K-Wire Fixation of Distal Radius Fractures with and without External Fixation
Christopher Doumas
Owen L. Ala
David J. Bozentka
DEFINITION
Distal radius fractures occur at the distal end of the bone, originating in the metaphyseal region and often extending to the radiocarpal and distal radioulnar joints (DRUJ).
Distal radius fractures can be classified as stable or unstable and extra- or intra-articular to assist in treatment decisions.
Fractures may angulate dorsally or volarly and may have significant comminution depending on the energy of the injury and the quality of the bone.
Percutaneous pins or K-wires, typically 0.062 or 0.045 inches, can be used for treatment of simple intra-articular or extra-articular fractures with mild comminution and no osteoporosis.
Percutaneous pins can aid reduction and stabilize the fragments in a minimally invasive manner.
Percutaneous pins can support the subchondral area of the distal radius and maintain the articular reduction in highly comminuted fractures, which is useful when combined with other fixation methods.
Smooth percutaneous pins may also be placed across the physis to maintain a reduction in children with minimal risk of a growth arrest.
Highly comminuted fractures are more difficult to fix rigidly and often require external and/or internal fixation to maintain alignment during healing.
External fixators can be hinged or static and may or may not bridge the wrist joint.
K-wire fixation of extra-articular and simple intra-articular fractures has received more support over the last few years after several prospective randomized trials comparing K-wire fixation to volar plating has shown no difference in outcome at 1 year.
ANATOMY
The distal radius consists of three articular surfaces: the scaphoid fossa, the lunate fossa, and the sigmoid notch.
Ligamentotaxis aids in the reduction of intra-articular and comminuted fractures.
Volar extrinsic ligamentous attachments include the radioscaphocapitate, long radiolunate, and short radiolunate ligaments.
Dorsal extrinsic ligamentous attachments include the radiotriquetral ligament.
Dorsal and radial to the second metacarpal lie the first dorsal interosseous muscle and the terminal branches of the radial sensory nerve.
The distal radial sensory nerve branches lie superficial to the distal radius and should be protected during dissection and pin placement.
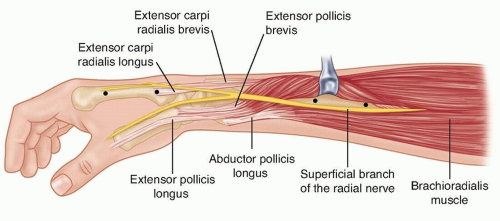
The radial sensory nerve emerges between the brachioradialis and the extensor carpi radialis longus (ECRL) muscle bellies (FIG 1).
The terminal branches of the lateral antebrachial cutaneous nerve lie superficial to the forearm fascia at the radial wrist.
There is a bare spot of bone between the first and second dorsal compartments in the region of the radial styloid.
The brachioradialis tendon inserts onto the radial styloid deep to the first dorsal compartment.
The ECRL and the extensor carpi radialis brevis (ECRB) lie dorsal to the brachioradialis in the second dorsal compartment.
Lister tubercle is dorsal, with the extensor pollicis longus (EPL) tendon on its ulnar side, in the third dorsal compartment.
The extensor digitorum communis tendons lie over the dorsal ulnar half of the distal radius in the fourth dorsal compartment.
The extensor digiti minimi lies over the DRUJ in the fifth dorsal compartment.
PATHOGENESIS
Distal radius fractures are the most common fractures of the upper extremity in adults, representing about 20% of all fractures seen in the emergency room.22
Mechanism of injury typically is a fall on an outstretched hand with axial loading, but other common histories include motor vehicle accidents or pathologic fractures.
Higher energy injuries cause increased comminution, angulation, and displacement.
Osteoporosis, tumors, and metabolic bone diseases are risk factors for sustaining pathologic distal radius fractures.
In children, fractures typically occur along the physis due to its relative weakness compared to the surrounding ligaments.
NATURAL HISTORY
Distal radius fractures needing no reduction and those that are stable after reduction typically recover functional range of motion with minimal long-term sequelae.
Two millimeters or more of articular surface incongruity of the distal radius can lead to degenerative changes, pain and stiffness.
Dorsal angulation can lead to decreased range of motion and increased load transfer to the ulna.
Radial shortening can lead to decreased range of motion, pain, and ulnar impaction of the carpus.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history of a fall on an outstretched hand is the most common presentation for a patient with a distal radius fracture.
Motor vehicle or motorcycle accidents and osteoporosis account for most comminuted fractures.
It may be clinically indicated to implement a workup for osteoporosis.
Pain, tenderness, swelling, crepitus, deformity, ecchymosis, and decreased range of motion at the wrist are typical symptoms and warrant radiographic evaluation.
Physical examination should include the following:
Inspection: Evaluate the integrity of the skin, cascade of the digits, direction of displacement, and presence of any swelling.
Identify points of maximal tenderness to differentiate between distal radius injuries and carpal or ligamentous injuries.
Palpate specific areas of the wrist and hand to differentiate distal intra-articular, DRUJ, and carpal injuries.
Two-point discrimination: Higher than normal (5 mm) results in the form of progressive neurologic deficit may signify an acute carpal tunnel syndrome or ulnar neuropathy.
Passive finger stretch test to assist with diagnosis of compartment syndrome.
EPL tendon function should be evaluated.
EPL assessment: Assess the resting position of the thumb interphalangeal joint and the patient’s ability to lift the thumb off of a flat surface to determine the continuity of the EPL tendon.
Palpation of forearm and elbow to assess for concomitant injury proximally
The DRUJ must be assessed for displacement and instability.
The bony anatomy must be carefully evaluated to avoid missing minimally displaced fractures, which may displace without treatment.
Skin should be assessed to avoid missing an open fracture.
Swelling should be monitored to allow for early diagnosis of compartment syndrome.
Sensory examination should be monitored for progressive changes, which may represent acute carpal tunnel syndrome.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographic evaluation should include posteroanterior (PA), lateral, and oblique views to assess displacement, angulation, comminution, and intra-articular involvement and allow for radiologic measurements.18, 22 Often, comparison x-rays of the uninjured wrist are helpful.
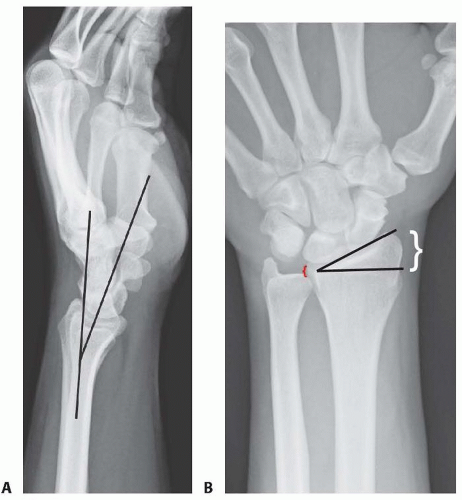
Lateral articular (volar) tilt is the angle between the radial shaft and a tangential line parallel to the articular margin as seen on the lateral view (FIG 2A). The normal angle is 11 degrees.
Radial inclination, measured on the PA view (FIG 2B), is the angle between a line perpendicular to the shaft of the radius at the ulnar articular margin and the tangential line along the radial styloid to the ulnar articular margin. The normal angle is 22 degrees.
Ulnar variance, also measured on the PA view (see FIG 2B), is the distance between the radial and ulnar articular surfaces. Ulnar variance is compared to the contralateral side.
Traction radiographs help assess intra-articular involvement, intercarpal ligamentous injury, and potential fracture reduction through ligamentotaxis.
Computed tomography (CT) scans are useful in fully elucidating the anatomy of the fracture, including impaction, comminution, and size of the fragments.
CT scans often significantly alter the original treatment plan.14
Magnetic resonance imaging (MRI) is rarely performed acutely but can diagnose concomitant ligamentous injuries, triangular fibrocartilage complex injuries, and occult carpal fractures.
DIFFERENTIAL DIAGNOSIS
Bony contusion
Radiocarpal dislocation
Scaphoid or other carpal fracture
Perilunate or lunate fracture-dislocation
Distal ulnar fracture
Wrist ligament or triangular fibrocartilage complex injury
DRUJ injury
NONOPERATIVE MANAGEMENT
Nonoperative treatment consists of splinting or casting for stable fracture patterns using a three-point mold.
Fractures amenable to nonoperative treatment include fractures that are stable after reduction with minimal metaphyseal comminution, shortening, angulation, and displacement.
Evaluation for secondary displacement weekly for 2 to 3 weeks is critical as the swelling subsides.
Unstable patterns will displace if not surgically stabilized.
There is little role for nonoperative treatment in highly comminuted fractures.
The physiologic age, medical comorbidities, and functional level of the patient should be considered in determining the need for surgical treatment.
Early range of motion of the nonimmobilized joints is essential in the nonoperative treatment of all fractures near the wrist to prevent contracture.
The cast or splint must not extend past the metacarpophalangeal joints so as to allow digital motion.
SURGICAL MANAGEMENT
Surgical treatments are indicated to prevent malunion and improve pain control, function, range of motion, and to decrease the time of return to function.
Surgery is reserved for unstable fractures, including displaced, intra-articular, comminuted, or severely angulated injuries and fractures that displace following attempted closed management.
Percutaneous pinning can assist in obtaining and maintaining reduction of displaced fractures with limited comminution in a minimally invasive manner.
External fixators maintain radius length but cannot always control angulation and displacement; therefore, supplementation with percutaneous pins is typically performed.2
Conversely, external fixators may augment percutaneous pins and plate fixation when extensive comminution is present.
Supplemental external fixation should be considered for fractures with comminution of over 50% of the diameter of the radius on a lateral view or when significant volar cortical comminution is present.
External fixation may be used as a neutralization device because the distraction forces decrease soon after fracture reduction.
External fixators also are useful for “damage control orthopaedics” to temporarily stabilize wrist fractures, especially for complex, combined, open injuries.
For nonbridging external fixation, there must be at least 1 cm of volar cortex intact and adequate fragment sizes to allow proper pin placement.
A relative contraindication to pin fixation with or without external fixation is a volar shear injury, which should be reduced and stabilized using a volar plate and screws.
Preoperative Planning
All radiographs should be reviewed before surgery and brought into the operating room.
Analysis of the pattern and presumed stability of the fracture fragments determines whether percutaneous fixation, with or without external fixation, is suitable.
For intra-articular fractures, the specific fragments to be reduced and fixed must be identified preoperatively to avoid incomplete reduction of the joint surface.
The surgeon must be prepared to change his or her management decision intraoperatively if the fracture behavior is different from anticipated. A variety of fixation devices should be available in the operating room.
Positioning
The patient is positioned supine on the operating table with a radiolucent arm board.
A tourniquet is applied near the axilla with the splint still in place (FIG 3).
Fluoroscopy should be used for confirmation of reduction and fixation throughout the procedure.
There must be enough range of motion of the shoulder and elbow to allow standard anteroposterior (AP), lateral, and oblique images.
Approach
Various approaches can be used in the application of external fixators and the insertion of percutaneous pins.
Distal external fixator half-pins may be placed directly into the second metacarpal or into other carpal bones (for injuries
including the second metacarpal). Wires and half-pins from nonbridging fixators may be placed in the distal radius itself.
Percutaneous pins can be inserted through the radial styloid between the first and second dorsal compartments, through Lister tubercle, through the interval between the fourth and fifth dorsal compartments, and across the DRUJ (FIG 4).
Caution is taken to avoid skewering tendons and nerves and to avoid penetrating the articular surface.
TECHNIQUES
▪ Closed Reduction of a Distal Radius Fracture
Closed reduction should be performed before fixation using a combination of distraction and palmar translation of the distal radius fragment and carpus.1
Use of a padded bump or towel roll will aid in the reduction (TECH FIG 1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree