Knee Arthroscopy: The Basics
Alan L. Zhang
Christina R. Allen
DEFINITION
Knee arthroscopy is a minimally invasive video-assisted surgical intervention for intra-articular disease of the knee.
ANATOMY
The knee can be divided into three compartments: the patellofemoral joint, the lateral tibiofemoral joint, and the medial tibiofemoral joint.
The patellofemoral compartment is composed of the suprapatellar pouch, the patella bone, its femoral articulation (called the trochlea), the medial and lateral femoral condyles, and the medial and lateral patellofemoral ligaments.
The suprapatellar pouch is a potential space that develops when the knee joint is insufflated with fluid. Within this area, adhesions, plicae, and loose bodies may be found. Adhesions are commonly found with revision surgery.
Synovial plicae are bands of synovium that are remnants from fetal development. Their location and size may contribute to snapping sensations and inflammation within the joint. In the suprapatellar pouch, however, they most commonly provide a location for loose bodies to hide.
Suprapatellar plicae may partition an entire compartment within the pouch, leaving only a centralized hole by which loose bodies may gain entrance. These holes are called porta.
The patella is the largest sesamoid bone in the body. It has a medial and a lateral facet that articulate with its respective condyles. Centrally, there is an apex of the bone that sits in the trochlea.
The patella has the thickest cartilage in the body, which is used to withstand forces up to five times body weight.
With normal articulation of the patella on the femur, the cartilage of the medial facet touches the medial femoral condyle. This can be visualized with arthroscopy.
The patella begins to engage the trochlea at approximately 20 degrees and fully engages at 45 degrees. Lack of contact of the medial facet with the medial femoral condyle at these points in the range of motion suggests malalignment.4
The medial and lateral patellofemoral ligaments are thickenings of the medial and lateral retinaculum, respectively. They originate centrally on the patella and insert onto the medial and lateral epicondyles of the femur.
The medial patellofemoral ligament may become disrupted or attenuated with patellar dislocations. This may predispose to further dislocations, necessitating operative repair.
The lateral patellofemoral ligament and retinaculum are often released in efforts to restore patellofemoral alignment.
The medial tibiofemoral compartment is composed of the medial gutter and the tibiofemoral articulation.
The medial gutter is a fold of synovium in the posteromedial aspect of the joint where loose bodies may hide. Ballottement of this space is essential to ensure that no potential sources of pain exist within this region.
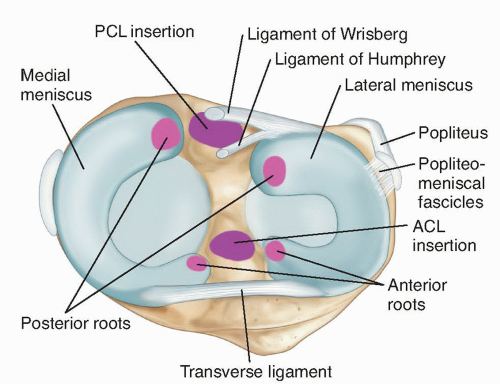
The medial tibial plateau is larger in the sagittal plane than the lateral plateau (FIG 1). It is a concave surface that articulates with a convex femoral condyle, but the plateau has a much flatter curvature than the femoral condyle. Given the relative incongruence, contact pressures are focused on a smaller surface area, leading to higher point contact stresses and cartilage degeneration.
The medial meniscus exists to alleviate this problem. The medial meniscus is a C-shaped structure on the perimeter of the medial tibiofemoral articulation. On cross-section, it is triangular, with the wider area along the periphery.
The meniscus provides better congruence between the two surfaces, participates in load sharing, and decreases point contact pressures throughout the articulation.
It is connected to the tibial plateau at the posterior and anterior ends at the meniscal roots. The deep medial collateral ligament attaches to the medial meniscus at its body centrally, providing stability. It is also attached to the capsule along its periphery.
The undersurface of the meniscus is not adherent to the plateau and can be lifted up, permitting inspection when one is suspicious of undersurface tears of the meniscus.
In the lateral tibiofemoral compartment, the meniscus is shaped more like an O than a C. It has a similar crosssectional anatomy as the medial meniscus, except it covers about 75% of the lateral tibiofemoral articulation. This is due to the geometry of the bony structures.
Although the lateral femoral condyle is quite similar to the medial femoral condyle, the lateral tibial plateau is substantially different.
The lateral femoral condyle and the lateral tibial plateau are two convex surfaces. To provide appropriate congruence, a larger meniscus is necessary.
The popliteus tendon inserts onto the posterior body of the lateral meniscus and provides stability to the meniscal body. It attaches to the meniscus by means of three popliteomeniscal fascicles: the anteroinferior, posterosuperior, and posteroinferior fascicles. Anterior and posterior to the insertion of the tendon on the lateral meniscus is a recess of the joint capsule that does not insert onto the periphery of the meniscus. This makes the lateral meniscus more mobile than the medial meniscus.
The two ligaments originate from the lateral meniscus, which travel anterior or posterior to the posterior cruciate ligament (PCL) prior to inserting on the femur. The ligament of Wrisberg travels posterior to the PCL, and the ligament of Humphrey travels anterior to the PCL.
Between the medial and lateral articulations is the intercondylar notch. It is a nonarticular portion of the knee that extends distally and posteriorly from the trochlea.
In the most anterior aspect of the notch lies the transverse meniscal ligament. This is a ligament that originates at the anterior horn of the medial meniscus away from the anterior root and inserts on the anterior horn of the lateral meniscus anterior to the anterior root.
The space between the transverse ligament and the anterior horn of the medial and lateral menisci can be mistaken for a tear of the menisci on magnetic resonance imaging (MRI).
There is significant bony variation in terms of the width of the intercondylar notch; this may contribute to the decision to perform a notchplasty or notch widening when performing an anterior cruciate ligament (ACL) reconstruction.
The ACL and PCL reside within the intercondylar notch.
The ACL originates at the posterolateral position (about 10:30 on a right knee and 1:30 on a left knee) of the inner wall of the notch and inserts centrally and anteriorly on the tibia. In the sagittal plane, it inserts slightly posterior to the anterior horn of the lateral meniscus and about 7 mm anterior to the PCL fibers.
The PCL originates from the anterior aspect of the medial wall of the notch and has a broad origination that begins at about 12 o’clock position and ends around 3:30 (on a right knee). This ligament travels posterior to the ACL and inserts centrally on the posterior aspect of the tibial plateau about 10 to 15 mm inferior to the joint line. The fibers run quite close to the posterior root of the medial meniscus and one must be careful not to deviate medially when débriding PCL remnants in this region during a PCL reconstruction.
SURGICAL MANAGEMENT
Preoperative Planning
Each patient is unique and the equipment needed for each surgery will vary. The surgeon must review the case specifics and studies before surgery and ensure that all necessary equipment is available when the surgery begins.
On the day of surgery, the surgeon should reconfirm with the patient the laterality of the procedure, “sign your site,” and verify that there has been no change in the signs and symptoms of the injury since the last office visit.
The surgeon performs an examination under anesthesia to reconfirm the diagnosis because this is crucial to understanding the nature of the injury. With sedation, the patient is more relaxed and able to give a more sensitive examination.
Positioning
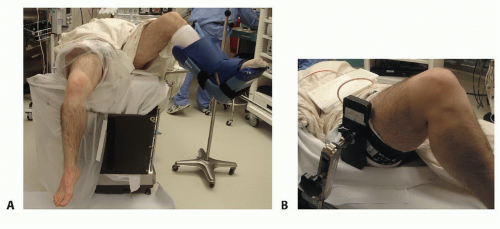
The patient should be supine and close to the edge of the bed.
The surgeon should verify that he or she will be able to get proper flexion of the leg should it be necessary to drop the foot of the bed.
The contralateral leg can be placed in a well-padded leg holder or secured to the bed with circumferential padding.
The use of a thigh holder versus a lateral post for arthroscopy is based on surgeon preference.
The thigh holder can be used with the foot of the bed dropped to 90 degrees, or the leg may be abducted and brought over the side of the bed (FIG 2A).
Commercial knee holders may not be capable of holding very large knees or pediatric knees. In these cases, a lateral post is preferred (FIG 2B).
Approach
The approach largely depends on what arthroscopic knee procedure is going to be performed.
Regardless, portal placement is the key to successful knee arthroscopy.
TECHNIQUES
▪ Portal Placement
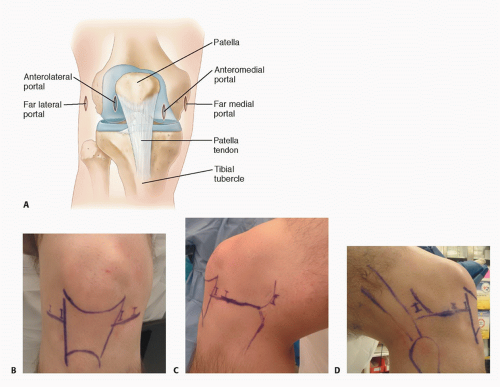
TECH FIG 1 shows the locations of the far lateral, anterolateral, anteromedial, and far medial portals and their relationships to landmarks of the knee.
Anterolateral Portal
Most arthroscopic visualization is performed through this portal.
It is created just lateral to the patella tendon. The incision is usually placed just inferior to the inferior aspect of the patella. Alternatively, the incision can also be referenced from the tibia.
The incision should measure 1 cm long.
Typically, the incision is made vertically, but some surgeons prefer a horizontal incision, which may theoretically decrease risk of injury to the infrapatellar branch of the saphenous nerve.
Anteromedial Portal
This is the primary working portal.
Its position is highly dependent on the work that needs to be done.
Traditionally, it is slightly more inferior than the anterolateral portal and just medial to the patella tendon, but the surgeon should be liberal about moving the location of this portal to optimize the surgical goals of the arthroscopy (ie, meniscal surgery vs. mosaicplasty).
The surgeon can use a spinal needle to localize the optimal portal placement under direct visualization before making the anteromedial portal incision.
Superomedial or Superolateral Portal
A superior portal can be placed either medial or lateral to the quadriceps tendon.
We prefer a superolateral portal because it results in less vastus medialis oblique inhibition.
This portal can be used as an inflow or outflow portal or to perform procedures in the suprapatellar pouch (ie, loose body removal, medial retinaculum plication, synovectomy, or evaluation of patella tracking).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree