I. FOUNDATION OF INJURY DIAGNOSIS. Knee injuries are common in active individuals. Both acute and overuse injuries occur, and they require different investigative processes to diagnose and treat them properly.
A. Subdivision of clinical categories
- Acute injury is an injury that happens where a single application of force creates the musculoskeletal damage. This is common in athletics, motor vehicle trauma, etc.
- Acute on chronic injury is an injury that results in a disabled state that can be quiescent over time and result in a new injury episode at a later time. This new injury would represent an acute injury. However, this new injury typically involves less force than the original acute injury, as there was preexisting damage to the musculoskeletal tissue. Common examples might be recurrent patella instability or recurrent shoulder subluxation.
- Overuse injury is an injury that is characterized by the absence of a traumatic event. This kind of injury results from repetitive submaximal or subclinical trauma that results in macro- or microscopic damage to a structural unit and/or its blood supply. This overuse pattern can be seen in all musculoskeletal tissue but is most common in bone (overuse pattern resulting in stress fracture), bursal tissues (overuse pattern resulting in bursitis), and tendon (overuse pattern resulting in tendinosis).
B. Clinical correlation. The clinical approach to a knee injury (acute/chronic/overuse) depends on four cornerstones:
- History
- Physical examination
- Tests and their interpretations
- Treatment
II. APPROACH TO THE ACUTELY INJURED KNEE
A. History
- Mechanism of injury. This helps to identify potential structures that may have been damaged by the application of force, either direct (contact) or indirect (noncontact, i.e., a twisting mechanism, deceleration mechanism). If the injury was a contact injury, one should look for external signs at the point of force application and what structures might have been injured as that force continues. For instance, a blow to the anterior tibia might create upper tibial bruising. This force creates a posterior displacement of the tibia on the femur, potentially injuring the posterior cruciate ligament (PCL). Noncontact injuries frequently involve rotatory twisting motion; the lower limb remains fixed as the upper body twists around the knee.
- Was a pop heard or felt? A pop is frequently associated with tearing of a ligament, most commonly the anterior cruciate ligament (ACL), or a bone bruise.
- Return to play. The degree of pain and/or disability cannot be used as a reliable indicator of the seriousness of an injury. However, continued play with little or no impairment in performance diminishes the likelihood of a serious knee injury.
- Has the joint been previously injured? Frequently this question uncovers an acute on chronic injury. Two common examples are recurrent patellar dislocation and recurrent subluxation after initial ACL injury.
- Joint swelling. A knee joint effusion or swelling within 12 hours after an injury is, by definition, blood within the joint. An effusion that occurs after 12 hours suggests synovial fluid accumulation due to reactive synovitis, often due to cartilage or meniscus damage.
- In an acute knee injury, bloody effusion or hemarthrosis is indicative of a significant intraarticular injury.1 The differential diagnosis is as follows:
a. Ligament injury. The ACL and PCLs are intraarticular, although the PCL is extrasynovial. Rupture of the ACL is the most common cause of an acute hemarthrosis (70%). Injury to the PCL may result in a hemarthrosis, but often the posterior capsule is injured and blood does not remain within the knee joint. An injury to the deep medial collateral ligament (MCL) may result in interarticular bleeding, but this is less common. The lateral collateral ligament (LCL) is extraarticular and injury to this ligament does not result in hemarthrosis.
b. Peripheral meniscus tear. The outer, or peripheral, one-third of the meniscus is vascular, and a tear in this region results in a hemarthrosis. Meniscus tears in this zone have the potential for healing and are repairable. Tears in the inner two-thirds of the meniscus are more often associated with synovial irritation leading to a serous effusion that arises later (e.g., 24 to 48 hours) after the initial injury.
c. Fractures. Any fracture that involves the joint surface results in a joint hemarthrosis. In addition to obvious condylar/patellar fractures, occult osteochondral fractures can be a source of hemarthrosis. These can include avulsion fractures of the PCL and ACL (more common in developing adolescents) and fractures secondary to patella dislocation.
d. Synovial/capsular tears. Patella dislocations, even in the absence of fractures, are a source of hemarthrosis as the medial patellofemoral ligament (MPFL) and medial retinacular restraints are torn. Also, a significant contusion without a frank fracture or ligament/meniscus injury can create synovial bleeding. This is often considered a diagnosis of exclusion.
B. Physical examination
- Inspection
a. Effusion (joint swelling). An effusion usually indicates an intraarticular injury. The absence of a joint effusion often indicates an extraarticular injury. However, it is possible that a significant intraarticular knee injury results in capsular disruption and extravasation of fluid into the soft tissue.
b. Localized bruises and abrasions. These can be useful to identify the point of application of force in a contact injury. These can indicate the direction of the force that helps to indicate what structures may be injured.
2. Palpation
a. Careful palpation of the injured area can often result in an accurate diagnosis. The medial and lateral joint lines can be palpated and may indicate injury to the menisci. Palpation of the LCL and MCL can indicate the presence and anatomic location of the injury. Tenderness along the medial retinaculum or at the adductor tubercle on the femur may indicate a patellar dislocation. Careful palpation of the medial plica and pes anserine tendons can indicate overuse injury to these soft-tissue structures.
b. Lateral patella dislocation: This is associated with tenderness along the patella retinaculum, especially at the medial epicondyle where the MPFL inserts and/or along the superior medial portion of the patella. Note that although the patella dislocates laterally, it is the medial-based structures that are injured and thus are painful when palpated.
3. Range of motion. Range of motion is best assessed with the patient in the supine position. It should be compared with the contralateral knee. Lack of symmetrical hyperextension or full-flexion compared with the contralateral knee would indicate loss of motion. When the knee has an effusion, the knee’s resting position is around 30° of flexion (where potential capsular distention is largest).
a. A locked knee is defined as the inability to obtain full passive motion of the joint secondary to a mechanical block. This does not mean that the knee is in one position, but rather that there is an inability to obtain full motion, typically full extension. Common causes are a displaced meniscus tear or loose body.
b. A pseudo-locked knee is defined as the inability to obtain full range of motion secondary to pain or intraarticular knee swelling. A torn meniscus without displacement can result in pain at the limits of flexion and/or extension. If the patient’s knee “locks” in full extension and does not want to bend, the most common reason is an injury to the extensor mechanism, resulting in pain when the patient attempts to engage the kneecap in the trochlear groove.
c. Active range of motion assesses the integrity of the motor units surrounding a joint. Even in a severely injured knee, the patient typically retains the ability to lift his or her leg. Therefore, active straight leg raising and range of motion should be assessed. Frequently missed acute knee injuries are disruptions of the extensor mechanism, which include quadriceps tendon and patella tendon injuries. In this instance, the patient will generally be incapable of a straight leg raise, or the leg is raised with a notable extensor lag.
d. An extensor lag is the difference between active and passive ROM and signifies a disrupted extensor mechanism, muscular weakness, nerve injury, or muscular guarding do to pain.
4. Stability testing. The sine qua non of a ligament disruption is the presence of pathologic joint motion.
a. Single plane instabilities are the easiest to test. The tibia is moved in relation to the femur in four known planes. The amount of instability is graded according to the AMA classification: Grade 1, less than 5 mm of translation or opening; Grade 2, 5 to 10 mm; and Grade 3, more than 10 mm of translation or opening.2
- Medial instability or valgus opening is associated with injury to medial or MCL.
The main clinical motion test for providing an analysis of the severity of MCL complex injuries is a valgus stress test with the knee flexed at 30°.
- Lateral instability or varus opening is associated with injury to the lateral or LCL. The main clinical motion test for providing an analysis of the severity of LCL is a varus stress on the knee with the knee flexed at 30°. Typically injuries to the LCL also involve injury to the posterolateral complex. Motion tests to determine the amount of injury to the posterior lateral complex of the knee are the most complex of all knee examinations. It is beyond the scope of this manual.3
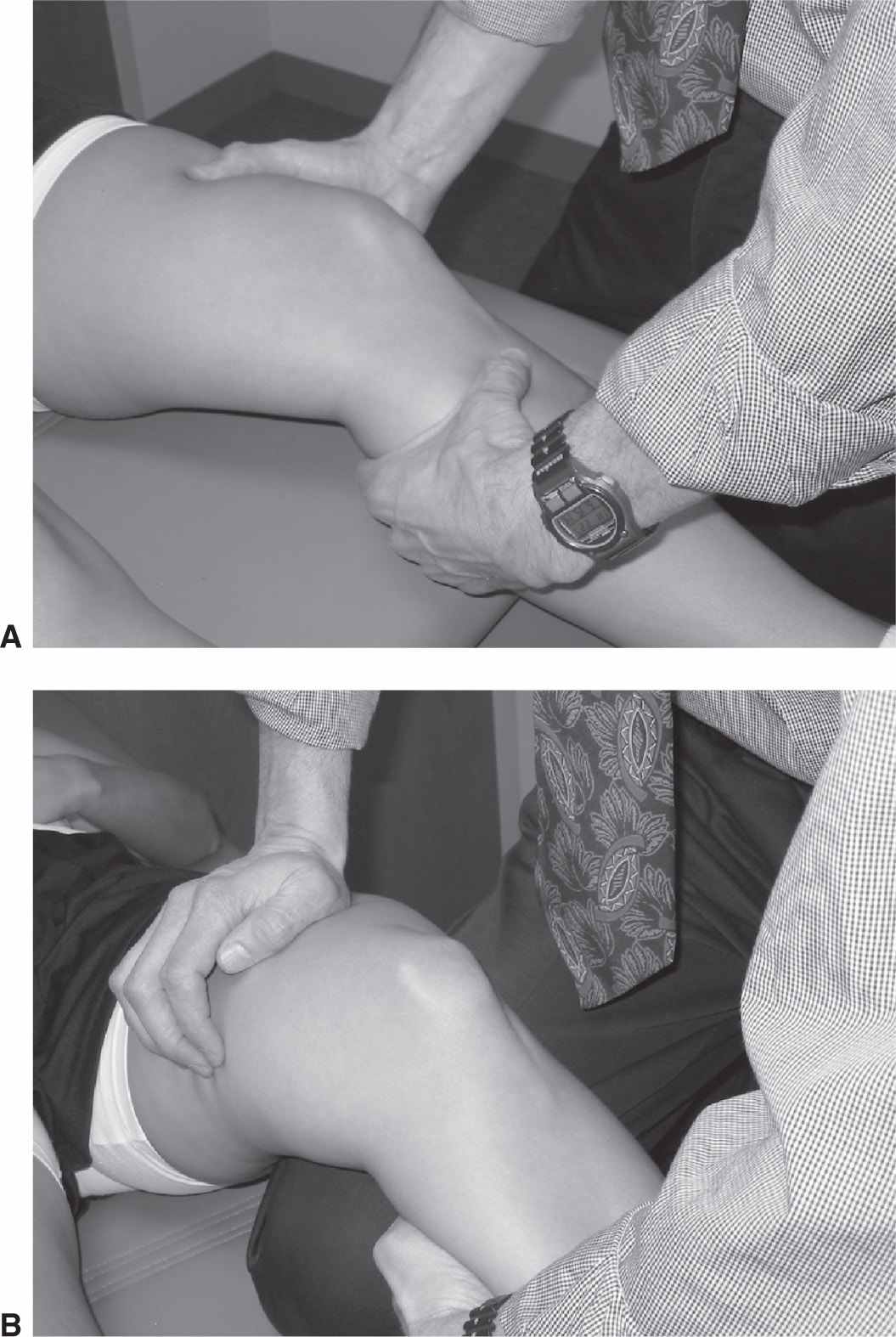
- Anterior instability is associated with injury to ACL. The main clinical motion test for an analysis of ACL injuries is the Lachman test (Fig. 25-1). This is performed with the knee in approximately 20° of flexion, with the leg in neutral rotation. Grading of displacement of the tibia on the femur is along the AMA guidelines. The anterior drawer test (done at 90° of knee flexion), although historically cited, has low reliability in the acute setting.4,5
Figure 25-1. Lachman examination of the knee: This is a test for deciding the degree of anterior translation of the tibia under the femur. The knee is held firmly in place at 20° to 30° of flexion by the examiner’s hand (A) or by resting the patient’s leg over the examiner’s knee (B). With a firm hold of the proximal tibia, the examiner places an upward or anteriorly directed force on the tibia, judging both the distance of translation and the firmness of the endpoint.
- Posterior instability is associated with injury to PCL. The main clinical motion test to detect injuries of the PCL is the posterior drawer test. This is performed by placing the knee at 70° to 90° of flexion. The key to this test is accurately assessing the starting point of the tibia.6
- Medial or lateral opening with the knee in full extension indicates injury to the collateral ligament as well as injury to either one or both of the cruciate ligaments.
(note: If you have straight plane pathologic motion of the knee in full extension, i.e., knee opens to valgus stressing, it signifies injury to one or both central posts, e.g., the cruciate ligaments.)
b. Rotary instabilities. This refers to the rotation of the tibia around its vertical or longitudinal axis (Fig. 25-2).
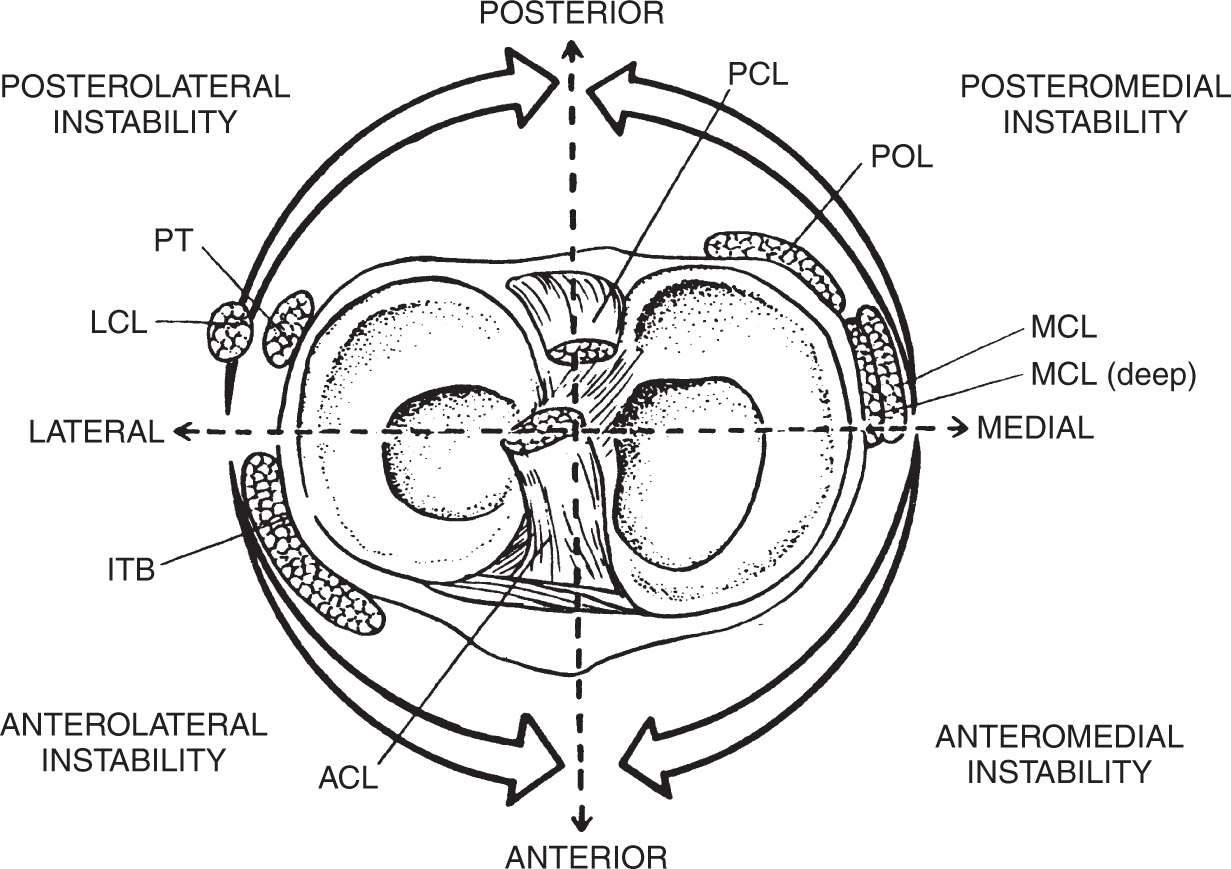
Figure 25-2. Rotatory instability of the knee. PT, popliteal tendon. (From Arendt, EA. Assessment of the athlete with a painful knee. In: Griffin, LY, ed. Rehabilitation of the Injured Knee. 2nd ed. St. Louis, MO: Mosby; 1990, with permission.)
- Anterolateral instability is associated with ACL injury. The test to determine anterolateral instability is the pivot shift test or Losee maneuver.7
- Posterolateral instability is associated with injury to the posterolateral corner (LCL, popliteal fibular ligament, popliteus tendon). Concomitant ACL or PCL injury is common with posterolateral instability. These are frequently associated with PCL and/or ACL injuries.
- Posteromedial injuries. These injuries are rare and involve injury to the PCL as well as the MCL.
- Anteromedial injuries are associated with ACL/MCL injuries.
c. Extensor mechanism instability
- Apprehension sign. Passive lateral movement of the patella causing pain and/or quadriceps contraction is suggestive of patellofemoral (PF) subluxation/dislocation. This maneuver is typically done with the leg in full extension, quadriceps muscles relaxed.
- Straight leg-raising against gravity confirms integrity of the extensor mechanism, including quadriceps tendon, patella, and patella tendon. A “lag” sign represents the difference between passive and active extension of the knee. A lag signifies disruption and/or weakness of the extensor mechanism.
- Medial/lateral patella restraints. Stability testing of the PF joint involves assessing the amount of passive patella motion in a medial and lateral direction of the patella. This is typically measured against an imaginary midline of the patella in the resting position (Fig. 25-3). This maneuver tests the static restraints of the medial and lateral extensor retinaculum complex. Any change from the patient’s “normal” measured against their uninjured contralateral knee is suggestive of extensor mechanism retinacular injury. Most particularly, an increase in lateral patella translation represents laxity or incompetence of the medial patella femoral ligament and medial retinacular structures associated with lateral patella dislocation.

Figure 25-3. Demonstrates one quadrant medial “glide.” The patella is divided visually into four quadrants. Holding the patella between the examiner’s thumb and index finger, the limits of medial and lateral motion are assessed and recorded as “quadrants” of motion. (From Halbrecht JL, Jackson DW. Acute dislocation of the patella. In: Fox JM, Pizzo WD, eds. The Patellofemoral Joint. New York, NY: McGraw-Hill; 1993, with permission.)
C. Tests and their interpretation
- Plain radiographs
The primary utility of plain radiographs is to evaluate the knee for bony injury. In addition, the presence of osteoarthrosis can be determined by looking at the cartilage space at the tibial-femoral articulation as well as the patella-femoral articulation.
a. Anterior/posterior view. This radiograph is obtained in the coronal plane. Standing views are preferred as they best assess tibial femoral joint space as well as knee alignment. If pain/swelling limits full extension and/or full weight bearing, supine views are performed but provide less information.
b. Lateral view is obtained in the sagittal plane. The lateral view allows evaluation of the caudad/cephalad position of the patella. Patella alta or increase in the cephalad position of the patella suggests a patellar tendon injury if it is asymmetric. Avulsion fractures of the ACL and PCL can often be identified on a lateral radiograph. Trochlea dysplasia is best viewed on the true lateral radiograph.
c. Axial view evaluates the position of the patella in its relationship to the femoral trochlear groove. Often, osteochondral fractures following a patella dislocation can be visualized on this view. Typically, one would see fragmentation of the medial patella facet and/or lateral femoral condyle in an acute patella dislocation (Fig. 25-4). Different axial views have been established (Laurin’s, Merchant’s).8 The clinician should become familiar with one technique. Axial views are a must for complete evaluation of all acute knee injuries.
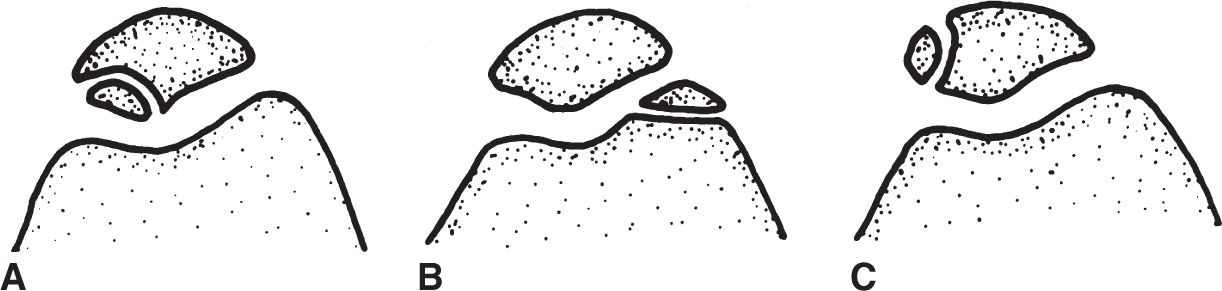
Figure 25-4. Three types of fractures associated with patella dislocation. A: Osteochondral fracture of the medial patella facet. B: Osteochondral fracture of the lateral femoral condylar. C: Avulsion fragment of medial patella femoral ligament off medial epicondyle (osseous-nonarticular). (From Halbrecht JL, Jackson DW. Acute dislocation of the patella. In: Fox JM, Pizzo WD, eds. The Patellofemoral Joint. New York, NY: McGraw-Hill; 1993, with permission.)
d. Rosenberg or PA view with a flexed knee is taken at 45° of flexion.9 This view is useful in determining early cartilage space, narrowing secondary to osteoarthrosis. This view is not typically obtained for an acute knee injury.
2. Magnetic resonance imaging (MRI) of the knee. MRI has its largest application in evaluating meniscus and cruciate ligament injury. The overall accuracy is greater than 90%.10,11 An MRI is typically an adjunct test in the evaluation of an acutely injured knee. It should be performed only if it will alter the treatment protocol and should be recommended by the physician who will be giving definitive treatment. It should never be used in the absence of a thorough and knowledgeable history and physical examination. Posterolateral knee structures are not well visualized in the standard MRI sequences and often require special technique for accurate assessment. In addition, articular cartilage integrity is not well assessed with standard MRI. However, recent techniques (e.g., gadolinium-enhanced, T2 mapping) and the use of more powerful magnets (3 Tesla) improve the accuracy of assessing articular cartilage injury.
3. Computerized tomography (CT) is useful in the evaluation of complex fractures about the knee. Tibial plateau fractures, certain patella fractures, and unusual femoral condyle fractures are best visualized with CT. Three-dimensional reconstructions can add additional information about complex fractures.
4. Stress radiographs can be extremely helpful in evaluating knee ligament injuries. They are often difficult to perform in the acute setting when patients have significant pain. However, in the subacute setting, they are useful to evaluate the degree of FCL and MCL injury. In addition, they can help evaluate the degree of PCL injury. In adolescence, stress radiographs may allow the diagnosis of physeal injury.
5. TcMDP bone scans are most useful in occult infections and to rule out stress fractures. Their usefulness in diagnosing reflex sympathetic dystrophy is variable. This is not a common diagnostic test prescribed for acute knee injuries.
D. General treatment
- Joint aspiration can be used to help evaluate and treat an acute knee injury. Aspiration or removal of a tense knee joint effusion can reduce pain and improve motion. In addition, the presence of fat droplets within the hemarthrosis can make the diagnosis of an intraarticular fracture. Aspiration also tends to be used in nontraumatic knee joint effusions to evaluate for infection, rheumatologic diseases, and crystalline deposit diseases.
- Immobilization/crutches. Knee joint immobilization with a brace or knee immobilizer is recommended until definitive diagnosis can be made. In addition, protected weight bearing with crutches should be utilized until a definitive diagnosis can be made. Care should be taken to avoid prolonged knee joint immobilization as this can result in muscle atrophy and knee joint adhesions.
- Reduction of swelling. Strategies to reduce swelling should be included in the initial treatment recommendation. These include activity reduction; ice; gentle, passive or active-assisted range of knee motion; elevation; and compression.
- Repeat examination is helpful in establishing a more firm diagnosis, especially when pain, swelling, and/or apprehension limit the initial examination.
- Medication: Tylenol should be the first-line medication to relieve pain in acute knee injuries. Nonsteroidal anti-inflammatory medications (NSAIDs) are commonly used to control pain and reduce swelling. However, NSAIDs do alter platelet function and may increase bleeding at the site of injury. In addition, NSAIDs may slow tissue healing by interfering with the normal inflammatory process. It is recommended that this class of medication be used judiciously and for short periods only.
III. SPECIFIC ACUTE KNEE INJURIES
A. Fractures of the patella
- Anatomic considerations. The patella is a sesamoid bone that is contained within the extensor mechanism. Its main function is to provide a lever arm for superior mechanical functioning of the extensor mechanism and to help stabilize the limb in deceleration. The strong quadriceps muscle tendon complex attaches to the superior pole of the patella and the stout patellar ligament connects the inferior pole of the patella to the anterior tibia.
- Common types of fractures
a. Transverse fractures, with or without comminution. These can be caused by direct or indirect trauma. They frequently are associated with disruption of the extensor mechanism and when displaced need to be surgically stabilized in order to regain the mechanical function of the extensor mechanism.
b. Vertical fractures of the patella frequently are because of a direct injury; infrequently they represent an overuse injury of the patella. When they are associated with no or minimal displacement, they do not constitute a disruption of the extensor mechanism and can be treated nonoperatively.
c. Chip fractures of the medial border are commonly seen with a patella dislocation; infrequently, they can be associated with direct trauma. This variety will be more thoroughly discussed under patella dislocation.
3. Treatment
a. Undisplaced or minimally displaced fractures may be treated symptomatically without surgery. However, they must be protected from further damage. Immobilization of the knee in extension with an immobilizer for 2 to 4 weeks is sufficient with weight bearing as tolerated. Quadriceps isometric exercises can be performed during this time. Gentle, passive range of motion as per the patient’s comfort level is recommended.
b. Displaced fractures involving the articular surface or compromising the extensor mechanism should be treated with open reduction and internal fixation. A tension band wire technique through cannulated lag screws is the treatment of choice.12
c. Comminuted fractures usually require surgical treatment. A partial patellectomy is necessary if the reduction and internal fixation of the fragments are not possible. If more than half of the patella remain intact, the comminuted pieces may be excised and the tendon sutured just above the subchondral bone into the remaining pole of the patella. Occasionally, fragments are large enough to fix with tension band wiring or 2.7-mm cortical lag screws.12
d. Osteochondral fractures often require arthroscopy for evaluation of the osteochondral fragment. These injuries are usually the result of a patellar dislocation. Large osteochondral fragments with viable bone should be fixed with careful reduction and internal fixation. Cartilage injuries are ominous for the future health of the joint; their treatment is beyond the scope of this text.13,14
e. Postoperative treatment must be individualized according to the type of fracture and the security of the repair. Most knees are initially placed in a compressive dressing with a posterior splint or knee immobilizer. If rigid internal fixation is achieved and the patient is trustworthy, early protective passive range of motion is initiated, progressing to active motion. Typically, 6 weeks of some form of immobilization is necessary for healing of the fracture(s). Quadricep muscle strengthening exercises, within the limits of the allowed knee motion, should be encouraged throughout this time.
f. The prognosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree