Chapter 3 Joint Assessment Principles and Procedures
The doctor of chiropractic views the human being as a dynamic, integrated, and complex living thing who has an innate capacity for self-healing.1 2 3 4 5 6 Chiropractic health care focuses on the evaluation and treatment of neuromusculoskeletal (NMS)-based disorders, but does not disregard the multiple potential causes of ill health and the complex nature of health maintenance.7,8
In keeping with this philosophy and the responsibility as “portal-of-entry” health care providers, chiropractors must maintain broad and thorough diagnostic skills. The Council on Chiropractic Education (CCE) defines the primary care chiropractic physician as an “individual who serves as a point for direct access to health care delivery; the doctor of chiropractic’s responsibilities include (1) patient’s history; (2) completion and/or interpretation of physical examination and specialized diagnostic procedures; (3) assessment of the patient’s general health status and resulting diagnosis; (4) provision of chiropractic care and/or consultation with continuity in the co-management, or referral to other health care providers; and (5) development of sustained health care partnership with patients.”9 Before applying therapy, the chiropractor must first ascertain if there is a clinical basis for treatment. The chiropractic physician who chooses to limit therapeutic alternatives must still possess the skills necessary to determine if patients seeking their care have a health problem responsive to the specific treatments they provide.10 This dictates that chiropractors be trained to screen and evaluate a broad range of complaints if they wish to maintain their primary contact privileges. Diagnostic skills must have sufficient depth to screen all organ systems of the body for those conditions that are and are not amenable to chiropractic treatment. The social expectation and regulatory requirement of a primary contact provider are to provide a suitable health status assessment and initial clinical impression regardless of the patient presentation or the health care professional’s particular discipline, philosophy, or theories.
The manipulable lesion
Manual therapy has been proposed as an effective treatment for a wide variety of conditions, but it is most commonly associated with disorders that have their origins in pathomechanical or pathophysiologic alterations of the locomotor system and its synovial joints. As a result, manual therapy is based on assessment procedures that take into consideration both functional and structural alteration of the NMS system. Haldeman11 has referred to this process as the identification of a manipulable lesion. Spinal manipulation is thought to act on this manipulable or functional joint lesion, but given the historical presumption of this entity, it is somewhat surprising that there is not more information on its pathomechanical properties.12 The lesion is viewed as a set of possible individual maladies responsible for the patient’s symptoms.13,14
A diagnosis of joint dysfunction syndrome identifies local altered mechanics, but it does not identify the underlying nature of the dysfunction. Although joint derangements may present as independent clinical syndromes, they are more commonly associated with other identifiable disorders and injuries of the NMS system.15 16 17 18 19 20 21 22 23
Determination of the appropriateness of adjustive therapy should not be based on the presence of a fixation, malposition, or spinal listing alone. The cause of the altered mechanics indicates whether adjustive therapy or some other form of therapy is in order.23
Subluxation
Within the chiropractic profession, the manipulable lesion has been equated primarily with the term joint subluxation. The concept of subluxation is a central defining clinical principle and the source of contentious debate and disagreement within the profession.24 Mootz suggests that the chiropractic profession’s attention to subluxation (pro and con) is found in virtually every dimension of the profession’s existence, be it clinical, scientific, philosophical, or political.25 He identifies four distinct ways that subluxation is used by the profession, each with merits and liabilities. They are25:
Historically, joint subluxation was defined predominantly in structural terms.1,2,23,26 27 28 29 30 The founder of chiropractic, D.D. Palmer, defined joint subluxation as a “partial or incomplete separation, one in which the articulating surfaces remain in partial contact.”31 Central to Palmer’s original subluxation hypothesis was the concept that vertebral subluxations could impinge on the spinal nerve roots (NRs) as they exit through the intervertebral foramina. This was postulated to obstruct the flow of vital nerve impulses from the central nervous system to the periphery and to induce lowered tissue resistance and potential disease in the segmentally innervated tissues.1,2,8,29,31 32 33 34 35 Palmer went so far as to suggest that the primary cause of all disease could be related to subluxations and interruption of normal “tone—nerves too tense or too slack.”1,8
The most impassioned supporter of this concept was D.D. Palmer’s son, B.J. Palmer. Throughout his career, B.J. Palmer ardently promoted a monocausal concept of disease,8,27,28,36,37 specifically stating that chiropractic is “a science with provable knowledge of one cause of one disease being an internal interference of the internal flow of abstract mental impulses or nerve force flow supply, from above down, inside out.”36
Although the profession today emphasizes the important relationship between health and the structure and function of the NMS system,4 5 6 7 32 33 34 3538,39 it does not promote a monocausal concept of subluxation-induced disease.7 8 9 10 37 38 39 40 The monocausal concept runs contrary to much of the profession’s recent literature24,34,35,37 38 39 and to the view held by the overwhelming majority of practicing chiropractors.8 Although a small minority of chiropractors still promotes this extreme view, both the profession’s national associations and the CCE have disavowed it.9,39
Beginning with the published work of Gillet,41 42 43 44 45 46 Illi,47 and Mennell,48,49 and later through the writings of Sandoz23,30,50,51 and Faye,52,53 the importance of the dynamic characteristics of joint subluxation moved to the forefront. As a result, joint integrity was defined not only in structural terms but also in functional terms.23,30,34,35,42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 Within this context, joint subluxation took on a broader definition, and joint malposition became a possible sign of disturbed joint function, not absolute confirmation.
This view provides a more dynamic perspective and suggests that minor joint misalignment does not necessarily predict the presence or absence of joint dysfunction or the direction of possible restricted movement.23,30,50 51 52 53 54 From this perspective, joints do not have to be malpositioned to be dysfunctional. Joint fixation can occur with the joint fixed in a neutral position, or it can have multiple planes of joint restriction.23,30,50,57,58 Consequently, treatment decisions concerning adjustive therapy and adjustive vectors, once based predominantly on the direction of malposition, grew to incorporate an assessment of the functional status of the patient including an assessment of joint mobility.41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 Today, consideration is given to both the static and dynamic components of spinal dysfunction, including presence or absence of joint pain with loading (joint provocation/challenge).23,32,34
Other health care providers within the field of manual medicine also struggle with multiple definitions and explanations for manipulable lesions.59 60 61 62 63Box 3-1 contains a list of terms and definitions commonly used to describe functional or structural disorders of the synovial joints. A common principle behind all of these concepts is that there is a somatic component to disease and that dysfunction of the NMS system can affect a patient’s overall health status as well as the ability to recover from injury and disease.
BOX 3-1 Terms Describing Functional or Structural Disorders of the Synovial Joints
Subluxation
The alteration of the normal dynamic, anatomic, or physiologic relationships of contiguous articular structures56; a motion segment in which alignment, movement integrity, or physiologic function is altered, although the contact between the joint surfaces remains intact60; an aberrant relationship between two adjacent articular structures that may have functional or pathologic sequelae, causing an alteration in the biomechanical or neurophysiologic reflections of these articular structures or body systems that may be directly or indirectly affected by them.10
Subluxation syndrome
An aggregate of signs and symptoms that relate to pathophysiology or dysfunction of spinal and pelvic motion segments or to peripheral joints.60
Subluxation complex
A theoretic model of motion segment dysfunction (subluxation) that incorporates the complex interaction of pathologic changes in nerve, muscle, ligamentous, vascular, and connective tissues.10
Joint dysfunction
Joint mechanics showing area disturbances of function without structural change—subtle joint dysfunctions affecting quality and range of joint motion. Definition embodies disturbances in function that can be represented by decreased motion, increased motion, or aberrant motion.61
Somatic dysfunction
Impaired or altered function of related components of the somatic (body framework) system; skeletal, arthrodial, and myofascial structures; and related vascular, lymphatic, and neural elements.62
Osteopathic lesion
A disturbance in musculoskeletal structure or function, as well as accompanying disturbances of other biologic mechanisms. A term used to describe local stress or trauma and subsequent effects on other biologic systems (e.g., effects mediated through reflex nerve pathways, including autonomic supply of segmentally related organs).63
Joint fixation
The state whereby an articulation has become temporarily immobilized in a position that it may normally occupy during any phase of physiologic movement; the immobilization of an articulation in a position of movement when the joint is at rest or in a position of rest when the joint is in movement.30
Vertebral subluxation complex
Because of continued professional debate and increasing scientific inquiry, a trend toward viewing subluxations as complex clinical phenomena has unfolded.* Rather than a condition definable by one or two characteristics, subluxation is more commonly presented as a complex, multifaceted pathologic entity, known as the vertebral subluxation complex (VSC) (see Box 3-1). The VSC is a conceptual model and should not be confused with the vertebral subluxation syndrome. The vertebral subluxation/dysfunction syndrome defines a clinical disorder identified by its presenting symptoms and physical signs.
Gitelman, and later Faye, were the first to promote this broader model and its theoretic components.51,56,65,66 More recently, Lantz67 and Gatterman60,64 have championed this cause. In 1994, a consensus60 presented broader definitions for the VSC that seems to be growing in recognition and acceptance.
Although the trend toward a broader perspective of subluxation has helped move the profession from a simplistic and reductionistic model of spinal health, it has not necessarily advanced the investigation into its existence and nature. Reaching consensus on subluxation theory and expanding the number of clinical spinal disorders that are supposedly subluxation-related does not provide proof of their presence as the primary “lesion” treated by chiropractors. Faye suggests that the subluxation complex is a conceptualization for organizing the essential information relevant to treatment, allowing a chiropractor to examine a person in both a classic orthoneurologic manner and using a biomechanical approach to arrive at a double diagnosis.68 The first assesses the state of the pathologic tissue changes and also aids in determining the prognosis. The second determines the therapeutic procedures to be used and the treatment schedule.68
Nelson24 states that subluxation theory lacks several necessary properties that would allow it to serve as a vehicle for research. First, a theory should attempt to explain existing phenomena and observations; the VSC theory has not been used to explain any specific clinical phenomena. Lantz67 adds that the VSC does not identify any single event or process as the sole causative element in the complex process of subluxation development. Second, a theory should make predictions; the VSC theory makes none. It does not lead in any particular direction or draw any distinction or specific conclusions. The VSC theory suggests that any number of pathologic conditions affecting tissue are possible, with none being more important than any other.67 Third, a theory should be testable and falsifiable so that a study may provide results or observations that either confirm or refute the theory. The VSC theory is so encompassing, allowing for a wide range of mitigating and changing circumstances, that it is difficult to evaluate. Nelson24 points out that this circular type of argument and reasoning (tautology) validates itself simply by renaming accepted principles as a new theory or principle. A tautology has the virtue of being irrefutable, but the deficiency of being useless. It explains nothing, makes no predications, draws no distinctions, and is untestable.
There is value in reaching consensus on the theoretic pathophysiologic and pathomechanical components of functional disorders of spinal motion segments, but mainly for purposes of dialogue and research. The VSC therefore remains a theoretic model in need of investigation. The VSC theory should not be considered as one grand theory, but rather a series of interlocking and interdependent principles. The principles that form a basis for considering the existence and significance of the subluxation should be consistent with current basic science precepts. They must reflect current practice and educational standards, be clinically meaningful, and present a distinct and unique point of view. Unfortunately, the available research data tell us little about the presumed clinical meaningfulness of the traditional chiropractic lesion. Clinical meaningfulness refers to the practical value of a concept in directing the clinician to successful resolution of the health problem the patient has presented. Unfortunately, no one has systematically addressed the predictive power (if any) of subluxation correction for any specific disease or “condition.” None of the controlled clinical trials of the effects of spinal manipulative therapy has, to date, included a subluxation element.69,70
Keating and colleagues point out that the concept of chiropractic subluxation stands pretty much today as it did at the dawn of the 20th century: It is an interesting notion without validation.71 Although there is a strong intraprofessional commitment to the subluxation construct and there are reimbursement strategies that are legally based on subluxation, there is no scientific “gold standard” for detecting these clinical entities.72 The term chiropractic subluxation continues to have as much or more political than scientific meaning.73
Subluxation is still the most common term chiropractors use to describe the spinal joint disorders they treat.74 However, chiropractors are much more likely to view subluxations as disorders that have either structural or functional components rather than simply malpositioned joints. Furthermore, the VSC has been described using theoretic pathologic components broadly divided into mechanical, inflammatory-vascular, and neurobiologic categories. Although these divisions are modeled after those proposed by previous authors, they do not represent an established professional convention. Instead the categories and topics presented here represent an overview of the theoretic effects of the VSC and are not intended to be an all-inclusive or exhaustive treatise on the subject. While these categories are discussed separately, it must be emphasized that although these characteristics may occur in isolation, they can also occur in varying combinations. Some are emphasized more than others, depending on the mode of onset, rate of repair, and length of treatment time.
Mechanical components
The mechanical category of the VSC includes derangements or disorders of the somatic structures of the body that lead to altered joint structure and function. Derangement of the articular soft tissues and mechanical joint dysfunction may result from acute injury, repetitive-use injury, faulty posture or coordination, aging, immobilization, static overstress, congenital or developmental defects, or other primary disease states.*
Joint Malposition
Historically, the basis for subluxation was founded on the concept that traumatic events could lead to altered joint position and that this malposition would interfere with neurologic impulses. Both the chiropractic profession (through D.D. Palmer) and the osteopathic profession (through A.T. Still) have stressed joint position as an important quality for normal joint function.1,94
One of the oldest concepts from the literature on manipulation is the interdependence of structure and function. In other words, structure determines function and function determines structure. When there is a change in structure, there will be a change in function. Therefore, if a structural alteration is identified, a functional change should also be perceived. When a spinal joint is either acutely traumatized or undergoes chronic repetitive stresses, it is assumed that asymmetric muscle tension is likely to develop and hold the joint in a position away from its neutral alignment. The central idea is that misaligned positions of skeletal components can result in movement limitations, associated inflammatory changes, and irritation of nociceptors leading to pain. From a historical perspective, the chiropractic profession primarily viewed spinal subluxations as a structural failure that alters body function.95
The concept of static vertebral misalignment is difficult to support, however. Triano cites evidence that there is no “normal position” between vertebrae in the sense of the historic subluxation argument.95 The spine and the component parts are not perfectly symmetric in their development. Spinous processes in particular are quite prone to asymmetric growth. It is also very unlikely that one could palpate a displacement of a few millimeters or degrees based on the location of the spinous processes. Identification of joint malposition is typically through static palpation or radiographic mensuration. Both of these procedures have only fair to poor inter- and intraobserver agreement. Furthermore, there is no evidence that supports a change in alignment following manipulative intervention. Clearly the “bone-out-of-place” concept is not likely to be the sole explanation for subluxation.25,96
Joint Fixation (Hypomobility)
A more biologically plausible model of spinal joint pain incorporates abnormal joint mechanics and postulates that vertebral hypomobility can cause pain and abnormal spinal mechanics because of changes in sensory input from spinal and paraspinal tissues. Work by Henderson and associates provide the first preliminary anatomic evidence that altered spinal mechanics may produce neuroplastic changes in the dorsal horn of the spinal cord.97 98 99 Their preliminary data suggest that chronic vertebral hypomobility (fixation) at L4 through L6 in the rat affects synaptic density and morphology in the superficial dorsal horn of the L2 spinal cord level.99
Soft Tissue Injury and Repair
A commonly proposed source of joint fixation (hypomobility) and dysfunction is periarticular soft tissue injury with its resultant fibrosis and loss of elasticity and strength.15 16 17 18 19 20 21 2254,56,57,75 76 77 Soft tissue injury and fibrosis may result from acute or repetitive trauma to muscular, tendinous, myofascial, or ligamentous tissue. Regardless of the mechanism of injury, an ensuing inflammatory response is triggered57 resulting in extracellular accumulation of exudates and blood. Platelets then release thrombin-converting fibrinogen into fibrin, which organizes into collagenous scar tissue, resulting in a variety of soft tissue and articular adhesions. This process is considered to be nonspecific and often excessive in the case of traumatic NMS injuries.15,79 As a consequence, early conservative management is often directed at limiting the extent of the inflammatory response. Therapies directed at minimizing the extent of associated inflammatory exudates are helpful in reducing pain and muscle spasm and in promoting early pain-free mobilization and flexible repair.79,83 84 8593,100 101 102 103 104 105 106 107 108 109 110 111 112 113 Aggressive early care and mobilization provide the best opportunity for optimal healing and an early return to work for the patient. Bed rest and prolonged inactivity increase the chances of long-term disability and lost work time.103,105,114,115
The exudates that form as a byproduct of injury and inflammation set the stage for the next step in the process of connective tissue repair. They provide the matrix for the development of granulation tissue and scar formation. The formation of granulation tissue is predominantly carried out by the proliferation of fibroblasts and the synthesis and deposit of collagen tissue. The collagen is initially very poorly organized and must add additional collagen cross-linkages and reorganize along planes of stress to improve the tensile strength of the injured area. This process of repair and remodeling may take months and may result in less than optimal restoration and extensibility of the involved tissue. Immobilization slows the process of recovery, leading to loss of strength and flexibility and potential intra-articular fatty adhesions.75,76,83 84 85 86 87 88 89 90 91 92 93 Immobilization also leads to dehydration, causing proteoglycans to approximate and stick together.83,84,88 If injury or immobilization leads to decreased flexibility, therapies such as articular adjustments or joint mobilization should be directed toward the restoration of motion.15,79,82,102
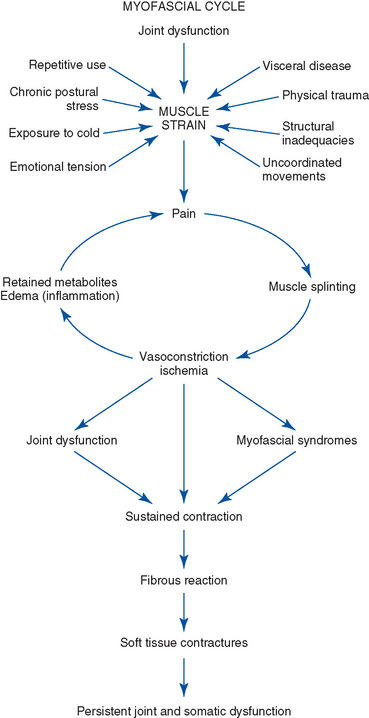
Myofascial Cycle
Painful conditions capable of triggering persistent muscle hypotoncity are additional sources of restricted joint motion (Figure 3-1). Muscle contraction, once initiated, may become a self-perpetuating source of pain and muscle hypotoncity.* Reactive splinting in the joint’s intrinsic muscles may further accentuate this process by blocking passive joint movement and the pain-inhibiting qualities of joint mechanoreceptor stimulation.120 Persistent contractions over time may develop into muscle contractures as a result of adaptational shortening and loss of elasticity from disuse or underuse. Although there is little direct evidence to support the belief that sustained muscle contraction is a feature of intervertebral dysfunction, the concept of protective muscle splinting appears plausible.121 Maladies capable of producing acute muscle contraction are wide ranging; they include trauma, structural inadequacies, visceral disease, emotional distress, and exposure to cold.122,123
Interarticular Derangements
A number of internal joint derangements have also been submitted as probable causes of joint locking and back pain. They include internal derangements of the intervertebral disc (IVD; intradiscal block), derangements of the posterior spinal joints (interarticular, intermeniscoid block),50,51,77,78,130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 and compressive buckling injuries.12,13 They are hypothesized to induce mechanical blockage to movement and unleveling of the motion segment, with resultant tension on the joint capsule, annulus, or both. The joint capsule and posterior annulus are pain-sensitive structures, and tension on these elements may induce additional painful muscle splinting, further accentuating the mechanical blockage and joint restriction. Mechanical joint dysfunction is therefore considered to be a significant and frequent cause of spinal pain and a potential source of spinal degeneration.
Interarticular Block
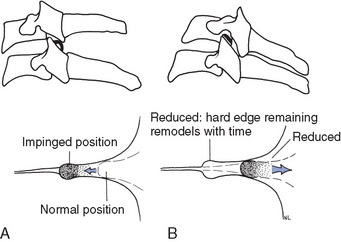
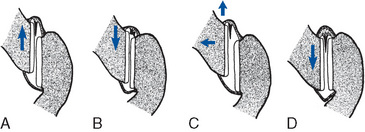
One source of derangement of the posterior joints is speculated to result from entrapment (Figure 3-2) or extrapment (Figure 3-3) of joint meniscoids or synovial folds.131 132 133 134 135 136 137 138 139 140 141 The intra-articular meniscoids are leaflike fibroadipose folds of synovium that are attached to the inner surface of the joint capsule and project into the joint cavity. These meniscoids have been found to be present in all of the posterior joints of the spine.
Bogduk and Jull140 have suggested that extrapment of these meniscoids may be one cause of restricted joint motion. They speculate that the meniscoid may occasionally be pulled out of its resting position by the inferior articular process of a zygapophyseal joint as it moves upward during flexion. On attempted extension, the inferior articular process returns toward its neutral position, but the meniscoid, instead of re-entering the joint cavity, impacts against the edge of the articular cartilage and buckles, representing a space-occupying lesion under the capsule. Pain occurs as a result of capsular tension, and extension motion is restricted. The use of a distractive or joint gapping adjustive procedure may function to separate the articular surfaces and release the extrapped meniscoid (see Figure 3-3). 140,147
Maigne78 and others77,116,137,148 149 150 151 152 have proposed a model of interapophysary meniscus entrapment rather than extrapment. In this model the menisci are purportedly drawn into a position between the joint margins during poorly coordinated spinal movements or sustained stressful postures. With resumption of normal postures, pain resulting from impaction of the menisci or traction of the articular capsule induces reactive muscle splinting and joint locking. The development of a painful myofascial cycle is initiated as prolonged muscle contraction leads to muscle fatigue, ischemia, and more pain. If spasm and locking persist, the articular cartilage may mold around the capsular meniscus, causing it to become more rigidly incarcerated within the joint.116 117 118 To interrupt the cycle of pain, muscle cramping, and joint locking, distractive adjustments have also been presented as a viable therapy capable of inducing joint separation, cavitation, and liberation of the entrapped menisci (see Figure 3-2).118 It is important to note that meniscoid derangement is only one hypothetical cause of joint dysfunction. Meniscoid derangement is postulated to be a more likely source of joint dysfunction in circumstances in which trivial trauma leads to acute joint irritation or locking and associated muscle spasm.139
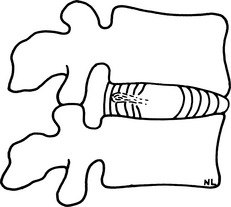
Interdiscal Block
The mechanical derangements of the IVD that may lead to joint dysfunction are postulated to result from pathophysiologic changes associated with aging, degenerative disc disease, and trauma. Farfan153 has proposed a model of progressive disc derangement based on repetitive rotational stress to the motion segment. He postulates that repetitive torsional loads of sufficient number and duration may, over time, lead to a fatigue injury in the outer annular fibers. The process would begin with circumferential distortion and separation in the outer annular fibers, followed by progression to radial fissuring and outward migration of nuclear material. Another view postulates that disc derangement, fissuring, and herniation begin in the innermost annular rings and progresses outward.154
The rate of fatigue and injury depends on the duration and magnitude of the force applied. In the individual with disrupted segmental biomechanics, the process is potentially accelerated as an altered axis of movement leads to increased rotational strain on the IVD. Postmortem dissection studies of degenerated discs have indeed identified radial fissures in the annulus fibrosus. Cyriax155 believes that displaced nuclear material along an incomplete fissure is the source of joint fixation. Nuclear migration along these radial fissures has also been demonstrated by computed tomography (CT) discography and correlated with patient pain.156
Interwoven in the natural history of degenerative disc disease may be episodes of acute mechanical back pain and joint locking. Maigne178 and others23,129 130 131 have postulated that incidents of blockage may occur during efforts of trunk flexion as nuclear fragments become lodged in fissures in the posterior annulus (interdiscal block) (Figure 3-4). Consequently, tension on the posterior annulus and other mobile elements of the involved motion segment are produced, initiating local muscle guarding and joint locking. Cyriax126 proposes that these lesions may induce tension on the dura mater, inducing lower back pain (LBP) and muscle splinting. Once local pain and muscle splinting are initiated, a self-perpetuating cycle of pain, cramping, and joint locking may result.
Adjustive therapy has been proposed as a viable treatment for interrupting this cycle of acute back pain and joint locking. In addition to the distractive effect on the posterior joints, adjustive therapy is thought to have a potential direct effect on the IVD, either by directing the fragmented nuclear material back toward a more central position or by forcing the nuclear fragment toward a less mechanically and neurologically insulting position (see Figures 4-18 and 4-19). Of course there are spinal joints (atlanto-occipital and atlantoaxial articulations) that do not have IVDs, and they are common sites of dysfunction. This clearly indicates that IVD derangement is not the sole source of spinal joint subluxation or dysfunction.
Compressive Buckling Injury
Triano suggests that a causal factor for a manipulable lesion may be a compressive buckling injury.12,13 Intersegmental buckling is likely the result of some error in neuromuscular control that fails either to provide adequate prestability to the segment or to respond appropriately with muscle activation to a perturbation.157 When a mechanical overload to spinal functional units occurs, either as a single traumatic event or cumulative events, a critical buckling load may be reached. Individual structural elements (disc, facet, ligament, nerve, muscle) may experience concentration of local stresses with reduced functional limits and symptom production specific to the tissue affected. The result is a state of dysfunction that may lead to local inflammatory or biomechanical changes.158,159
Each joint possesses some inherent stability resulting from the stiffness of the ligaments and joint capsule. Further stability and control are provided by the neuromuscular system and faulty motor control may lead to inappropriate levels of muscle force and stiffness at a given spinal segment. This may compromise segmental stability at that level,160 leading to transient intersegmental buckling.161 The segment briefly exceeds its safe physiologic motion, which leads to loading of the surrounding soft tissues (ligaments, IVD, etc.).157 Furthermore, exposure to vibration and previous disc injury may augment the buckling event. The result of intersegmental buckling is asymmetric positioning of the vertebra that is maintained by the intrinsic muscles producing hypomobility of the functional unit.
Clinical Joint Instability and Hypermobility
Joint dysfunction resulting from soft tissue injury or degeneration does not necessarily result in joint hypomobility. Disturbances of function of the vertebral column can also result from a loss of joint stability. Joint derangement and dysfunction resulting from a loss of joint stability are commonly referred to as joint hypermobility or clinical joint instability. Both terms are often used interchangeably, and there is no standard for defining these terms. Definitions vary among clinicians and authors and between the clinical and biomechanical literature.162,163
Although numerous definitions abound, all seem to incorporate a loss of stiffness or sensorimotor control affecting the joints’ stabilizing structures.162 163 164 165 The loss of stiffness is clinically relevant if excessive or aberrant movements lead to pain, progressive deformity, or compromised neurologic structures. Movement can be abnormal in quality (abnormal coupling) or in quantity (increased movement).
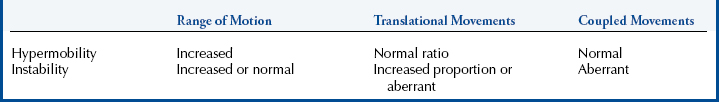
Attempts have been made to distinguish clinical joint instability from hypermobility (Table 3-1). The differences are a reflection of the structures involved and degree of pathologic change in the joints’ stabilizing structures. Hypermobile joints are assumed to be stable under normal physiologic loads. Hypermobile joints demonstrate increased segmental mobility, but they maintain normal patterns of movement. Hypermobility may be in one plane and not associated with any abnormal translational movements.166,167
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree