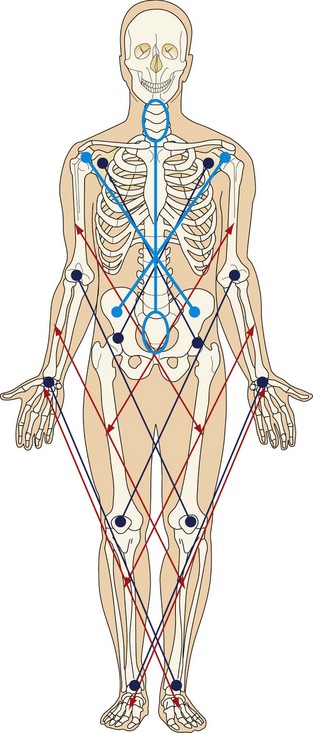
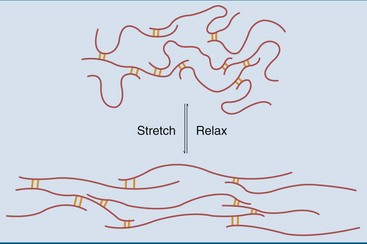
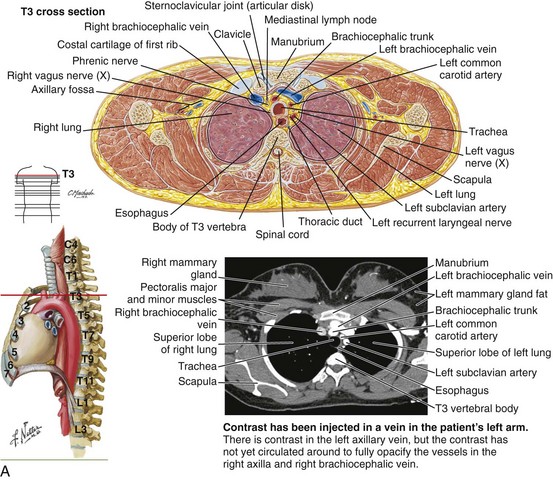
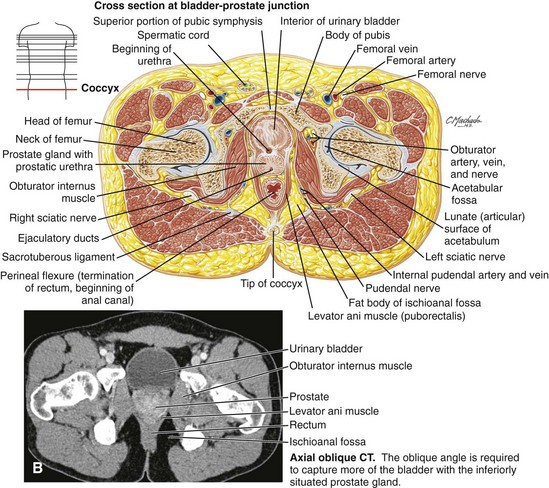
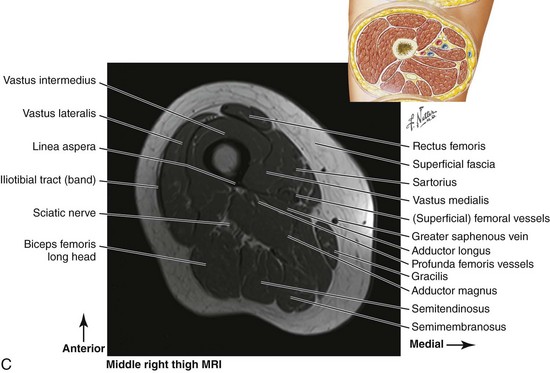
Chapter 4 After completing this chapter, the student will be able to perform the following: 1 Apply principles of kinesiology to sports massage outcomes. 2 Describe the relationship of connective tissue to normal and abnormal movement. 5 Demonstrate normal and abnormal range of motion. 6 Describe two types of joint stability. 7 Identify joint capsule fibrosis. 8 Explain response to synovial membrane injury. 9 Describe the structure and function of cartilage. 10 Identify the location of bursae and explain bursitis. 11 Explain joint degeneration. 12 Demonstrate joint mobilization. 13 Describe the structure and function of the muscle organ. 14 Demonstrate three types of muscle actions resulting in five types of function. 15 Explain the muscle length-tension relationship. 16 Describe five reflexive muscle actions. 17 Define kinetic chain and multiplanar movement. 18 Explain and locate four muscular functional subsystems. 19 Explain full-body pronation and supination. 20 Define serial distortion patterns and synergistic dominance. As mentioned in Chapter 1, it is expected that the fundamental elements of anatomy and physiology are in place, and that you, the reader, will take the next step toward understanding the real element of kinesiology, which is movement. Movement is a process for athletes. Athletic movement begins with a stable, strong, yet dynamic and flexible posture. Athletes are constantly balancing necessary stability and strength with flexibility and agility. • Stability is required to provide a stable base for functioning. Usually, stability concerns are focused on proximal musculature in the trunk, shoulders, and hips to allow for movement of the extremities. Stability is required before there can be balance. • Balance is the ability to execute complex patterns of movement with the right timing and sequencing. Balance is essential to motor function, as is the ability to maintain one’s center of gravity over the available base of support. • Coordination is the efficient execution of a movement. Usually, coordination involves motor learning and practice. • Endurance (lasting power) is based on efficiency and stamina. • Agility is the ability to move and change direction and position of the body quickly and effectively while under control. An important development in biomechanics research is the concept of the kinetic chain (also known as the kinetic link). This concept came out of mechanical engineering in the 1970s and was applied to biomechanics. The kinetic chain describes the body as a linked system of interdependent segments. By understanding their relationships to each other, we can maximize the effectiveness of massage application with an understanding of the importance of whole-body massage rather than isolated spot work. The diagram in Figure 4-1 illustrates the common areas of interrelated kinetic chain function. Follow the colored line to locate the interconnections. Chapter 3 presented the research on fascia. Now we will review and explore the relevance of the connective tissue anatomy and physiology to massage therapy application. Immobilization or lack of use decreases collagen production, leading to atrophy in the connective tissue and to osteoporosis in the bone. Without movement, collagen is laid down in a random orientation, with fibers packed close together and forming microadhesions. Adhesions are abnormal deposits of connective tissue between gliding surfaces (Figure 4-2). This atrophy with random orientation of fibers creates weakness in the tissue and instability of the associated joint. This condition is more common in those who are just beginning a fitness and performance regimen and increases injury potential. The aging process decreases the amount and quality of the collagen structure; therefore, exercise helps prevent age-related soft tissue dysfunction. Fascia is a fibrous connective tissue arranged as sheets or tubes. Fascia can be thick and dense, or it can consist of thin, filmy membranes. Fascia is connected throughout the body, creating a unified form. You can conceptualize fascia as duct tape or plastic wrap (Figure 4-3). However, we must remember that we now know that fascia is not a passive tissue. Research shows that fascia responds to and sends nerve signals. Recent research (see Chapter 3) indicates that there may be a proprioceptive component, as well as an active contractile component, to fascia based on myofibroblast cells and sensory receptors embedded in the fascia. We now know that fascia tone is more than thickness or thinness of the tissue and is controlled through neuroendocrine mechanisms. The implications for massage therapists, particularly sports practitioners, are significant because our approach to connective tissue function and dysfunction would be expanded. Along with methods used to produce increased pliability, length and slide application of massage would include nervous system functions as well. It is important to understand that at the same time that massage application is introducing mechanical forces such as tension and torsion forces into the tissues to change the more passive elements of fascia (i.e., ground substance, fiber alignment), the nervous system is also being stimulated. FIGURE 4-3 Fascia is connected throughout the body, creating a unified form. From head to foot, a continuum and unity are noted. A, Transverse view through thorax. B, Transverse view through hips and pelvis. C, Transverse view through thigh. (Netter illustration from www.netterimages.com. ©Elsevier Inc. All rights reserved.) Fascia functions by connecting, unifying, and separating structure while acting as a communication network based on the interconnect tensegric structure. Muscle fibers are embedded in fascia, not just wrapped in it, and a single muscle structure becomes a unified functional unit consisting of multiple muscles in an intertwined chain of a variety of fascia wrappings, tendons, ligaments, joint capsule structures, and periosteum, which are located up and down, spiral around, and flow through the body. Through these interconnected structures, the forehead is connected to the bottoms of the feet, the left wrist connects to the right ankle (and vice versa), and the left shoulder is connected to the right hip and down through the knee. Tom Myers calls these chains myofascial meridians (Myers, 2008). Information from the Stecco group describes the chains as myofascial units that function as uniting elements between unidirectional myofascial units (myofascial sequences), and as connecting elements between body joints through myofascial expansions and retinacula (myofascial spirals; Stecco at http://www.fascialmanipulation.com/englishhome32.html). Effectively focused massage can do the following: • Stimulate fibroblasts to repair the injured collagen • Introduce mechanical forces to realign the collagen fibers to their normal parallel alignment • Introduce mechanical forces to separate tissue layers to support sliding • Heat the tissue, affecting the fluidity of the ground substance • Stimulate fluid distribution throughout tissue layering to promote normal tissue gliding • Lengthen shortened tissue and increase ground substance pliability • Create controlled focused inflammation to increase collagen proliferation, especially in lax structures. Proper rehabilitation must be combined with this approach for a beneficial outcome. Otherwise, the result can be increased adherence and scar tissue formation. • Influence fascia tone related to myofibroblast contraction by changing the shape of tissue and altering autonomic nervous system function. Simply, contraction of muscles crossing the joint causes the joint to move throughout its range of motion. Each specific joint has a normal range of motion that is expressed in degrees (Box 4-1). However, we now know that it is not that simple. The pulling forces created by contracting muscle cells are embedded in connected functional units unified by spans of connective tissue structures that are individually called fascia, aponeuroses, tendons, ligaments, and so forth. More than individual muscles, joint movements are caused by the distribution of force throughout these tissues.
Kinesiology
Kinesiology
Connective Tissue
Collagen
Fascia
Joints
Kinesiology