Small Joint Arthroscopy of the Foot
Keywords
• Arthroscopy • Small joints • Foot • First metatarsophalangeal joint
History
Arthroscopic treatment of the first metatarsophalangeal joint was first described by Wanatabe1 in 1972. Bartlett2 first reported its use in 1988. In 2006 Debnath and colleagues3 noted 95% of patients remaining pain-free at 2 years following first metatarsophalangeal joint (MTPJ) arthroscopy for treatment of early signs of degenerative joint disease. In 2008 Lui4 demonstrated a statistically significant correlation between joint cartilage erosion, joint synovitis, and pain in hallux valgus. He also noted a statistically significant correlation between the size of cartilage defect and severity of hallux valgus using diagnostic arthroscopy of the first MTPJ.4 In 2009 Wang and colleagues5 noted a statistically significant decrease in recurrence of acute gouty arthritis to the first MTPJ following arthroscopic debridement of tophi when compared with patients treated by medical means alone. Liu and colleagues6 has reported on performing arthroscopy on the great toe joint for hallux valgus deformity, with good results. These investigators evaluated 94 feet treated for hallux valgus deformity and felt that arthroscopy can be effective in improving both clinical and radiographic findings in patients with appropriate indications. These findings included a reducible first intermetatarsal angle and no significant deformity to the distal first metatarsal articular angle. Patients were treated with an endoscopic soft tissue release and medial exostectomy; proximal screw placement after manual manipulation was performed to close the intermetatarsal angle. An endoscopic approach to soft tissue release at the first MTPJ for treatment of hallux valgus has also been reported, with a significant increase in American Orthopaedic Foot and Ankle Society (AOFAS) score at greater than 2 years of follow up.6
The use of arthroscopic technology for small joints of the foot has not been limited to the diagnosis and treatment of first MTPJ pathology. Arthrodesis of the first metatarsocuneiform (MCJ) joint through a plantar-medial and dorsal-medial portal system has been recently described.7 In 2007 Lui8 presented a tarsometatarsal (Lisfranc) joint arthrodesis following a neglected fracture/dislocation through a 5-portal dorsal approach. Parisien and Vangsness9 first reported the arthroscopic approach to subtalar joint deformity in 1985, but the calcaneocuboid and talonavicular joint resection for triple arthrodesis by arthroscopic means was also demonstrated by Lui10 in 2006. In 2010 Bauer and colleagues11 reported the first case of calcaneonavicular coalition resection by endoscopic means, resulting in an AOFAS score of 82 at 2 years of follow up.
Anatomy
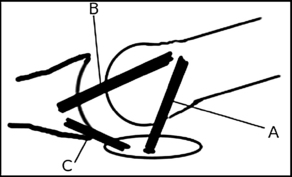
To properly perform arthroscopic procedures to the small joints of the foot, a firm understanding of the anatomy of these joints is required. In describing the first MTPJ complex, the base of the proximal phalanx of the hallux is ovoid in shape; wider than it is tall, concave both medial to lateral as well as dorsal to plantar. Little stability is gained from the chondroid nature of the first MTPJ, due to shallow surface for articulation between the phalanx and the metatarsal head.12 The rounded head of the first metatarsal has a side-to-side curvature that is greater than the vertical curvature and is somewhat wider (20–24 mm) than its height (16–20 mm).13 The articular surface, covered by hyaline cartilage, extends onto the dorsal aspect of the metatarsal head and continues plantarly into the medial and lateral grooves, which serve as articulations for the sesamoid bones, with the medial groove larger and deeper to accommodate for the larger tibial sesamoid. The plantar grooves are separated by a median crest, known as the crista.13 The joint capsule of the first MTPJ attaches close to cartilaginous edges dorsally; however, plantarly it attaches several millimeters proximal to the cartilage, with the plantar aspect of the capsule thicker than the dorsal capsule because of the presence of the plantar metatarsophalangeal ligament. The metatarsosesamoid ligaments thicken the medial and lateral aspects of the joint capsule, along with the medial and lateral collateral ligaments, which tract from the medial and lateral metatarsal tubercles to the corresponding tubercles on the sides of the phalanx (Fig. 1).13 The sesamoid bones of the flexor hallucis brevis muscle, which ossify between 10 and 12 years of age, are attached to the metatarsal via the metatarsosesamoidal ligaments and to the proximal phalanx of the hallux via the phalangeal-sesamoidal ligaments, respectively. The sesamoids also firmly adhere to the plantar metatarsophalangeal ligament, which results in a firm attachment to the proximal phalanx. The sesamoids therefore do not move relative to the proximal phalanx but relative to the metatarsal. Along with the ligamentous attachments already described, there are tendon attachments to the sesamoid bones as well. The tibial sesamoid provides an insertion point for the abductor hallucis, and the fibular sesamoid provides an insertion point for the adductor hallucis as well as the deep transverse metatarsal ligament. Contraction of the soft tissues that insert on the fibular sesamoid have been reported to contribute to the formation of hallux abducto valgus.14
The first MCJ is the largest of the tarsometatarsal joints. The outline of the facets of the first MCJ is reniform in shape with the hilus laterally. The articular surface of the base of the first metatarsal is 25 to 30 mm deep and 16 to 20 mm wide, and the surface is concave dorsally and flat or slightly convex in the more plantar aspect of the joint.15 The corresponding dorsal part of the distal aspect of the medial cuneiform is slightly convex, with the plantar aspect flat or slightly concave, allowing for inversion and eversion along the long axis of the metatarsal.
The midtarsal joint comprises the talonavicular joint (TNJ) and the calcaneocuboid joint (CCJ). The TNJ is condylar in nature while the CCJ is a saddle joint. These joints cannot act independently, as motion in the subtalar joint (STJ) and CCJ is required for motion at the TNJ. The head of the talus is convex in all directions and bears at least 3 recognizable articular areas: an ovoid area for articulation with the navicular, a triangular facet for the plantar calcaneonavicular ligament, and a long oval area plantarly for the anterior calcaneal articular facet. The posterior surface of the navicular is ovoid in shape, broader laterally than medially; the articular surface is concave and wholly articular with the head of the talus. The talonavicular ligament is a wide, thin band that connects the superior surface of the talar neck to the dorsal surface of the navicular. The calcaneonavicular ligament component of the bifurcate ligament also serves to provide medial support to the calcaneocuboid joint and lateral support to the TNJ. The anterior surface of the calcaneus is shaped roughly like an inverted triangle. The articular surface is concave from superior to inferior and convex transversely, giving the characteristic saddle shape. The posterior surface of the cuboid has a saddle shape corresponding to the anterior surface of the calcaneus.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree