The knee accounts for approximately 7% of all traumatic joint injuries. Recreational sports activities can lead to events that exceed the tolerance of stabilizing structures. There is a relative increase in the incidence of knee injuries due in part to an increasing participation in highly demanding recreational activities and a rising level of performance in these sports. At the same time, patients’ expectations have increased to the point where complete restoration of knee function is often expected. The physician must promptly determine whether conservative or surgical management is indicated.
The anterior cruciate ligament is frequently involved in knee trauma. This ligament plays a key role in the function of the knee. The importance of diagnosing damage to this ligament is obvious.
The sensitivity of diagnostic studies varies according to the examiner. Only 7–48% of initial examiners diagnose a tear in the anterior cruciate ligament upon clinical examination. Even a bloody effusion is not conclusive. Effusions occur in 23–65% of all meniscus injuries, but in over 60% of anterior cruciate tears.
Diagnosing degenerative changes in the knee is equally difficult. One is unlikely to assume the presence of “wear and tear” symptoms, particularly in young patients. In the absence of a history of trauma or occupational overuse, degenerative meniscus damage or cartilage changes are usually thought to be of secondary importance, and their sequelae are minimized.
In older patients precise diagnostic information is also crucial. The decision to perform total knee arthroplasty in the case of severe arthritis decisively impacts the patient’s life.
5.2 Clinical Examination
Standard Examination
The standard examination begins with taking the patient’s history. This permits differentiation between acute injury and possible degenerative changes, and provides initial clues as to the possible involvement of certain joint structures.
Inspect both knees from the front (contours, axes, position of the patella, muscular contour, and skin), from the side (leg axes for extension deficit, genu recurvatum, and position of the patella and fibular head), and from behind with the patient standing (swelling, muscular contour, and leg axes).
The rest of the examination should be performed with the patient supine. After a preliminary examination of the hip and ankle joints, palpate the patella and joint capsule. Watch for signs of inflammation such as warmth, swelling, and erythema. Next look for effusion, then palpate the medial and lateral joint space, fibular head, insertion of the patellar tendon, and the popliteal fossa.
Palpation is followed by range of motion tests (flexion/extension, external rotation/internal rotation with the knee extended and flexed). This can provide initial signs of locking and impingement syndromes. Document any crepitus, evaluate the rolling and gliding mechanism, and check the play of the patella. Observing the rotational motion can provide initial evidence of instability of the knee.
Continue the examination by assessing tenderness to palpation and evaluating the meniscus. Several tests should be used closely examine the patella, its adjacent structures, and the patellofemoral articulation. Pay careful attention to subluxation and retropatellar findings.
Next test stability. The anterior cruciate ligament is tested at 30° flexion (Lachman test) and at 90° (anterior drawer). This is followed by the pivot-shift test to evaluate the rolling and gliding mechanism. The posterior cruciate ligament is tested in a similar way.
The next step in the procedure is the evaluation of the collateral ligaments. This is done with the knee extended and flexed 20°–30°. Additional special tests should be used if signs of instability of the anterior cruciate ligament are detected. The examination is completed by assessing vascular supply and sensation in the affected leg.
Patient History
Every examination begins with taking the patient’s history. This provides information and helps establish a relationship of trust between examiner and patient. You should devote just as much attention to the patient in this initial conversation as in the subsequent physical examination. For very young and very old patients, information supplied by family members can be important.
| “Twelve commandments” for taking patient history | |
| 1 | Brief description of accident by patient |
| 2 | Time of accident |
| 3 | Precise mechanism of injury and specifics of type of sport |
| 4 | Tentative diagnosis specifying pattern of injury |
| 5 | Previous trauma or first injury? |
| 6 | Estimation of magnitude and direction of traumatic force |
| 7 | Behavior after trauma (ability to walk or participate in sports, feeling of instability, incarceration symptoms, swelling) |
| 8 | Previous therapy |
| 9 | Character of pain (time, duration, location) |
| 10 | Present pattern of symptoms (ability to walk or participate in sports, “giving-way” phenomenon, locking, swelling tendency, limited motion, signs of inflammation) |
| 11 | Estimation of patient’s expectations regarding diagnosis and treatment |
| 12 | Estimation of psychosocial background (personal need for bodily function, sense of responsibility, compliance, occupational situation) |
The patient will often find it difficult to describe the key aspects of his or her knee disorder in chronological order, therefore some structure will have to be provided. It is essential to record the therapy performed ; when inquiring about previous therapy, one should ask about measures undertaken by the patient (cooling, dressings, immobilization, and pain medication) as well as about previous treatments (injections, aspiration, medications prescribed, physical modalities, therapeutic exercise, and, if applicable, surgical intervention).
When taking the patient’s history, one should be alert to an accident or the sudden onset of atraumatic symptoms and should attempt to determine their chronological order. In acute trauma, one must differentiate between blunt and sharp external trauma and trauma without “action by an opponent.”
The history should be taken according to a scheme that follows the “twelve commandments” with respect to detail and documentation (Table 5.1). A differentiation should be made between sports, leisure, occupational, and traffic accidents. The elapsed time between the injury and the examination will decisively influence the findings. After the first 6–8 hours, expect to encounter reflexive splinting of the muscles during specific tests, which will make examination more difficult. Rarely, examination under anesthesia may be required.
| • Hyperflexion or hyperextension |
| • Varus or valgus stress |
| • Internal or external rotation |
| • Valgus stress in external rotation |
| • Varus stress in internal rotation |
| • Lateral and/or anterior impact |
Precise reconstruction of the mechanism of injury is extremely important. Generally, it will consist of a combination of rotation and abduction or adduction of the knee in flexion with the thigh or calf immobilized. The most frequent mechanisms of injury are valgus flexion with external rotation or varus flexion with internal rotation. Other mechanisms of injury can occur in isolation or in combination (Table 5.2).
Instability of the knee is classified according to the direction of motion of the tibia with respect to the femur. Nicholas (1973) classifies injuries to the capsular ligaments of the knee as: 1 simple, 2 complex, or 3 combined instability.
Information about the duration of symptoms and mechanism of injury (including the specific sport when applicable) will usually be sufficient for an accurate tentative diagnosis. Additional information about prior injuries and immediate post-injury events should be obtained.
The character, duration, and location of pain will provide helpful information. Displaced menisci can cause focal pain in addition to snapping or locking. A meniscus with degenerative changes and a small longitudinal or transverse tear will tend to cause deep, dull pain. A bucket-handle tear may cause pain at the end of the range of motion in flexion and extension. A partially torn cruciate in the acute phase can cause stabbing pain at rest, an isolated tear of the anterior cruciate ligament will tend to cause pain during exercise. Additional acute injuries may then cloud the picture.
An acute tear of the anterior cruciate ligament may show massive swelling that occurs immediately after trauma, persisting for up to 12 hours. Hemarthrosis may or may not be present. This massive swelling may not be present if the synovial membrane investing the anterior cruciate ligament is intact, if the anterior cruciate ligament had preexisting degenerative cruciate changes, or if the hemarthrosis drained through a capsular rupture. A useful piece of information from the history is the patient’s description of the “pop.” Many patients report a sound or sensation of some structure breaking, often heard by teammates and spectators in sporting events.
| Newborns Infants | Adolescents Young adults | Older patients |
| Congenital knee dislocation | Osgood-Schlatter disease | Quadriceps tendon tear |
| Discoid meniscus | Osteochondritis dissecans | Patellar tendon tear |
| Septic arthritis | Prepatellar bursitis | Degenerative bucket-handle tear |
| Osteomyelitis | Acute meniscus tear | Osteoarthhtis of the knee |
| Slipped epiphysis | Cruciate tear: ligamentous/bony | Synovitis |
| Chondrocalcinosis | Retropatellar arthritis | |
| Tendon disorders/tenosynovitis at the muscular insertions | Meniscus ganglia Chondromatosis | |
| Osteosarcoma | Baker cyst | |
| Recurrent patella dislocation | Aseptic osteonecrosis | |
| Sinding-Larsen-Johansson syndrome | Patellar degenerative joint disease | |
| Patellar chondrosis | ||
| Jumper’s knee | ||
| Runner’s knee |
The capability of the acutely injured knee can vary greatly. Some patients will immediately refrain from placing weight on the injured knee. Ambitious athletes, often influenced by their coach and teammates, will continue to participate and initially ignore the “giving-way” symptom that can occur with an anterior cruciate tear.
Personal impressions of the patient should not be underestimated. The patient’s description of all events will be colored by the situation in which the injury occurred. Patients with high demands, whether with respect to their occupation or sport, may minimize symptoms and expect a rapid return to the previous level of performance after minimal therapy.
In an acute exacerbation of a chronic problem or pain without specific trauma, it is important to inquire about occupational exposures and sports activities. Bent-knee activities can lead to early meniscus degeneration in association with cartilage damage. Overuse in track and field events, weight lifting, and martial arts may also lead to early symptoms that can occur during exercise and at rest. Inquiries should be made about previous treatments and partial successes.
Repetitive microtrauma causes characteristic symptoms in adolescents and older patients. Adolescents will complain of pain at the tibial tubercle during jumping in school sports. This may be a sign of Osgood–Schlatter disease or, in older adolescents, of “jumper’s knee.” Runners complaining of symptoms across the lateral side of the knee should be questioned for signs of tenosynovitis at the muscular insertions (biceps femoris and iliotibial tract) and overuse syndrome of the lateral collateral ligaments (“runner’s knee”). Changes in footwear and malalignment at the knee and ankle provide important information (Table 5.3).
Even in young adults, degeneration of previous meniscal injuries can produce sudden meniscus symptoms in the absence of a specific triggering
event. This condition may improve within a few hours of its onset. Often, arthroscopy will demonstrate a bucket-handle tear of the medial meniscus or a lesion of the posterior horn of the meniscus. So-called “snapping phenomena” may be encountered. These can be caused by intra-articular loose bodies or patellar subluxation. The semitendinosus tendons can cause such phenomenon medially, and the biceps tendon and iliotibial tract laterally. Bursal hypertrophy can exacerbate the snapping.
In older patients diffuse knee pain without trauma is almost always a sign of meniscus degeneration. Occasionally, minimal swelling and warmth will confirm the tentative diagnosis. Accompanying synovitis will almost always be present.
When retropatellar arthrosis is present, the patient will complain of pain when climbing stairs and walking downhill. In contrast, advanced osteoarthritis of the knee can lead to a feeling of instability with sudden episodes of the knee giving way for no apparent reason. The patient may then experience a stabbing pain as opposed to a dull, deep pain.
Patellar pain in young patients often occurs when climbing stairs or sitting for long periods. The “theater sign” (selecting an aisle seat to allow for knee extension) may be elicited.
Pain in the popliteal fossa is reported by patients with Baker cysts or posterior ganglia of the menisci. The patient experiences a sensation of tension with the knee extended, which may lessen with drainage of the cyst. This feeling of relief is temporary and is reduced as the cyst reforms.
Any uncharacteristic pain reported by the patient should be carefully investigated. Consider disorders of adjacent joints. Hip arthritis, for example, can produce thigh pains that radiate into the knee. Changes in the sacroiliac joint and lumbar spine can cause knee pain, as can limb-length inequalities and ankle deformities.
The history should include questions about vascular supply and sensation.
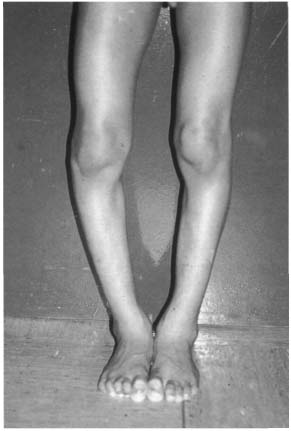
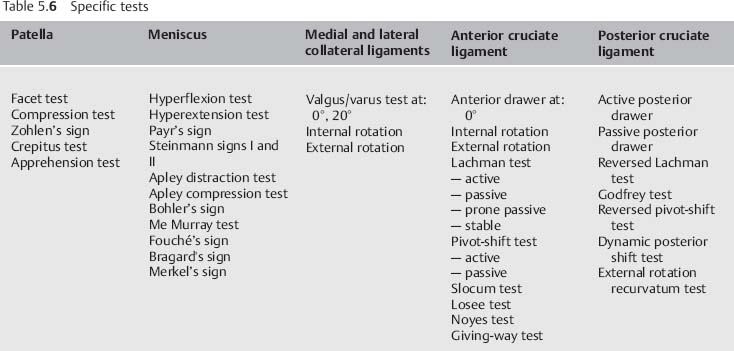
Figs. 5.1a, b Knee deformities: (a) genu varum, (b) genu valgum.
Finally, inquire about disorders of other organ systems to exclude causes of knee symptoms related to systemic diseases, such as diabetes mellitus, hemochromatosis, gout, hemophilia, hyperparathyroidism, thyroid condition, rickets, and psychogenic causes. The history should also) explore benign tumors such as exostosis, enchondromas, fibromas, osteomas, and bone cysts. It should explore the possibility of malignant tumors, neuropathic joint diseases such as poliomyelitis, tabes dorsalis, and syringomyelia, and the wide variety of rheumatic and infectious diseases.
If you suspect chronic rheumatic disease, inquire about involvement of multiple joints, symmetric distribution, and chronicity. The knee is affected in over 60% of rheumatic disorders. Further diagnostic studies should include various laboratory tests such as antinuclear antibodies or HLA-B27.
| • Inflammatory rheumatic joint disorders |
| • Collagen vascular disease |
| • Chronic inflammatory gastroenteritis with joint involvement |
| • Metabolic arthropathy |
| • Infectious arthritis |
| • Arthropathy resulting from coagulatory disorders |
| • Malignant tumors |
| • Arthritis |
The different diagnosis in monarthritis causes is broad (Table 5.4). Prior history is important; inquire about travel to foreign countries, the patient’s social environment, venereal diseases, previous injections, surgery, and injuries. Acute inflammatory knee diseases require immediate diagnostic studies and treatment.
The information obtained from a thorough patient history provides a guideline for subsequent diagnostic procedures.
Observation
Always be present to observe how the patient enters the examination room. If you wait until the patient has undressed and is lying on the examining table, you will miss important information about the patient’s gait, exertional ability, walking aids, single-leg stands, and knee flexion while undressing and getting on to the examining table. Information during this informal testing may be different from the information obtained during formal testing. This may be crucial in situations where disability, compensation, or litigation are involved.
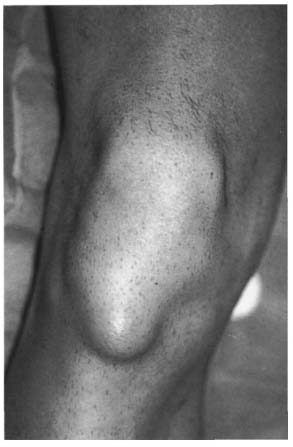
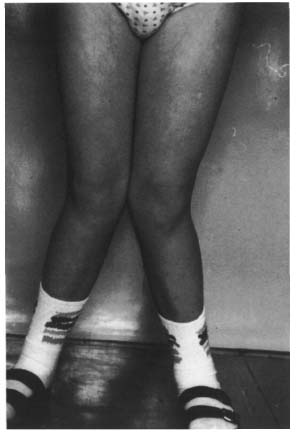
Fig. 5.2 Infrapatellar swelling indicative of prepatellar or infrapatellar bursitis.
Initial inspection should detect any external signs of injury that may indicate associated injuries. The presence of a traumatic arthrotomy is a surgical emergency. Watch for signs of contusion, hematomas, and open skin wounds.
Inspect the knee for contusion of the prepatellar bursa, even if the skin is intact, since it may require surgical excision.
Always inspect both knees for comparison. With the patient standing, inspect the anterior aspect of the knee (Figs. 5.1 a, b) forvarus, valgus, internal rotation, and external rotation deformities. Also check for any scoliotic changes in the spine, and evaluate muscle contour of the thigh and calf and changes in the popliteal fossa.
Inspection of the knee from the side with the patient standing will reveal flexion contractures of the hip and knee and ankle deformities.
Note any compensatory postures with pelvic obliquity, scoliotic curvatures, and abduction or adduction contractures of the hip. Document the position of the patellar and changes in the popliteal fossa.
With the patient supine, inspect the normal joint contour of the unaffected side in the absence of a bilateral disorder. This will serve as a reference for locating swelling in the superior recess (synovitis and exostosis), the parapatellar region (hemarthrosis or dislocation injuries), the medial or lateral joint space (meniscal ganglia or osteophytes), and the prepatellar region, patella tendon, tibial tubercle, pes anserinus, and fibular head (Fig. 5.2). Document any erythema and skin changes. Thickening of the retropatellar fat pad can produce a second prominence in the lateral aspect distal to the patella, known as the camel sign.
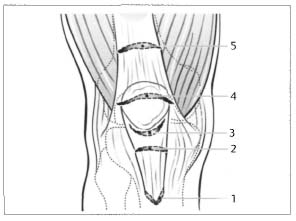
Fig. 5.3 Injury patterns of knee extensor mechanism. 1 evulsion of tibial tubercle; 2 intraligamentous rupture of the patella ligament; 3 proximal rupture of the patella ligament; 4 patella fracture; 5 rupture of the quadriceps tendon.
The position of the patella can indicate the presence of changes or previous trauma. Lateral displacement is a sign of patellar hypermobility and possible subluxation. An indentation proximal to the superior pole of the patella suggests a tear in the quadriceps tendon; extreme proximal displacement of the patella is indicative of a tear in the patella tendon. A transverse patellar fracture with a gap between the fragments can produce an indentation in the patella (Fig. 5.3). Patella dislocation with an abnormal prominence and an indentation between the femoral condyles is another diagnosis that can be made by inspection (Table 5.5).
Measurement of the Q. angle permits estimation of the lateral patellar displacement (Fig. 5.4). Measure this angle with the patient supine, placing a goniometer on the patella. The proximal arm points toward the anterior superior iliac spine and the distal arm points toward the tibial tubercle. A Q angle of up to 10° in males and up to 15° in females is normal. A wide pelvis, increased femoral anteversion, increased tibial external rotation, and genu valgum lead to an increased Q angle.
| • Quadriceps tendon tear |
| • Patella tendon tear |
| • Patella dislocation |
| • Transverse patellar fracture |
| • Complete dislocation |
| • Prepatellar bursitis |
| • Baker cyst |
| • Spontaneous posterior drawer with posterior cruciate ligament tear |
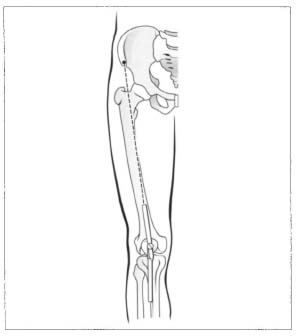
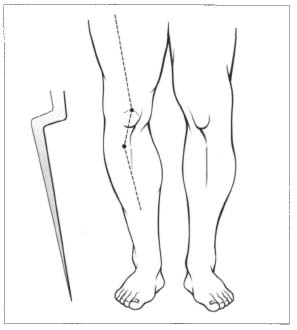
Fig. 5.5 The bayonet sign shows distal malalignment of the patella.
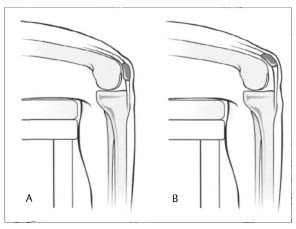
Fig. 5.6 A: Normal position of the patella with the knee flexed over the side of the examination table with the front of the patella facing straight ahead. B: In patella alta the patella is facing the ceiling.
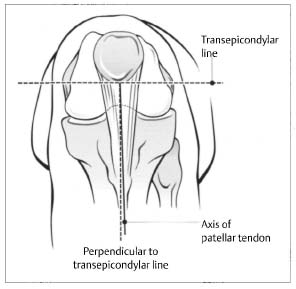
Fig. 5.7 In 90° of knee flexion the transepicondylar line is assessed. The axis of the patellartendon is compared to this line.
Pathologic internal rotation of the femur and external rotation of the tibia produce a particularly unfavorable deformity known as a bayonet sign (Fig. 5.5). This may be found in “malignant malalignment syndromes.”
A superiorly displaced patella (patella alta) will be apparent when the patient is sitting (Fig. 5.6). The tubercle sulcus angle can also be documented in the sitting position (Fig. 5.7). The patient flexes the knee 90°, forming an angle between the horizontal transepicondylar line and the axis of the patella ligament. This angle should be 0°; an angle exceeding 10° is regarded as pathologic.
Muscular imbalance between the vastus medialis and vastus lateralis can be detected by inspection. There may be noticeable atrophy of the vastus medialis. Patella tracking is readily discernible at about 45° of flexion. If there is evidence of muscular imbalance, this will be coupled with lateral displacement and patella tilt (Fig. 5.8). In such a case the patient will often exhibit a positive J sign in the dynamic examination. As the knee is extended from a flexed position, the patella forms a reverse J indicative of the predominance of lateral forces (Fig. 5.9).
Next inspect the musculature of the knee at rest and with isometric contracture. This can reveal new or older muscle fiber tears. Atrophy can be documented by comparing both knees. Generalized atrophy of a quadriceps leads to a visible decrease in the circumference of the thigh. This may be found in the presence of cruciate ligament insufficiency, meniscus injury, and retropatellar pain syndrome. Atrophy of the vastus medialis is typical of anterior cruciate ligament insufficiency. Irreversible muscle atrophy often occurs following arthrotomy with partial dissection of the quadriceps.
Additional information can be obtained by instructing the patient to demonstrate certain movements. For example with a tear in the quadriceps tendon the patient will be unable to lift the leg from a supine position. The active pain-free range of motion should be documented. This can deviate considerably from the passive range of motion. Evaluate the motion of the patella during tests. Impaired extension and, less frequently, impaired flexion can indicate injury to the meniscus and/or cruciate ligament with impingement. This should be differentiated from injuries to the soft-tissue envelope accompanied by swelling, intra-articular effusion, and loose bodies.
Finally, test for a spontaneous posterior drawer when the anterior margin of the tibia “sinks” back after an injury to the posterior cruciate ligament.

Fig. 5.8 Lateral tilting secondary to tightness in the lateral structures when looking from the front and below the right knee.
Preliminary Examination of the Thigh, Calf, and Adjacent Joints
Evaluation of knee function requires the examination of adjacent structures and joint because the pattern of stress acting on the knee depends on hip and ankle function. Abnormal stresses on the knee occur when the function of adjacent joints is impaired or their motion is limited. Abduction and adduction contractures of the hip place additional stresses on the medial and lateral compartments of the knee. Knee flexion contractures are often sequelae of hip flexion contractures or spine pathology.
If knee flexion contractures of unclear cause are present, the patient should be evaluated for neurologic disorders (spina bifida, cerebral palsy, and poliomyelitis) and congenital disorders and symptoms (arthrogryposis and Larsen syndrome).
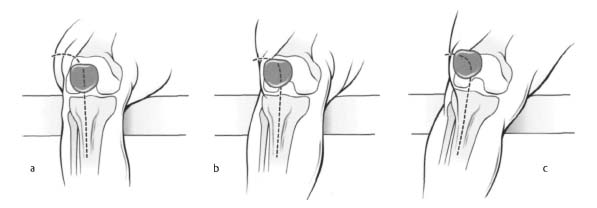
Fig. 5.9 When actively extending the knee from a 90° flexed position (A) to full extension (C) the patella describes an exaggerated inverted J-shaped course, which indicates predominance of laterally directed forces.
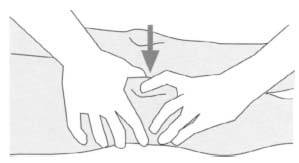
Fig. 5.10 Ballottable patella is indicative of an intra-articular effusion.
The function of the calf musculature should be examined and contractures evaluated. Initially muscular dystrophy may be present with calf muscle abnormalities.
Finally, the preliminary examination should include a vascular evaluation including arterial pulse, capillary refill, and venous drainage, as well as sensory examination in the lower extremity.
Palpation
Initial bodily contact with the patient is through palpation. We recommend palpating the unaffected knee first. Maintain eye contact with the patient when performing all manual testing. This will allow early detection of painful sensations.
First check the skin temperature, comparing both knees. Palpate swelling from proximal to distal. Palpation of the suprapatellar recess can reveal the presence of an intra-articular effusion, and swelling may be differentiated as synovitis, inflammation, or infection.
Palpating a ballottable patella is a further step in diagnosing an effusion. The synovial fluid is pressed from the recess under the patella. Experienced examiners can estimate the volume of the effusion to within 10–20 mL (Fig. 5.10).
Patellofemoral joint. Palpate the patella facets and check for tenderness. Evaluate the medial and lateral excursion of the patella. Tenderness at the medial facet of the patella is a sign of previous patellar dislocation. After tilting the patella, palpate the retropatellar aspects to obtain information about chondrosis. Evaluate the medial and lateral tilts of the patella. The femoral condyles should be palpated at the same time. Often this examination will reveal signs of avulsed fragments at the lateral condyles with local tenderness and crater formation and corresponding findings on the medial patella facet.
Local tenderness at the distal end of the patella can suggest “jumper’s knee.” Palpable hypertrophy of the retropatellar fat pad and a corresponding history will support this suspicion (Fig. 5.11).

Fig. 5.11 Palpating the tip of the patella and the proximal patellar tendon.
After palpating the patella tendon for swelling, thickening, and hardening, continue in the region of the tibial tubercle. In patients with occupational exposure, prepatellar bursitis and bursitis at the insertion of the patella tendon may be present.
Evaluate the continuity of the insertion of the quadriceps tendon when palpating the proximal end of the patella. A gap here suggests a tear in the tendon.
Document possible patellar hypermobility by comparing both knees. Perform this examination with the knees extended. With the palm of your hand on the knee, listen for audible and palpable crepitus when the patient flexes the knee.
Posterior aspects of the knee. With the knee extended, palpate the contours of the gastrocnemius and hamstrings. Palpate the pulse of the popliteal arteries in both knees. Tenderness in the popliteal fossa suggests a lesion of the posterior horn of the meniscus. Look for a Baker cyst that will usually be located posterolaterally. In rare cases, bursitis at the insertion of the biceps femoris or tumors in the surrounding soft tissue may produce palpable bulges in the popliteal fossa.
Tibiofibular joint. There are no characteristic findings upon palpation. The anatomical proximity of many structures renders diagnosis difficult. Tenosynovitis at the insertion of the iliotibial tract (runner’s knee) can make the tract appear hardened and tender. Differential diagnosis should include overuse of the lateral collateral ligament and tenosynovitis at the insertion of the biceps femoris, although this will usually cause localized tenderness above the fibular head.
Rotational stability should be evaluated in addition to tenderness to exclude a dislocation of the fibular head. A hematoma at the fibular head can be a sign of a tendon tear or proximal fibular fracture. In this case, damage to the peroneal nerve should be excluded (Fig. 5.12).

Fig. 5.12 Palpating the fibular head and the tibiofibular joint.
Medial aspect of the knee. Palpate the medial collateral ligament from proximal to distal. Tenderness at the medial femoral condyle is a sign of a lesion of the collateral ligament that is most frequently found proximally. Hardening from an older injury may also be palpable. Tenderness further distally suggests distal ligament lesions. To differentiate these from meniscus lesions, palpate further posteriorly.
In slender patients a palpable cord on the medial femoral condyle may correspond to a medial patellar plica.
To evaluate the cartilage, palpate the medial femoral condyle in maximum flexion. Focal soft spots will often be tender. Osteochondritis dissecans can appear as a crater.
Carefully palpate the joint space from anterior to posterior. Meniscal lesions are often detected as tenderness in the joint space. Degenerative changes such as osteophytes, cartilage lesions, or synovitis produce similar symptoms that duplicate meniscal lesion pain. Degenerative lesions of the posterior horn of the medial meniscus can produce tenderness at the posteromedial corner of the capsule.
Hypertrophy of the retropatellar fat pad will be palpable at the anterior medial joint space. A displaced meniscus will rarely project prominently; reduction will initially relieve the symptoms.
In the posteromedial area of the joint, tears of the posterior oblique ligament and tendinitis or bursitis of the semimembranosus may be palpable as swelling or fluctuation.
Distal to the medial joint space, examine the insertion of the collateral ligament for lesions. Further anteriorly, bursitis at the insertion of the pes anserinus may be seen as swelling.
Lateral aspect of the knee. Lesions of the proximal insertion of the lateral collateral ligament are rare. Despite this, the lateral condyle should be palpated to exclude such lesions.
The anterior sections of the lateral joint space should be examined for lesions of the lateral meniscus. These lesions will produce tenderness much less often then medial meniscus lesions. A palpable swelling not necessarily accompanied by meniscal symptoms is a characteristic finding with a lateral meniscal ganglion.
Next, palpate the posterior portions of the joint space. Injuries of the popliteus tendon are associated with complex injuries of the knee ligaments. Bursitis and tendinitis of the popliteus tendon are palpable as tender hardened areas on the distal posterior aspect of the lateral collateral ligament, and should be differential from corresponding changes to the biceps femoris tendon.
A lateral plica may also be palpated. A history of snapping phenomena will provide important information.
Continue the examination by palpating the lateral tibial plateau. Tenderness here could be an injury of the distal collateral ligament, iliotibial tract, popliteus muscle, or peroneal nerve, or irritation of the periosteum.
Assessing Range of Motion
Instructing the patient to move the knee provides information about the tolerated range of motion, as a patient will rarely exceed the discomfort threshold. Function of the muscles, specifically the quadriceps, in active motion can also be evaluated.
When evaluating passive range of motion, be alert to crepitus. Audible grinding sounds should be localized. Retropatellar friction suggests a cartilage lesion or patellar dysfunction in the trochlear groove. With advanced arthritis, “gear phenomenon” can often be documented by placing the palm of the hand on the knee. Severe cartilage destruction in the joint will produce visible steps in the pattern of motion.
The active and passive ranges of motion are documented. Individual differences, such as are to be expected between ballet dancers and bodybuilders, should be observed. Soft-tissue contractures may reduce the range of motion.
The patient will rarely be able to actively overcome a locked joint. A snapping phenomenon can occur when testing passive range of motion, for example in adolescents with osteochondritis dissecans and intra-articular loose bodies. These conditions can cause locking of the joint. Other cause of a snapping phenomenon in adolescents include subluxing patella and discoid lateral meniscus. In addition, meniscal and cruciate ligament tears can cause snapping or locking phenomena.
Locking phenomena in older patients tend to be caused by degenerative tears in the menisci, intra-articular loose bodies in arthritis and chondromatosis, and hypertrophic synovial tissue.
Pain at the end of the range of motion in flexion and maximum extension suggests a meniscal lesion.
Active and passive ranges of motion in external and internal rotation are assessed at various degrees of flexion. Thirty degrees of external rotation and 15° of internal rotation should be achieved. Excessive or restricted rotation requires examination of the lateral capsular ligaments and menisci. However, painfully restricted motion after injury is not specific to any single cause.
Figs. 5.13a, b Quadriceps contracture test. When attempting to press the heel against the buttocks (a) a gap may remain if the musculature is well developed and the quadriceps shortened (b).
Figs. 5.14a, b Rectus contracture test. Normal knee flexion of 90° (a) cannot be achieved if the rectus femoris is shortened (b).
As the joint is moved through its range of motion, a pivot shift can occur in the presence of severe instability. This phenomenon refers to anterior subluxation of the lateral tibial plateau as the joint nears extension. If the iliotibial tract and medial collateral ligament are intact, a pivot-shift phenomenon consistent with injury of the anterior cruciate will only occur when provoked by the examiner. In complex instability, pivot shift may be observed during the normal range-of-motion tests.
Muscle Elasticity Tests
The muscle are evaluated in conjunction with range-of-motion tests. In addition to evaluating individual muscle groups, note any shortening or contractures of the calf and thigh. Often adolescent patients will complain about patellofemoral pain during sports. Tightness in the quadriceps and hamstrings will increase patellar contact pressure and should be considered as a possible cause of such pain.
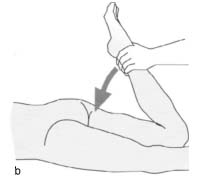
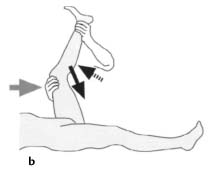
Evaluate the quadriceps with the patient prone. Passively flex the knee until the heel is positioned against the buttocks. This should be possible with both legs (Figs. 5.13 a, b).
If the quadriceps musculature is tight, it will not be possible to press the heel against the buttock and a gap will remain.
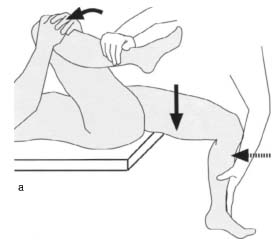
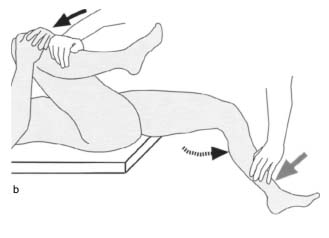
Test the rectus femoris and the hamstrings with the patient supine. To test the rectus, instruct the patient to hold the unaffected leg in maximum flexion. With the affected leg hanging over the edge of the examining table, passively flex the affected knee (Figs. 5.14 a, b). Normally, the knee can be flexed slightly more than 90°, allowing for hip extension. Shortening of the rectus femoris will result in flexion less than 90°. To test the hamstrings, lift the patient’s extended leg and document the degree of hip flexion attainable with lordosis of the lumbar spine neutralized. Angles less than 90° are regarded as abnormal. If the hamstrings are shortened, further hip flexion can only be achieved by bending the knee (Figs. 5.15 a, b).
Specific Tests
Systematically performing specific tests can verify tentative diagnoses. However, results of specific tests may also conflict with all previous findings (Table 5.6).
Figs. 5.15a, b Hamstring contracture test. If the hamstring muscles are shortened, the extended leg cannot be flexed 90° at the hip (a); this is only possible by flexing the knee (b).


Figs. 5.16a, b Evaluating lateral (a) and medial (b) patellar mobility.
Specific Tests for Patellar Disorders
Patellar tracking. The motion of the patella in the trochlear groove provides information about the ligaments and muscles guiding it. Grasp the patella with your thumb and index finger, and instruct the patient to slowly flex the knee from an extended position. Watch for patellar shift (lateral displacement) and tilt (vertical tilting). The test corresponds to radiographic positioning at 30°, 60°, and 90° of flexion for evaluating a lateral displacement tendency. Then observe patella tracking from the front during active flexion.
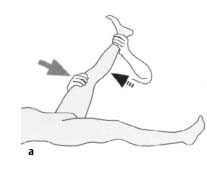
Patellar mobility. With the knee extended, evaluate the medial and lateral mobility of the patella (Figs. 5.16 a, b). This test should compare both legs in evaluating hypermobility as a possible cause of subluxation. Hypomobility is a sign of degenerative changes. Quadriceps contracture must also be considered when evaluating patellar mobility.
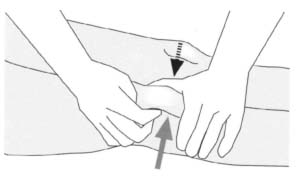
Fig. 5.17 Facet test. Elevating the lateral patellar facet.
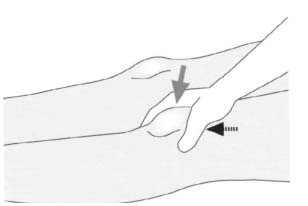
Fig. 5.18 Zohlen’s sign (patellar inhibition). The patella is displaced distally and the patient is instructed to tense the quadriceps.

Fig. 5.19 Payr’s sign. The cross-legged position produces pain at the medial joint space indicative of an medial meniscus lesion.
Facet test (Fig. 5.17). This test can detect retropatellar cartilage irritation. Tilt the patella to palpate beneath it. A painful reaction can often be provoked in chondromalacia or with a history of patella dislocation.
Compression test. A retropatellar cartilage lesion in the trochlear groove or synovial hypertrophy will cause a sensation of pain when pressure is applied to the patella.
Zohlen sign/patellar inhibition (Fig. 5.18). Grasp the proximal end of the patella with your thumb and index finger so that the web of skin in between is in contact with the patella. Move the patella distally while the patient actively tenses the quadriceps, pressing the patella onto the femoral condyles. This will be painful if cartilage pathology is present. This pain must be differentiated from pain that can be provoked in the manner described in a normal knee when the patient’s leg is lifted with the patella displaced distally.
Crepitus. Audible grinding phenomena occurring when the patient dynamically assumes a squatting position suggest advanced cartilage damage. This crepitus must be distinguished from medial and lateral compartment pathology.
Apprehension test for patella dislocation and subluxation. As with the apprehension test for anterior instability, this test is intended to reproduce patellar dislocation. Patient distress provides important diagnostic information. Previously described by Fairbank (1948), this test consists of attempting to dislocate the patella laterally with the knee extended, and progressively increasing flexion. Patients who have experienced previous dislocations will show apprehension and pain in their facial expression.
Specific Tests for Meniscus Disorders
Degenerative meniscus disorders often present with increasing pain in response to exercise. Minor trauma can often produce a tear in a chronically damaged meniscus. These specific tests are designed to determine the location, extent, and type of meniscus lesion.
Meniscus pain on pressure. Palpating the medial and lateral joint space with the patient’s knee flexed is very useful for evaluating a meniscus lesion. Often the only positive finding with a meniscus injury will be pain to palpation.
Pain at the end of the range of motion. Pain in the popliteal fossa at the end of the range of flexion suggests involvement of the posterior horn of meniscus. Hyperextension with stress applied to the anterior horns can produce corresponding pain; rubbery resistance to motion in partial flexion is a sign of displaced meniscus fragments.
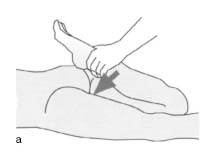
Payr’s sign. In a cross-legged position, pressing down on the thigh produces pain at the medial joint space with a medial meniscus lesion (Fig. 5.19).


Fig. 5.21 Apley compression test. Axial compression is applied in a grinding motion. Meniscal and chondral injuries will cause pain.
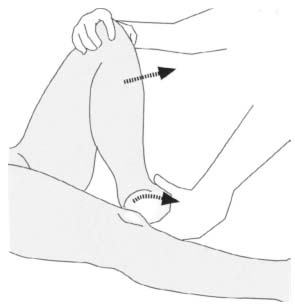
Fig. 5.22 McMurray test. The knee is extended from flexion and external rotation. Patients with injuries to the medial meniscus or medial ligaments will experience pain at the medial joint space.
Steinmann’s sign. Grasp the patient’s heel with one hand while fixing the knee against lateral motion with the other hand. For Steinmann’s sign I, perform forced external or internal rotation at various degrees of flexion. Pain at the medial or lateral joint space suggests involvement of the inner or lateral meniscus.
Steinmann’s sign II involves a painful pressure point that migrates posteriorly as flexion is increased.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree