary lactase deficiency, treating the underlying condition and resultant restoration of mucosal integrity often restores lactase activity.24
 Congenital Lactase Deficiency
Congenital Lactase Deficiency
Congenital lactase deficiency is a rare inborn error of metabolism characterized by very low or absent lactase activity in the intestinal microvilli at birth. Unlike lactase nonpersistence mutations, which affect upstream enhancer regions of LCT, mutations in the LCT gene itself appear to be responsible for congenital lactase deficiency.25 Clinical symptoms include severe diarrhea, dehydration, and malnutrition, and often appear during the first week with the consumption of lactose. Separately, preterm infants may exhibit symptoms of lactase deficiency if born before 34 weeks’ gestation, a condition called developmental lactase deficiency.26 As expected, preterm infants can gain function of the lactase enzyme with time.
 Lactose Intolerance Versus Dairy Allergy
Lactose Intolerance Versus Dairy Allergy
Lactose intolerance and dairy allergy are separate pathologies. Lactose intolerance results from the maldigestion of dairy carbohydrate (lactose), whereas dairy allergy is an immune response to dairy proteins (e.g., casein, lactalbumin, whey). Dairy allergy may involve reactions (e.g., systemic anaphylaxis) that affect the gastrointestinal tract, skin, respiratory tract, or multiple systems. These immediate reactions are often mediated by immunoglobulin-E (IgE) and can cause severe morbidity and even death; however, in such cases, dietary elimination of dairy products is associated with good prognosis.27 The prevalence of IgE-mediated allergic reaction to dairy protein in the general population is estimated at 1% to 3%, being highest in infants and lowest in adults. However, the prevalence of IgG-mediated allergic reactions may be higher.
 Diagnosis of Lactose Intolerance
Diagnosis of Lactose Intolerance
Clinical suspicion of lactose intolerance should be raised when foods containing milk or milk products produce symptoms of gas, bloating, cramping, or diarrhea (Box 22-1). A short course of dietary manipulation, with careful removal of milk containing products, can strengthen the case for lactose intolerance as a diagnosis. Testing stool acidity, oral lactose tolerance testing, breath tests for hydrogen and methane, and/or genomic evaluation for LCT haplotypes should be used to confirm the diagnosis. Because the presence of lactase deficiency does not always result in lactose intolerance, genomic testing should never be used as a sole determinant in diagnosis. Breath testing provides the most reliable noninvasive means of determining lactose malabsorption, but must be used in the context of symptomology to make the diagnosis of lactose intolerance. In contrast, a positive breath test coupled with the absence of LCT haplotyping indicating primary lactase deficiency suggests a secondary causation, the diagnosis of which should be pursued.
There have been conflicting results regarding the presence of lactose intolerance in patients with irritable bowel syndrome (IBS). By definition, the diagnosis of IBS is a functional diagnosis that is made when all organic causes of symptoms have been ruled out. However, studies have shown that IBS patients have a high rate of lactose intolerance, with resolution of IBS symptoms upon lactose limitation or removal.28–30 Rana et al31 found that patients with diarrhea-predominant IBS had a higher incidence of lactose intolerance (82%) than patients who had either spastic-type IBS or features of both IBS types. For this reason, lactose intolerance should always be investigated in cases of IBS, a condition that affects up to 20% of Americans.32
A number of studies have suggested that transient lactose intolerance is also associated with infantile colic.33,34 For susceptible children with lactose maldigestion, only 12 grams of lactose (~1 cup of milk) daily has been shown to be associated with increased abdominal pain.35
Nutritional History
A detailed history of the patient’s average consumption of lactose-containing food should be obtained. Often, patients do not consider yogurt, ice cream, chocolate milk, and milk ingested with cereal as important sources of lactose. They also may not be aware that lactose is added to many nondairy products to provide texture, flavor, and browning, and to absorb flavors, aromas, and food colors (Box 22-2). In addition, because of its excellent binding ability, lactose is contained in many drugs and over-the-counter products (Box 22-3). Identifying all sources of lactose is necessary to (1) identify the potential relationship between gastrointestinal symptoms and lactose consumption and (2) develop an effective lactose-free diet, if necessary.