CHAPTER 6 KNEE
A ONE-PLANE TESTS
Valgus test
Technique
Positive test
In full extension stability to the joint is afforded by the cruciate ligaments and laxity in this position is likely to represent major disruption to the knee and concurrent injury to the posterior capsule, posterior cruciate ligament (PCL) and possibly the anterior cruciate ligament (ACL) should be suspected (Malanga et al 2003, Slocum & Larson 1968).
Clinical context
Assessment of the subacute or chronic lesion allows the MCL injury to be graded (Bulstrode et al 2002, Kesson & Atkins 2005):
| Grade | Findings |
|---|---|
| Minor/grade I | Pain, tenderness and diffuse swelling with medial joint gapping of less than 5 mm on valgus testing with maintenance of the normal joint end-feel and a minimal suction sign (drawing in the skin over the medial joint line) signifies some MCL microfailure but no instability |
| Moderate/grade II | Pain, tenderness and local swelling with medial joint gapping of 5–10 mm on valgus testing with maintenance of the normal joint end-feel and a marked suction sign caused by moderate to major MCL tear. Minor ligamentous laxity does not usually result in serious functional instability unless the demands on the knee are high |
| Severe/grade III | Severe pain at the time of injury, significant swelling and possible haemarthrosis. Gapping of greater than 10 mm, with loss of the definite ligamentous end-feel, indicating a complete MCL rupture |
Although valgus stress is the most frequently used test in assessing injury to the MCL, the absence of an appropriate reference standard against which to measure the accuracy of mild injury or rupture has resulted in little evidence to support its use. Only one study reported a sensitivity of 86% for MCL tears using arthroscopy as a reference standard (Malanga et al 2003).
Clinical tip
| EXPERT OPINION | COMMENTS |
|---|---|
 | Valgus test |
| Used in every patient as a screening test for medial knee stability and pain. |
Varus test
Clinical context
Lateral or posterolateral knee injuries are relatively uncommon as the mechanism of injury usually requires an external impact (e.g. being hit by a car or a rugby tackle) to force the knee into an extreme varus position. In contrast to the MCL, the ligament is quite independent of the lateral capsule and meniscus which makes the structure less vulnerable to injury. The normal degree of varus is variable (usually around 7°) and should be compared to the normal knee if laxity is suspected. Stress X-ray showing a lateral opening of more than 8 mm is suggestive of a grade III injury (see ligament injury table, p. 184) and the likelihood of injury to the other posterolateral structures (cruciate ligaments, posterolateral capsule, arcuate–popliteus complex, iliotibial band) increases with the degree of abnormal varus movement detected (LaPrade & Terry 1997, Larsen & Toth 2005). Lateral instability, though much less common, is potentially more disabling than medial instability.
Varus stress tests the integrity of the LCL ligament. Although laxity noted on this test may indicate one-plane lateral instability, it is more likely to be positive where there has been injury to the other structures that contribute to posterolateral stability (Malanga et al 2003). If this is suspected, the posterolateral drawer test (see p. 205), dial test (see p. 209) or external recurvatum test (see p. 211) are considered to be more accurate in detecting posterolateral rotational instability (PLRI; Baker et al 1983). Conversely, a negative varus test does not rule out PLRI as an intact PCL contributes to varus stability in full extension and may limit varus excursion. In one large study, the LCL was found to be involved in only 23% of PLRI injuries (LaPrade & Terry 1997).
There is little evidence on the accuracy of any of the tests for the lateral structures of the knee primarily due to the absence of an appropriate reference standard. The clinical findings for lateral and posterolateral injuries of the knee are often subtle and, as a result, are more frequently misinterpreted (Hughston et al 1976).
Clinical tip
The test can be repeated with the knee in full extension and if instability is still detected, major disruption of the knee has occurred and injury to either the cruciates, popliteus or other lateral structures should be suspected along with injury to the LCL (Larsen & Toth 2005, Malanga et al 2003).
| EXPERT OPINION | COMMENTS |
|---|---|
 | Varus test |
| Used in every patient as a screening test for lateral knee instability. |
Posterior drawer test
Technique
Patient position
Supine with the hip flexed to 45°, the knee flexed to 90° and the foot placed on the couch.
Clinician position
The lower leg is stabilized by sitting on the dorsum of the forefoot. Both hands grasp around the upper tibia with thumbs placed anteriorly over the joint line with the thenar area of both hands positioned over the upper tibia. The fingers can also palpate the hamstring tendons posteriorly to ensure they are relaxed.
Clinical context
In a complete PCL tear, the average extent of posterior excursion of the tibia is 9.2 mm although incomplete tears will produce varied degrees of laxity (Hewett et al 1997). Injury of other stabilizing structures (i.e. arcuate–popliteus complex, posterior oblique ligament, iliotibial band) should always be considered as a potential source of pain and/or instability. Posterior excursion can be assessed and graded by measuring the amount of ‘step-off’ between the anterior tibial plateau and the femoral condyles (Larsen & Toth 2005).
| Grade | Amount of step-off between anterior tibial plateau and femoral condyles |
|---|---|
| 1 | Palpable step (approx 5 mm) |
| 2 | The normal anterior step is eliminated and the medial femoral condyle and medial tibial plateau are level |
| 3 | The medial tibial plateau is displaced posteriorly in relation to the medial femoral condyle resulting in a reverse ‘step off’. With this finding, posterolateral corner and medial injuries should also be considered |
The posterior drawer test is considered to be the most accurate test for diagnosing isolated PCL injuries but this has not been verified in studies examining its use as an isolated test. A high degree of sensitivity and specificity has been recorded where it is used as part of a composite assessment to determine PCL injury, particularly when complemented by other tests such as the posterior sag test (Malanga et al 2003); analysing the test in this context is helpful as it mirrors usual clinical practice.
Perhaps unsurprisingly, increased inter-examiner reliability has been noted in the presence of more significant grade II and III injuries (Rubenstein et al 1994).
Clinical tip
With an isolated tear of the PCL, the greatest degree of tibial excursion is noted at 90° flexion. Where the injury is located to the posterolateral corner, most excursion is found when the test is performed in 30°. In a combined posterolateral corner and PCL injury, increased posterior tibial movement will be noted when the test is repeated at both 30° and 90° flexion (Larsen & Toth 2005) and injury to other lateral stabilizers will be likely.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Posterior drawer test |
| A standard test used in all patients which accurately identifies PCL tears. |
Anterior drawer test
Technique
Positive test
Increased anterior excursion of the tibia accompanied by the loss of normal ligamentous resistance usually indicates significant injury. In a healthy knee, it is normal for approximately 6 mm of anterior tibial translation to be present (Magee 2008). If the ACL is injured in combination with the medial ligament/capsule, a much greater degree of anterior translation will be present (15 mm or more).
Clinical context
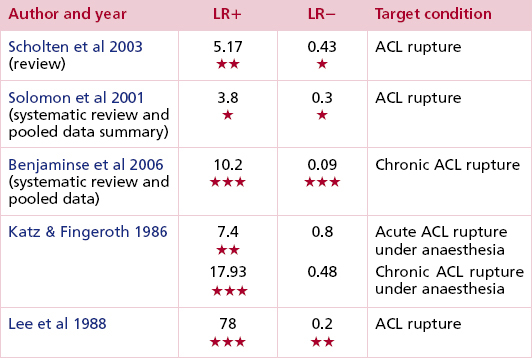
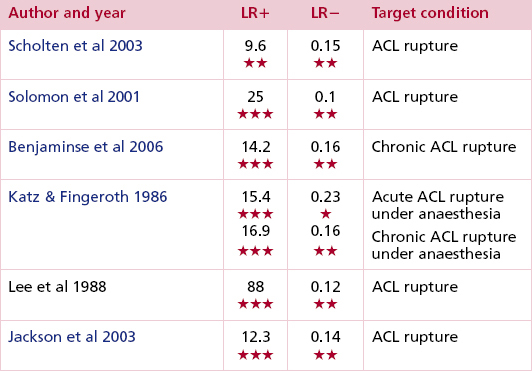
In an evaluation of the evidence around physical tests at the knee, a composite assessment (which included the anterior drawer test) was found to be more accurate than any one single test in diagnosing ligament and meniscal lesions (Solomon et al 2001). The test has also demonstrated a high degree of specificity (Jackson et al 2003) although doubts over its degree of sensitivity led other studies to conclude that the test should be secondary to the more sensitive Lachman (see p. 194) or pivot shift test (see p. 201) (Benjaminse et al 2006, Jackson et al 2003, Ostrowski 2006, Scholten et al 2003). It is an easier test to perform, however, and for the less experienced practitioner, the findings may be more helpful than trying to detect abnormalities with the pivot shift test. The sensitivity of all these tests improves when testing in the acute stages is avoided and they are used either when the patient is anaesthetized or in the subacute/chronic stage of the condition.
In the test position of 90° knee flexion, the MCL and posterior capsule provide secondary restraints to anterior tibial translation. If these structures are intact and the ACL is injured in isolation, the drawer test will be normal, leading to a false negative result. Other factors that can lead to a false negative result are hamstring spasm, a bucket-handle meniscal tear which blocks anterior translation of the tibia, or a partial ACL tear which has attached to the PCL during the healing process (Kim & Kim 1995). A false positive test can occur (increased anterior translation even when the ACL is intact) if the medial coronary (meniscotibial) ligament has been disrupted (Magee 2008). Increased anterior excursion of the medial tibial condyle should lead the clinician to conduct further multiplanar tests (see Slocum AMRI, p. 198) to establish the extent of the rotational instability. If a click or sudden shift accompanies a positive drawer test, suspicion of a concurrent meniscal tear should be aroused. The sudden movement or jerk is known as Finochietto’s jump sign (Magee 2008).
Clinical tip
If the posterior cruciate ligament has been injured it can be difficult to establish the normal starting position for this test. PCL laxity or rupture will cause the tibia to drop backwards (posterior sag sign, see p. 191) which then falsely leads to an apparent increase in anterior drawer. It is therefore necessary to eliminate a positive sag sign before recording an increase in anterior drawer.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Anterior drawer test |
| Useful as a secondary test if Lachman’s test is equivocal. |
Lachman’s test
Clinical context
This is a test for one-plane anterior instability and is the most sensitive physical test for diagnosing an isolated ACL injury. It was originally described by Torg but he named the test after his boss, Lachman (Torg et al 1976).
In studies using arthroscopy as the ‘gold standard’ for ACL diagnosis (Jackson et al 2003, Ostrowski 2006) Lachman’s test has been shown to be both more sensitive and specific compared with the anterior drawer (see p. 191) and pivot shift (see p. 201) tests. The Lachman test has also been found to be more accurate than MRI in the diagnosis of ligamentous injury (Kocabey et al 2004, Liu et al 1995, Rose & Gold 1996), a negative test thereby effectively ruling out complete ACL rupture (Scholten et al 2003).
The test is less sensitive where there is complex or acute injury (Frobell et al 2007, Yoon et al 1997) and, as with all ligament tests at the knee, is more sensitive when performed under anaesthesia (Kim & Kim 1995, Katz & Fingeroth 1986). Torg’s original study (Torg et al 1976) examined its use on patients with combined ACL and meniscal lesions and reported high levels of sensitivity, largely unaffected by the presence of bucket-handle tears. False negative results have been reported however, in cases where there is only a partial tear of the ACL, in chronic lesions where the injured ACL has adhered to the PCL, or where there is a concurrent meniscal injury sufficiently significant to prevent anterior translation of the tibia (Kim & Kim 1995).
In the test position, maximum tension is found in all portions of the ACL (Kim & Kim 1995). If instability is detected, stress X-rays can assist in grading the degree of injury (see below) although, in practice, clinicians are more likely to use their findings on examination to subjectively grade the degree of tibial translation.
| Grade | Amount of anterior tibial translation |
|---|---|
| 1 | < 5 mm |
| 2 | 5–10 mm |
| 3 | >10 mm |
Clinical tip
In the larger patient, the knee can be supported in the required flexed position over the clinician’s knee, making handling a heavy leg easier. The degree of anterior drawer can be palpated if the fingers of the outside hand are placed over the joint line while the tibia is drawn forwards.
The knee must be maintained in a degree of flexion throughout the test to reduce tension on the medial and lateral collateral ligaments and the iliotibial band, thereby minimizing their ability to restrain anterior movement of the tibia (Magee 2008). Lerat et al (2000) suggested that sensitivity of the test was improved by positioning the tibia in slight external rotation with the anterior translatory force coming from a posteromedial direction, as anterior translation of the medial compartment is thought to be a better indication of ACL deficiency in chronic tears than translation of the lateral compartment.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Lachman’s test |
| Extremely helpful, with a positive test confirming an ACL tear, but the range must be compared with the unaffected knee as this varies considerably in the normal population. |
B MULTI-PLANE TESTS
• Anteromedial rotatory instability (AMRI)
Slocum (AMRI) test
Technique
Patient position
Lying supine with the hip flexed to 45°, the knee flexed to 90° and the foot placed on the couch.
Clinical context
The sequence of injury originally described by Slocum & Larson (1968) started with rupture of the medial collateral ligament and medial joint capsule followed by the posterior oblique ligament. If the knee continues to rotate into further external rotation, especially if accompanied by a valgus force, strain then falls on the anterior cruciate ligament which will ultimately rupture if the force is great enough. With this degree of instability, abnormal loading of the medial meniscus over time will predispose the knee to further injury. Given the structures implicated in AMRI, other physical tests should be used to fully assess the stability of the knee (see Lachman’s test, p. 194; valgus test, p. 183).
The degree of instability can be graded with stress X-rays by measuring the extent of anterior subluxation of the tibia (Magee 2008) (see below) although, in practice, clinicians are more likely to use their findings on examination to subjectively grade the degree of tibial translation.
| Grade | Amount of anterior tibial translation |
|---|---|
| 1 | <12 mm |
| 2 | 12–20 mm |
| 3 | >20 mm |
Clinical tip
The tibia must not be fully rotated as this will tension the surrounding structures and could lead to a false negative finding. If abnormal external rotation is noted when placing the leg into the pre-test position, major disruption of the medial capsule and deep portion of the medial ligament should be suspected. Greater degrees of instability would also implicate injury to the more superficial layer of the medial ligament and ACL (Slocum & Larson 1968).
| EXPERT OPINION | COMMENTS |
|---|---|
 | Slocum (AMRI) test |
| There is a lack of evidence to determine relative sensitivities and specificities for this test and it is considered by clinicians to be insufficient, if used in isolation, to diagnose AMRI with confidence. It should therefore be employed alongside other instability tests. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree